This is an in important question and one that needs good data. I serve as the chair of a committee of the International Society of Hair Restoration Surgery. On Friday we sent out a survey to hair transplant surgeons around the world with the hopes of gathering more information on the successes and failures surgeons have had when transplanting scarring alopecias.
There is no doubt that hair transplantation works wonderfully in some patients with scarring alopecia and does not work well in others. One must always have quiet (inactive) disease for at least 1-2 years before a transplant is attempted.
What are the criteria for transplanting scarring alopecia?
In general, a scarring alopecia must be quiet for 1-2 years before a transplant can be even considered. Several years ago I put forth criteria for determining if an individual with lichen planopilaris is a hair transplant candidate:
Criteria for Hair Transplantation Candidacy in LPP
1. The PATIENT should be off medications.
Ideally the patient should be off all topical, oral and injection medications to truly know that the disease is burnt out and ‘inactive’. However, in RARE cases, it may be possible to perform a transplant in someone using medications AND who meets criteria 2, 3 and 4 below. This should only be done on a case by case basis and in rare circumstances as the risk for disease reactivation is high. A patient using medications to suppress disease activity is at high risk for reactivation following hair transplant surgery. It is a last resort in a well-informed patient.
2. The PATIENT must not report symptoms related to the LPP in the past 12 months, (and ideally 24 months).
The patient must have no significant itching, burning or pain. One must always keep in mind that the absence of symptoms does not prove the disease is quiet but the presence of symptoms certainly raises suspicion the disease could be active. Even the periodic development of itching or burning from time to time could indicate the disease has triggers that cause a flare and that the patient is not a candidate for surgery. The patient who dabs a bit of clobetasol now and then on the scalp to control a bit of itching may also have disease that is not completely quiet.
3. The PHYSICIAN must make note of no clinical evidence of active LPP in the past 12 months, (and ideally 24 months).
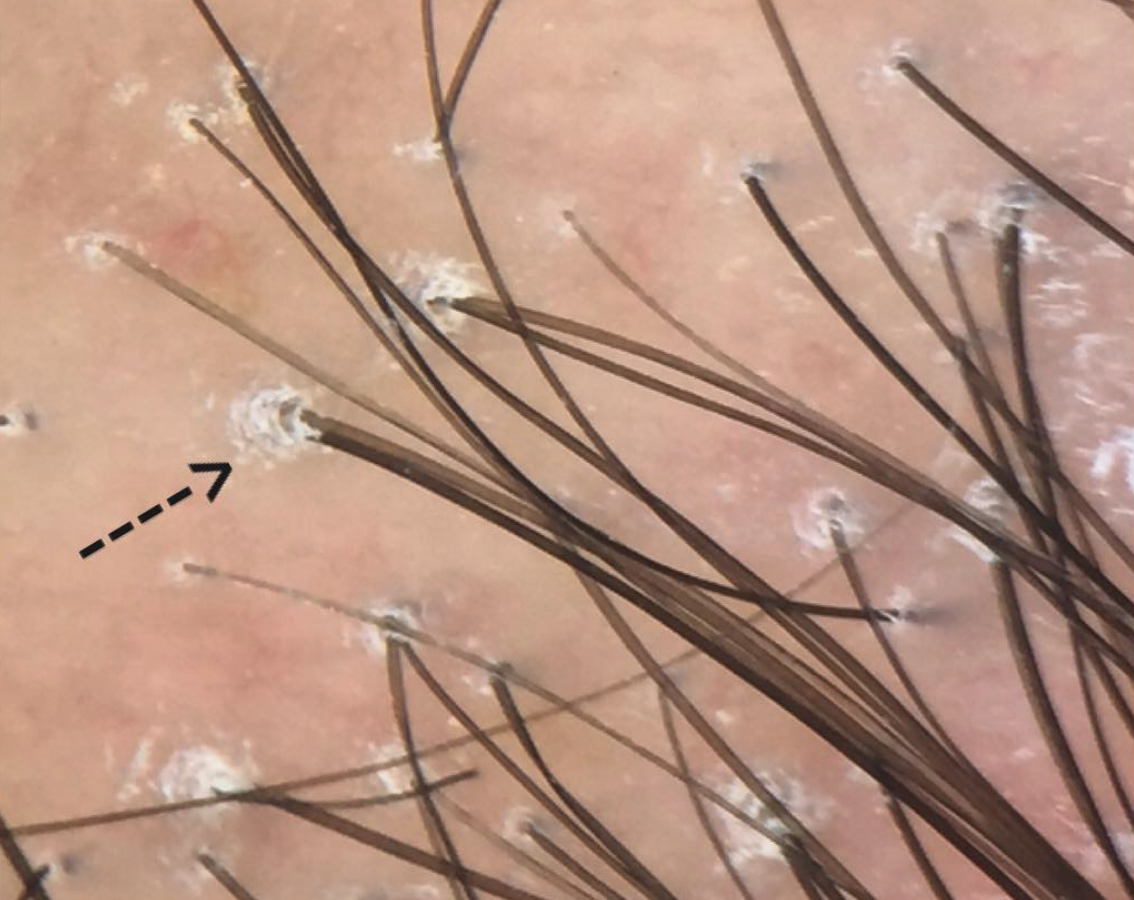
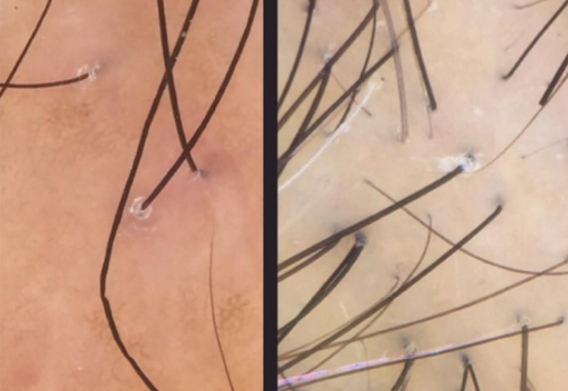
There must be no scalp clinical evidence of active LPP such as perifollicular erythema, perifollicular scale (follicular hyperkeratosis). In addition, the pull test must be negative.
4. Both the PATIENT and PHYSICIAN must show no evidence of ongoing hair loss over the past 12 months (and ideally 24 months).
There must be no further hair loss over a period of 24 months of monitoring off the previous hair loss treatment medications. This general includes the patient and physician's perception that there has been no further loss as well as serial photographs every 6-12 months showing no changes. As discussed above, the 12 month waiting time is the standard of care as an accepted definition for hair transplant candidacy.
5. The patient must have sufficient donor hair for the transplant.
Not all patients with LPP maintain sufficient donor hair even if the disease has become quiet.
Disease Reactivation Following Surgery
My research has focused on the chances of reactivation of LPP after surgery. It is important to be aware that ANY patient with LPP is at risk for reactivation or a 'flare' of their LPP after surgery. The risk, I estimate, is as follows:
LPP Reactivation Risk (Donovan, J, unpublished data)
i) A patient with active LPP before their transplant is nearly guaranteed to have a flare of his or her LPP if a hair transplant is done. (estimate 90-100 % chance of flare within 2 years post transplant)
ii) A patient with partially active LPP before their transplant is very likely to have a flare if a hair transplant is done. (estimate 70-90 % chance of flare within 2 years post transplant)
iii) A patient with medication induced inactive LPP before their transplant has a moderate chance of a flare if a hair transplant is done (estimate 50-70 % chance of flare within 2 years post transplant)
iv) A patient with inactive LPP off all medications for 1 year before their transplant has a low chance of a flare if a hair transplant is done (estimate 10-25 % chance of flare within 2 years post transplant)
v) A patient with inactive LPP off all medications for 2 years before their transplant has a low but definite chance of a flare if a hair transplant is done (estimate less than 10% chance of flare within 2 years post transplant)