Fibromyalgia as a Cause of Scalp Dysesethesia
The “scalp dysesthesias” are a group of conditions whereby the patient has various types of symptoms in the scalp despite the scalp looking fairly normal. In other words, these are a group of disorders characterized by chronic cutaneous symptoms without objective findings. Patients complain of burning, stinging, or itching, which is often triggered or exacerbated by psychological or physical stress.
RECENT RELATED ARTICLES ON SCALP DYSESTHESIA
Scalp Exercises for the Scalp Dysesthesias
Approach to the Treatment of Scalp Dysesthesias
Scalp Dysestheisas: Misunderstood, Misdiagnosed and Poorly Managed
What causes scalp burning?
Drug-Free Options to Reduce Scalp Symptoms
Witch Hazel: What is it?
Scalp Dysesthesia Among Patients with Fibromyalgia
Breathing Exercises for Scalp Dysesthesias
Fibromyalgia and the Scalp
For anyone with scalp symptoms, a full examination is needed to determine the cause. Some are related to common conditions like seborrheic dermatitis, psoriasis, and other common dermatologic issues. However, sometimes the symptoms are due to a scalp “dysesthesia.” Symptoms from a dysesthesia can include burning, pain, itching, brushing, shoot pains and throbbing. The difference between a dysesthesia and a non-dysesthesia is that usually the scalp appears fairly normal in a dysesthesia and there is not much in the way or redness, scale, and other inflammatory systems
There are many causes to consider in patients with underlying scalp dysesthesia. Cervical spine disease and underlying depression/anxiety have received some attention in the research world. However, there are many causes to consider. The first of course is to ensure that the cause of the scalp symptoms are truly a dysesthesia and not some other explainable cause.
Today, we’ll spend time talking a bit about fibromyalgia as a potential cause of scalp dysesthesia. Fibromyalgia is a chronic pain disorder with a well-defined clinical phenotype which affects about 2-4 % of people in the United States. The condition has several key features including widespread pain and tenderness, high levels of sleep disturbance, fatigue, cognitive dysfunction and emotional distress. Research over the past decade has shown that abnormal processing of pain and other sensory input occurs in the brain, spinal cord and periphery and is related to the processes of central and peripheral sensitization. As such, fibromyalgia is deemed to be one of the central sensitivity syndromes.
Neurogenic Inflammation in Fibromyalgia
The method by which nerve signals communicate appear to be disturbed in fibromyalgia. We now know that the brain and spinal cord don’t process information about pain sensations in a normal manner. Patients with fibromyalgia often feel pain. Stimuli that might not be painful to most people are interpreted by the brain of someone with fibromyalgia as painful. For example, a scalp massage might be considered painful by someone with fibromyalgia.
A special type of inflammation known as “neurogenic inflammation” may contribute to the symptoms that patients with fibromyalgia experience. For example, there is now evidence of neurogenically-derived inflammatory mechanisms occurring in the peripheral tissues, spinal cord and brain in fibromyalgia. Neuropeptides, chemokines and cytokines are proposed to be the chemicals that drive this inflammation and are postulated to be the activators of both the innate and adaptive immune systems. This contributes to the clinical features of fibromyalgia, such as swelling and dysesthesia, and may influence central symptoms, such as fatigue and changes in cognition. In turn, emotional and stress-related physiological mechanisms are seen as upstream drivers of ‘neurogenic inflammation’ in fibromyalgia.
Scalp Dysesthesia in Fibromyalgia
Individuals with fibromyalgia commonly experience a variety of scalp symptoms including itching, burning, pain, throbbing, shooting pains. For some it hurts to lay down on a pillow, brush the hair or even shampoo the scalp. These types of symptoms are much more common in fibromyalgia than we realized. Unfortunately, the symptoms are often ignored by the medical community or incorrectly diagnosed as dandruff, seborrheic dermatitis. All too common the symptoms are attributed to anxiety or depression.
Despite being so common, scalp findings and symptoms in patients with fibromyalgia have not received much attention or study in the medical literature. We don’t really have a good understanding of the types of symptoms patients with fibromyalgia experience. Some of the pain has been attributed to the tightening of scalp muscles, but I think this is far too simplistic of a view. Now that we understand more about neurogenic inflammation in fibromyalgia it becomes clear that these cytokines, chemokine and neuropeptides are likely to be directly responsible for creating the pain, itching, and burning in fibromyalgia. A variety of other pain syndromes may be associated with the same neurogenic inflammation - including such entities as chronic fatigue syndrome. Many such entities have associated scalp conditions but have been poorly studied and documented.
Treatment of Scalp Symptoms in Fibromyalgia
A variety of treatment options are available to address the scalp symptoms that occur in patients with fibromyalgia. The first of course is to determine precisely the cause. If the cause of scalp symptoms in a person with fibromyalgia is simply dandruff or seborrheic dermatitis and not related to a dysesthesia, then treating the dandruff or seborrheic dermatitis is what is needed. Patients with fibromyalgia still have the same set of conditions that anyone can have - it’s just that there is a whole set of conditions and considerations that can be different.
If symptoms are truly arising from a scalp dysesthesia, it’s important for the physician treating the scalp symptoms to work closely with the rheumatologist to formulate a plan for treating the scalp symptoms. When I work with patients who have scalp symptoms due to nerve related issues, I generally correspond with the main fibromyalgia treating team.
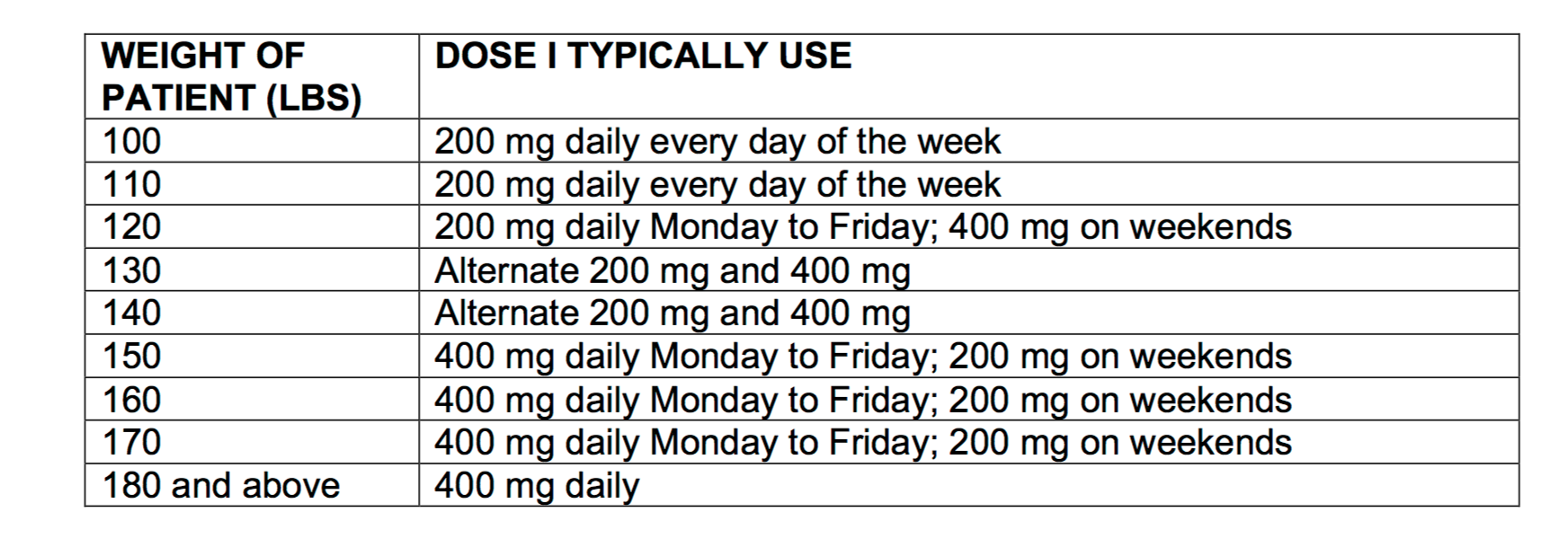
Daily exercise and improving sleep as much as possible can help many people. Meditation techniques are helpful for some. There are hundreds of different types of meditation that are possible and there is no right or wrong way. Some of my patients with scalp pain simply find that turning on the TV helps take their mind off the symptoms (other patients of mind with fibromyalgia find the noise and light of the TV bothersome altogether so there is no one type of answer). Yoga, tai chi, prayer help many others. A variety of medications can be considered including gabapentin, Lyrica, and amitriptyline. Low dose naltrexone at 1.5 to 4.5 mg helps some patients with fibromyalgia-related scalp symptoms. Topical TKAL is proving helpful for some but not all individuals with fibromyalgia as sometimes rubbing creams into the scalp causes pain. We are also studying the role of N-acetyl cysteine.
A variety of non-pharmacological options are available including apple cider vinegar rinses, use of witch hazel and use of essential oils. Ice packs and frozen peas placed on the scalp or neck provide relief to many patients. Cool water placed on scalp also helps many as well.
scalp physiotherapy, neck massage, breathing exercises and daily exercise are also important.
Summary
A variety of scalp symptoms may be experienced by patients with fibromyalgia. A full examination is needed to determine the cause. Some are related to common conditions like seborrheic dermatitis, psoriasis, and other common dermatologic issues. However, sometimes the symptoms are due to a scalp dysesthesia.
Symptoms from a dysesthesia can include burning, pain, itching, brushing, shoot pains and throbbing. The difference between a dysesthesia and a non-dysesthesia is that usually the scalp appears fairly normal in a dysesthesia and there is not much in the way or redness, scale, and other inflammatory systems. These types of symptoms are poorly understood. Unfortunately they are all too often dismissed by health care providers or attributed to other reasons. Treating is challenging but a multifaceted approach often provides some degree of help.