Diagnosing and Treating an Unpleasant Scalp Smell
Every now and then, a patient reports that they have a problem with scalp odour. The story typically goes that their scalp smells bad and no matter what they do, they just can’t get rid of the smell. The specific issue goes by a variety of names, although the most common names are smelly scalp syndrome (SSS) and smelly hair syndrome (SHS).
What causes SSS?
There is no one cause of smelly hair syndrome. There are many causes. The first thing that I tell my patients is that I need to use my eyes and ears to help determine the cause - use of my nose actually plays little role.
Step 1: Hear the Story
To start with, I need to hear their story. I need to understand when the odor started and what things in the patient’s life changed around this time. I also need to understand several other issues including:
Were any new medications started?
Were any new hair products started?
Any new hair dyes started?
Were any new shampoos started?
How often does the patient shampoo?
What shampoos are used?
Did a child in the house start school?
Is their a new pet in the house?
Were any new hobbies started?
Is it just the scalp odor or does odour come from the body (armpits/groin?)
Has their been any changes in the patients health?
Are their any dental concerns?
Does the scalp itch?
Is their burning in the scalp?
Is the scalp tender?
Is their hair loss accompanying the odor ... or just odor?
Does the patient wake up with blood or secretions on the pillow?
Has the patient’s level of fatigue changed?
What is the patient’s stress level?
Has the patient travelled?
Has the patient’s diet changed?
Does the patient report any skin rashes?
Is their any concerns regarding sexually transmitted diseases?
Step 2: See the Scalp
After getting a sense about the patient’s story, I need to see the scalp, eyebrows, eyelashes and body hair. I also need to see the nails and may even examine parts of the skin.
The scalp examination is important to determine if there are any abnormalities in the skin of the scalp and/or the hair follicles themselves. It is important to determine if there is redness, scale, pustules (pimples), openings in the skin, sores, breakdown. Of course, determining whether or not the smell is actually associated with hair loss is critically important.
Causes of SSS
There are many potential cause of SSS. The most common causes include:
- Seborrheic dermatitis
- Psoriasis
- Fungal Infections
- Allergic contact dermatitis
- Irritant contact dermatitis
- Scarring Alopecias
- Apocrine/Eccrine Gland Overactivity
- Metabolic Disturbances
- Infections
- Skin Cancers
- Hormonal disorders
- Infrequent Washing
Tests for SSS
For individuals with smelly scalp, there are no specific tests per se. However, a number of tests may be performed including:
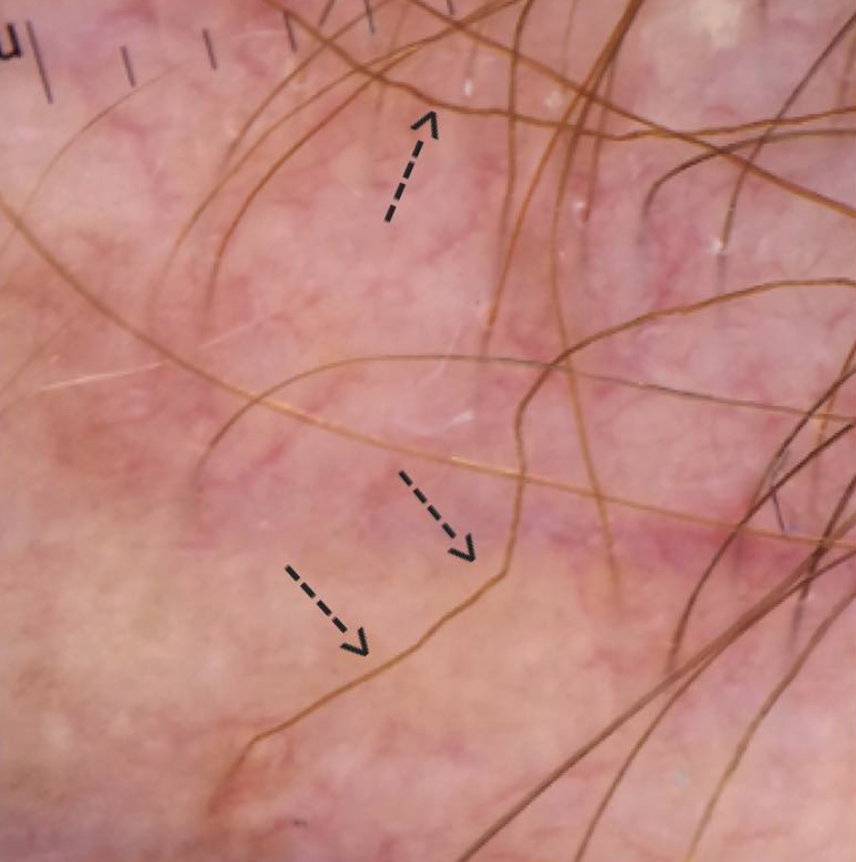
1. Dermoscopy
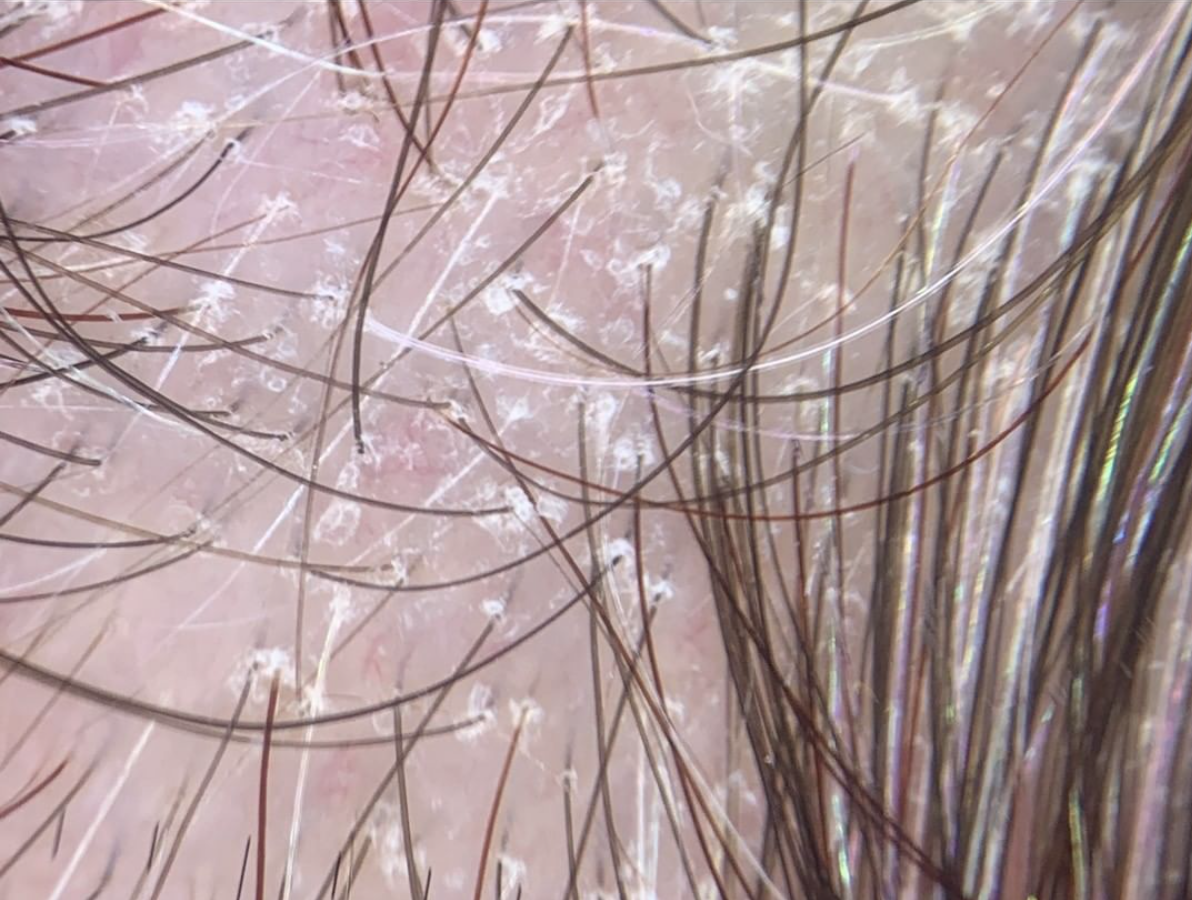
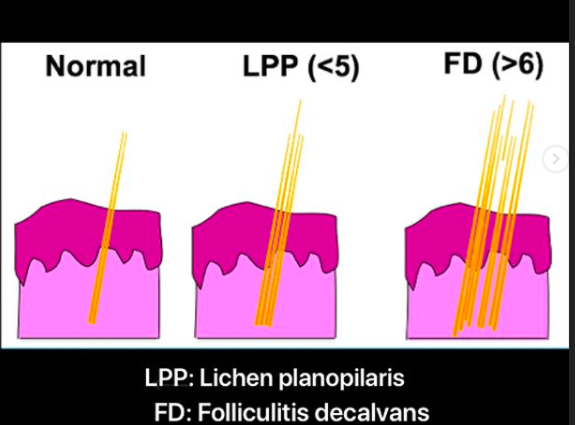
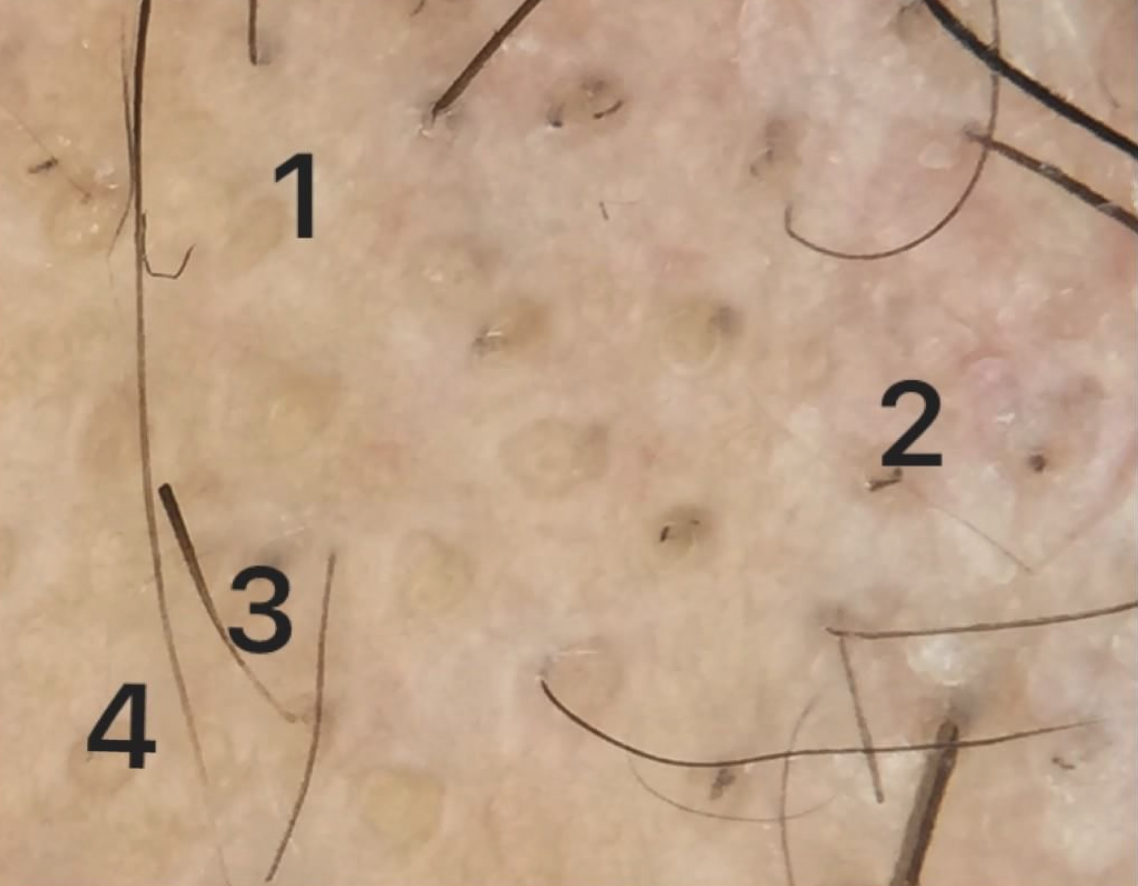
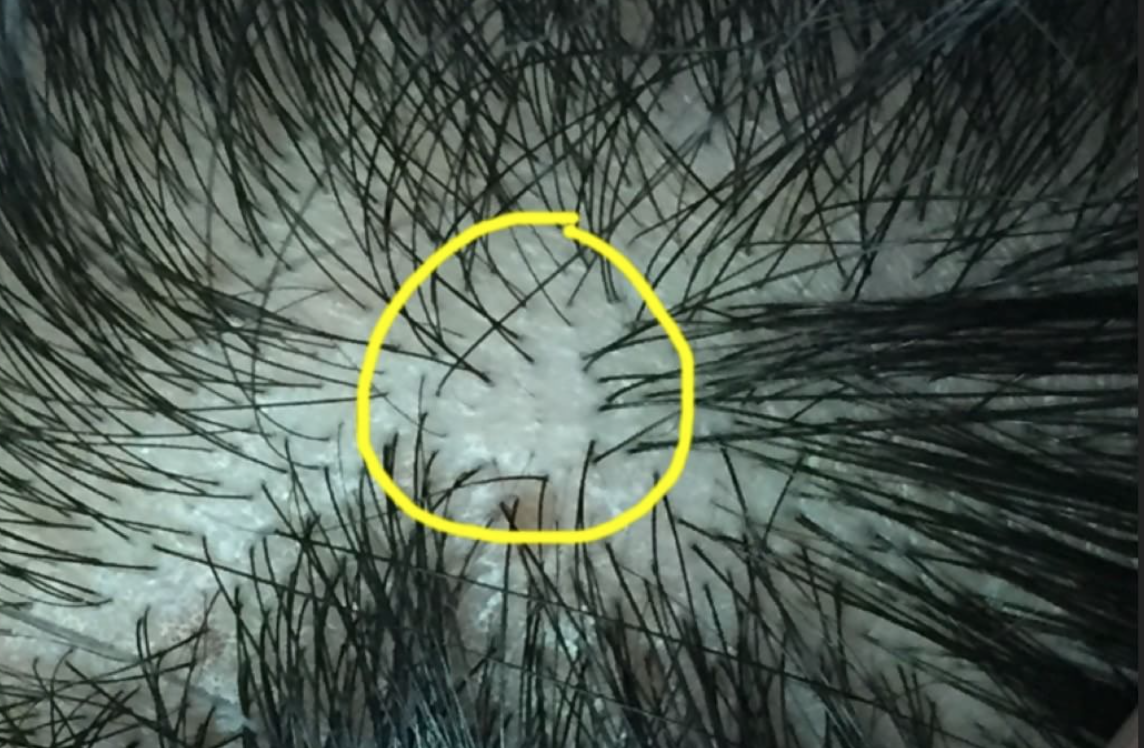
Dermoscopy is a technique that involves examination of the hair and scalp with a specialized instrument known as a dermatoscope. Dermoscopy can help physicians identify special features that point to a specific disease including seborrheic dermatitis, psoriasis, tinea capitis, scarring alopecias, folliculitis.
2. Swabs of Pustules
Any pustules on the scalp need to be swabbed. The presence of yellow pustules does not necessarily mean their is an infection in the follicle, but careful assessment is needed. A swab will help not only to identify bacteria that might be present on the scalp but also to determine the precise antibiotics that kill those bacteria. This information is helpful if a decision is made at any point to treat.
3. Skin scrapings
Skin scrapings are important if a diagnosis of tinea capitis (scalp ringworm) is being considered. The scrapings can be examined under the microscope using a standard KOH preparation or sent off to a laboratory for analysis.
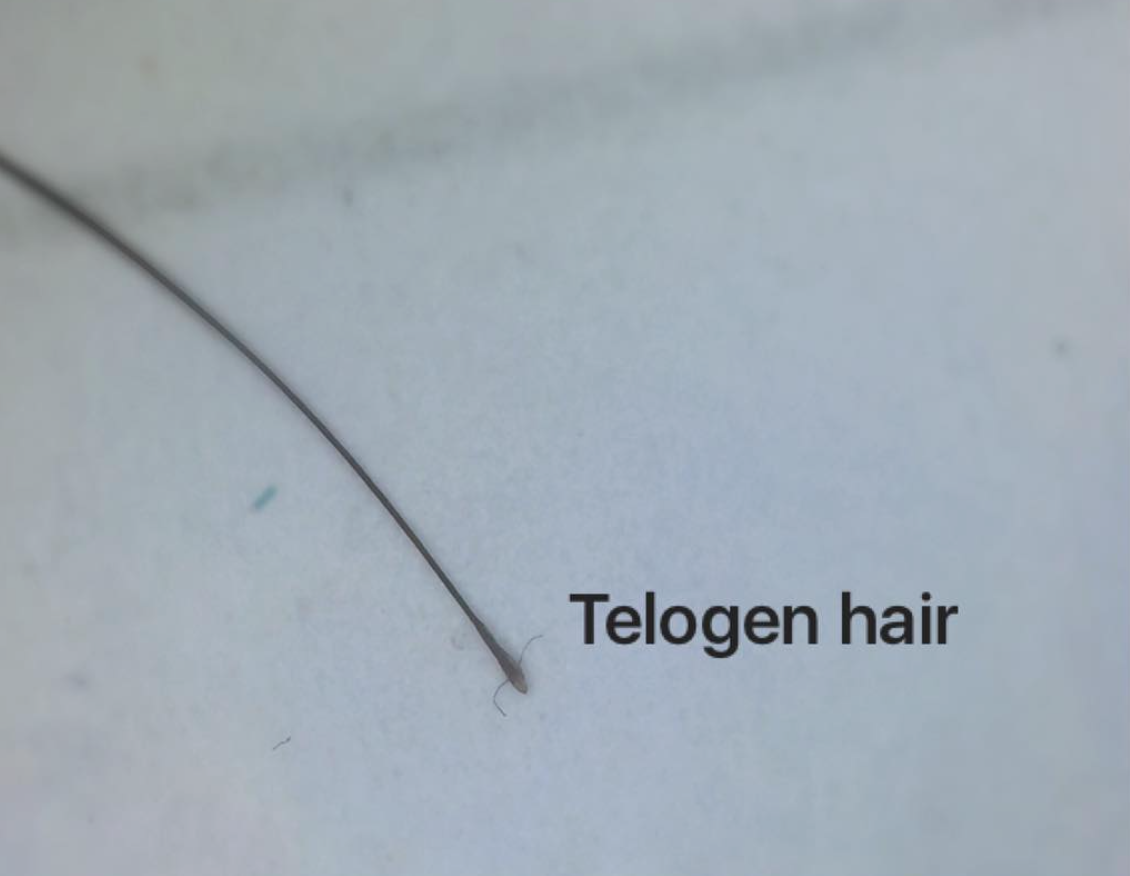
4. Examination of Hairs
Hairs themselves should be analyzed. A gentle pull of hairs may reveal secretions and crusts attached to hairs. These should be examined for bacteria and fungi as in the paragraph above.
5. Scalp Punch Biopsy
A scalp biopsy is rarely needed for patients with smelly scalp syndrome but should always be considered. Patients with scalp odor who have concerns about severe burning or pain or who have concerns about bleeding, weeping or oozing are most likely to benefit from a biopsy.
6. Blood Tests
Blood tests are usually normal in patients with scalp odor. However there are situations where I will consider blood tests for blood sugars, thyroid disease and hormone abnormalities.
7. Patch Testing
Patch testing is a method of determining whether a patient has a true allergy. It’s a very involved test and not appropriate for everyone but may be appropriate for a minority of patients with SSS who have marked scalp itching and tenderness especially those with rashes elsewhere on the body.
Treating SSS
The best treatment for SSS is to treat the underlying cause - if it can be identified. If the odor is coming from a scarring alopecia (like dissecting cellulitis) treatment for this condition is what is needed. If the smell is coming from a weeping skin cancer, the only definitive way to get rid of the smell is to treat that cancer. In other words, treatment for scalp odor is first and foremost centred around trying to lock in a diagnosis.
One needs to keep in mind that a cause is not always readily apparent. In such cases a variety of approaches can be taken.
Treatments to Consider When No Cause Can be Found.
In cases where the precise cause can not be identified, my general approach is to target scalp fungi, bacteria and inflammation. As I often say to physicians who visit with me in my clinic a helpful “memory tool” to treat scalp smell is to remember that dealing with challenging cases of scalp smell requires us to call in “smelly undercover FBI agents on a daily basis to deal with the slippery cover up.”
This 'memory tool' reminds us we need to
a) uncover any scale
b) kill bacteria (letter B in FBI)
c) kill fungi (letter F in FBI)
d) reduce inflammation (letter I in FBI)
e) shampoo daily
f) slippery (reduce oils)
f) cover up any smell
The three letter FBI acronym stands for agents that target fungi (letter F), bacteria (letter B) and inflammation (letter I)
A variety of approaches are possible and there is no one treatment approach that fixed everything. But with a logical approach we can often combat challenging cases of scalp smell.
I generally start patients with a once daily to twice daily shampooing regimen which includes antibacterial cleansers alternating with ketoconazole shampoos and alternating with a sulphur shampoo containing salicylic acid. These are done in 3 day cycles (see below) amd are left on the scalp for three minutes each application. Depending on the specific situation, the patient may use a topical clindamycin/corticosteroid solution at night for a few weeks.
Initial Starting Routine:
Day 1 morning: Antibacterial cleanser 3 min
After morning shampoo: apply 3 drops peppermint oil in jojoba to scalp
Day 1 evening: Clindamycin/steroid solution
Day 2 morning: Ketoconazole shampoo 3 min
After morning shampoo: apply 3 drops peppermint oil in jojoba to scalp
After morning shampoo: apply 3 drops peppermint oil in jojoba to scalp
Day 2 evening: Clindamycin/steroid solution
Day 3 morning: Sulphur/SA shampoo
After morning shampoo: apply 3 drops peppermint oil in jojoba to scalp
Day 3 evening: Clindamycin/steroid solution
Repeat cycle...
Let’s look at each of these steps in a bit more detail.
1. Uncover
In many of these smelly scalp syndromes, it is important to get rid of any scale or crust that might be harbouring bacteria. For this reason, I frequently recommend use of a shampoo containing salicylic acid. Salicylic acid helps remove scale. There are many ways to bring salicylic acid into a treatment program but shampoos are frequently the easiest. Neutrogena T sal is a common sulphur based shampoo which contains salicylic acid. Many patients with SHS like both components, but particularly the sulphur component.
2. Fungi
Yeast are a common culprit in scalp smell for many patients. Yeast known as Malassezia are thought to be the key underlying cause of seborrheic dermatitis. Any patient with scalp smell needs to eradicate yeast as a fundamental step in treatment. Ketoconazole is a good first step in eradicating yeast in patients with SSS. However other options can be considered including
a) zinc pyrithione shampoo
b) ciclopirox shampoo
c) selenium sulphide
d) oral itraconazole
e) tea tree oil shampoo
f) 1 teaspoon tea tree oil in 1 cup water
3. Bacteria
Bacterial load on the scalp should be reduced as part of a basic regimen to stop scalp smell. Antibacterial soaps containing triclosan were common antibacterial agents we used in the past. These are less commonly used given the ban on triclosan in many countries. However, I am a fan of antibacterial washes for smelly scalp syndrome -including harsh ones. Normally, we don't use soaps on the scalp as they tend to be harsh and tend to leave a residue. In many patients with SSS/SHS, this actually proves beneficial.
The use of antibacterial agents should be left on for 3 minutes.
Depending on the patient, bacterial load can also be controlled with
a) Topical clindamycin
b) Topical or oral metronidazole (Flagyl)
c) Oral doxycycline
d) Benzoyl peroxide body washes (10%) used as scalp cleanser
e) topical chlorhexidine 2-4 % applied with wash cloth (must be kept out of eyes and ears)
e) topical triclosan and phisohex - no longer used.
4. Inflammation
Inflammation in the skin of the scalp can change the types of oils that are produced and the types of free fatty acids that are released. In the early weeks of treating scalp smell, I recommend use of a mid potency topical steroid such as topical betamethasone valerate to help reduce inflammation. This can be used nightly with topical clindamycin compounded into it.
5. Reducing oils
A variety of options are available if it is discovered that the patient is producing too much oil. One can first see if shampoos like ketoconazole shampoo discussed above can help dry things out. The other option is to use various dry shampoos throughout the day. These can be washed out at night with one of the shampoos discussed above so that the clindamycin/betamethasone can be applied.
In rare cases, scalp smell can be improved by drastically and dramatically affecting the size of the oil glands with oral medications such as isotretinoin. In patients with bacterial scalp issues, reduction in oil glands makes bacteria less likely to remain on the scalp - a second benefit.
6. Cover up
There are a variety of other options to cover up smell. Use of essential oils such as peppermint oil, rosemary or lavender can be applied to the scalp. 3 drops of peppermint oil for every teaspoon of jojoba oil is a great start. This can be applied after the morning shampoo.
Rinses with baking soda help some. 1 teaspoon of baking soda is added to 1 cup of water along with a few drops rosemary. This is allowed to sit on the scalp 20 minutes.
For others, mixing 1/4 cup apple cider vinegar 3/4 cup water with 10 drops rosemary essential oil and 1/8 cup lemon juice forms a tonic than can be left on the scalp 30-40 minutes before rinsing off
Conclusion
Managing scalp door can be challenging. Too often it is forgotten that the fundamental step in treating scalp door is to treat the underlying cause of the door. That may require an examination by a dermatologist to determine that. The use of suphur based shampoos with salicylic acid together with various antibacterial washes and anti-seborrheic shampoos is a good starting point. More advanced options should be discussed with a dermatologist including use of isotretinoin or metronidazole.