Do birth control pills cause alopecia areata? Can they be used to treat alopecia areata?
Alopecia areata is an autoimmune conditions that is not uncommon in the population. In fact, about 1 in 50 women will develop alopecia areata and usually before 30. Oral contractive use is also common in women 18-40 years of age with 15-18 % of women in this age group using birth control. Given these relatively high frequency of alopecia areata and birth control there will be individuals who will develop alopecia areata fairly close in time to the start of an oral contraceptive pill. The question then arises :
Did starting the birth control pill cause the alopecia areata?
50 years of wondering
The question as to whether or not oral contraceptives can trigger a patch of alopecia areata has been with us since oral contraceptives first came to market. In fact, oral contraceptives were first FDA approved in 1960. Reports questioning whether a possible connection could exist between alopecia areata and oral contraceptives surfaced in 1965 with studies published in the British Medical Journal in an article "Alopecia areata and Oral Contraceptives".
No good evidence
For most people, there is no good evidence that alopecia areata is triggered by oral contraceptives. That does not rule out the possibility that there are a proportion of individuals who do have this as a trigger - but for the most part medical studies can't conclusively pinpoint a link.
Oral contraceptive and Autoimmune diseases
A compressive review by Willams in 2017 examined whether there was any link between hormonal type contraceptives and any of the known autoimmune diseases. The article indicated that ere was in fact substantial evidence exists linking the use of combined oral contraceptives to an increase in multiple sclerosis, ulcerative colitis, Crohn's disease, Systemic Lupus Erythematosus, and interstitial cystitis. Oral contraceptives were associated with a lower incidence of hyperthyroidism. Alopecia areata was not on this list.
Alopecia areata and estrogen
We do know that the inflammation that is seen in alopecia areata can be influenced in some manner by estrogen. One study has suggested that alopecia areata can actually be treated with a combination of oral contraceptives (especially those containing norethindrone) and metformin.
Reisz et al 2013
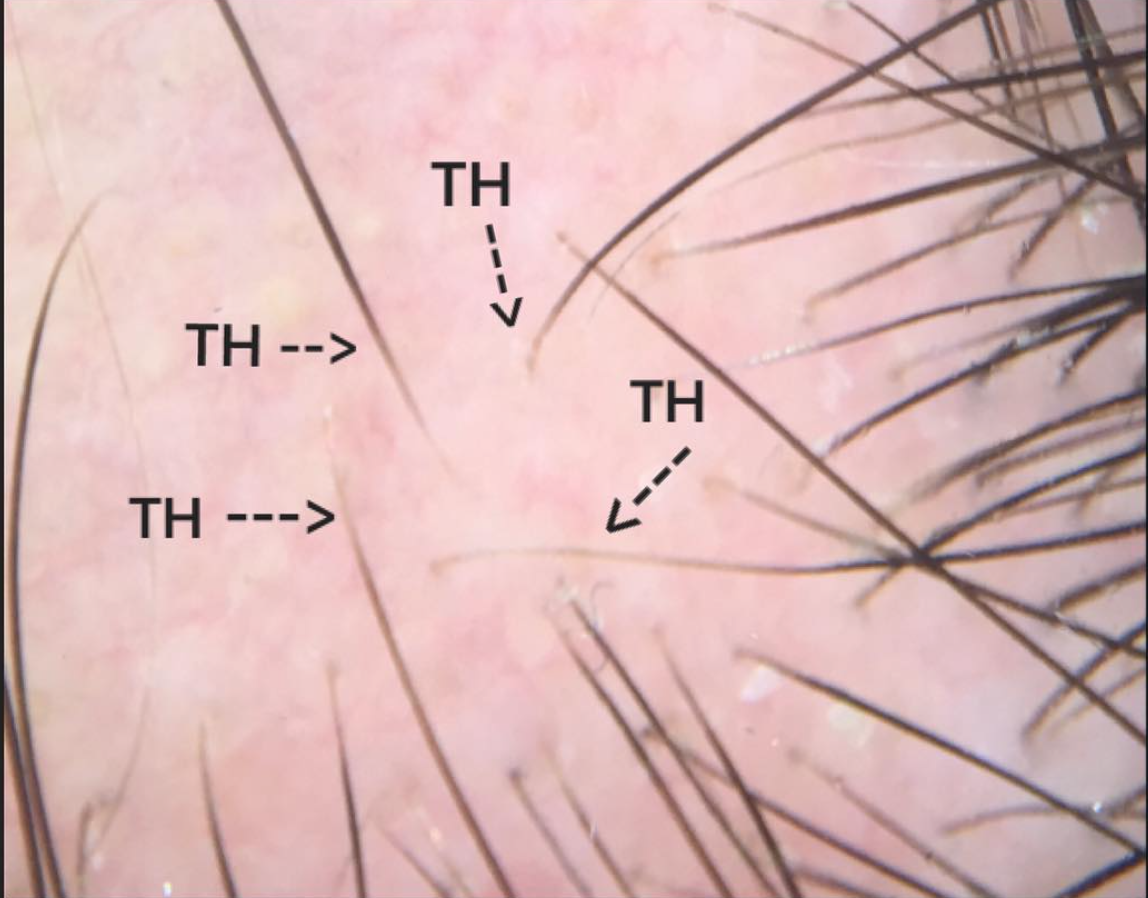
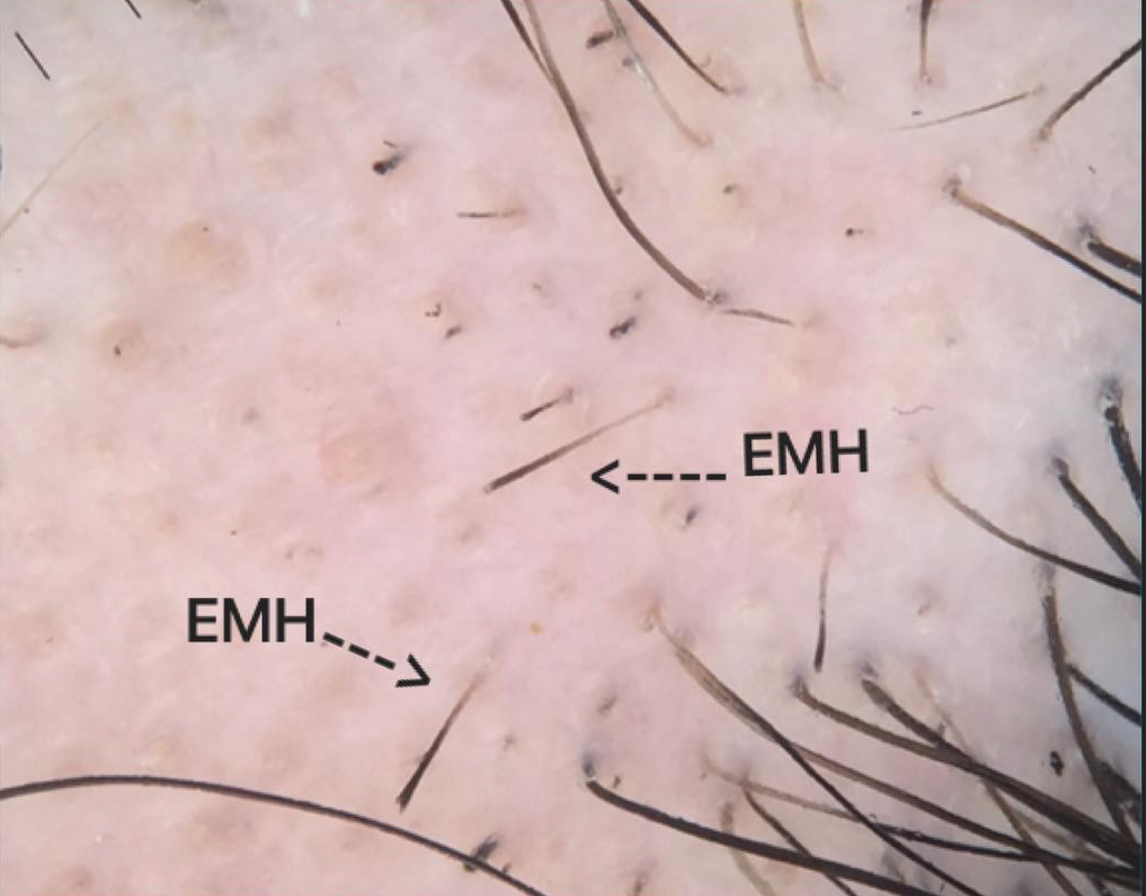
In 2013, Dr Colleen Reisz from Kansas City evaluated the benefits of one or a combination of birth control pills, metformin and vitamin D in treating alopecia areata. She noted in the background leading up to the study that women of reproductive age experience variation in hormones like estrogens during different phases of the menstrual cycle. What is so relevant to this study – and alopecia areata in general is that these changes in hormone levels during the menstrual cycle are accompanied by changes in immune function. Dr Reisz wished to better understand how medical interventions that reduce hormone production and lower aromatase behavior can help alopecia areata. The authors evaluated 14 patients with alopecia areata. 13 had recent hair loss within the past 1 year. About 50 % had moderate to severe hair loss at baseline.
The patients were then offered norethindrone containing oral contraceptive pills (1/20 or 1.5/30) or metformin (500-850mg/day) or both, along with vitamin D (1000-2000IU/day). There were four patients treated with metformin, 9 with metformin and birth control and one with birth control. Some patients (N=5) requested intralesional corticosteroids along with hormonal therapy
Seven of the 14 (50%) had complete regrowth of hair within 3 months of treatment. Another 4 patients regrew their hair fully but the time to reach that state of full regrowth was much longer (about 1 year or more). Of the four other patients, 2 continued to have hair loss, one converted from minor degrees of alopecia to complete hair loss in one week. One patient did not respond at all.
Norethindrone containing oral contraceptives
The following oral contraceptives may contain norethindrone and ethinyl estradiol:
Norethindrone & Ethinyl Estradiol Containing OCPs
CONCLUSION
It's clear that estrogen affect the immune system and at least for some immune based diseases (like multiple sclerosis, ulcerative colitis, Crohn's disease, Systemic Lupus Erythematosus, and interstitial cystitis) there is good evidence that oral contraceptive use increases the risk of developing these conditions.
We don't have good evidence yet for alopecia areata and to date it would appear for the vast majority of patients there is no link. However, this does not exclude a small subset of individuals that in fact develop alopecia areata after starting a birth control pill. Detailed studies have not examined this and whether there are certain types of birth control pills that are protective against AA and some that are contributory. The study by Reisz and colleagues discussed above would certainly cause us to give pause and consider that some oral contraceptives may actually be helpful. For my patients who clearly feel that their OCP is a trigger, I may consider stopping if the alopecia areata is not responding to treatment as one might expect. If an oral contraceptive is restarted in the future, a different one might be considered with close monitoring of whether the OCP gives a flare of the alopecia areata.
REFERENCES
1) Williams WV. Hormonal contraception and the development of autoimmunity: A review of the literature. Linacre Q. 2017.
2) Oral contraceptives and alopecia. 1968 Mar 9; 1(5592): 593.
3) Oral contraceptives and alopecia areata. Br Med J. 1965 Oct 23; 2(5468): 1005.
4) Wallace ML, et al. Estrogen and progesterone receptors in androgenic alopecia versus alopecia areata. Am J Dermatopathol. 1998.
5) Reisz, CM. “Reinstitution of Immune Privilege in Alopecia Areata: norethindrone and metformin” International Journal of Immunology 2013