Lichen planopilaris or Pseudopelade of Brocq: Does anyone care?
Lichen Planopilaris and Pseudopelade of Brocq are Different Conditions with the Same Treatment.
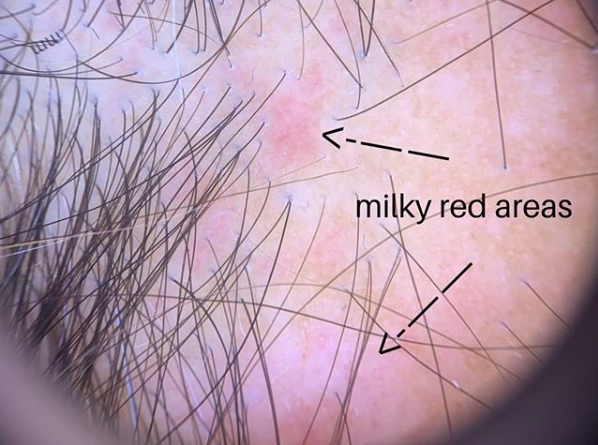
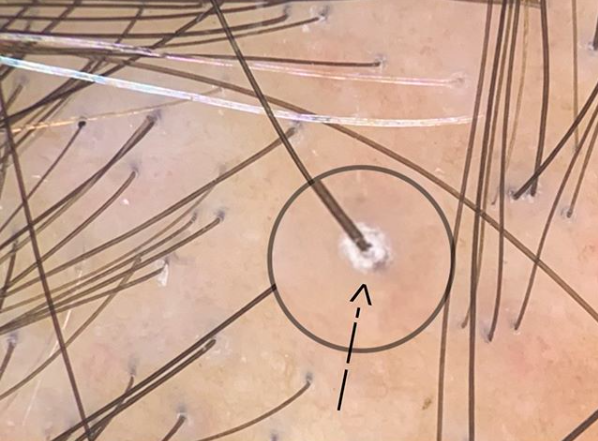
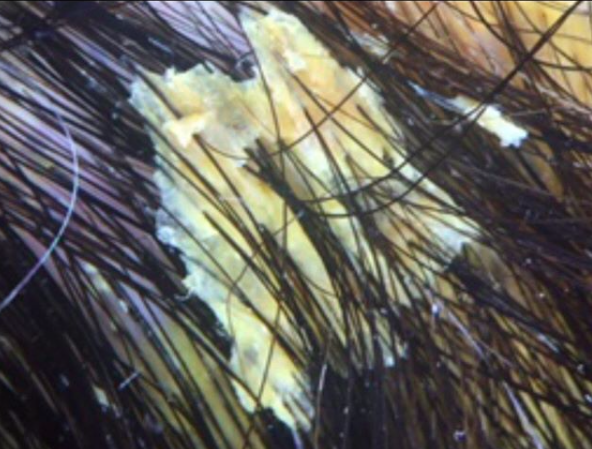
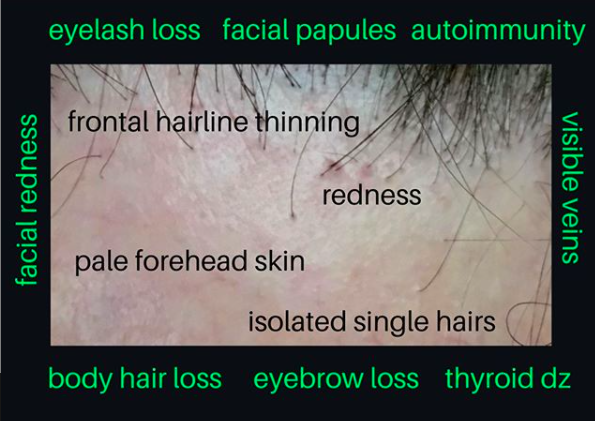
Lichen plaopilaris and pseudopelade are both types of scarring alopecia. They can look similar - but there are many unique differences as well too. Patients with lichen planopilaris often present with scalp itching and burning and the central area of the scalp is typically affected. Increased scalp shedding is common in the early stages. Other areas can be affected too. Some patients have other areas affected as well including eyebrows, and eyelashes. Some patients have oral, nail and vaginal lichen planus but this is present only in a small proportion. Examination of the scalp in a patient with LPP shows redness in the scalp and redness around hairs. There is often scaling and flaking in the scalp as well with scaling notably seen around the hairs in active disease (perifollicular scale).
Pseudopelade of Brocq: A type of primary lymphocytic scarring alopecia
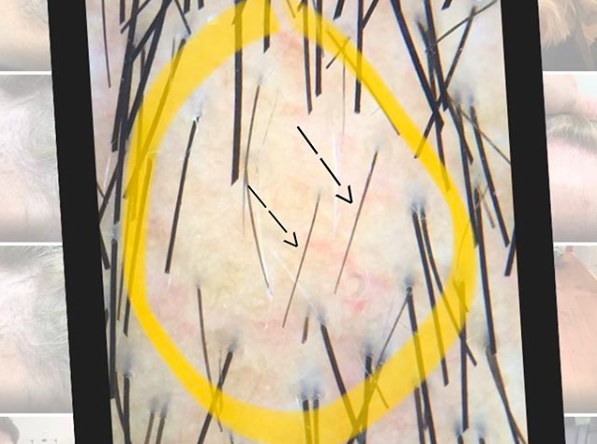
Pseudopelade is a scarring alopecia which also presents with itching and burning. The scalp is often pink in color although may be surprisingly normal in appearance despite the ongoing loss of hair. Patients with PPB often have circular or oval areas of hair loss with strikingly close resemblance to alopecia areata. In fact, pelade is the french word used for alopecia areata. Pseudopelade is different than LPP because it typically lacks the thick perifolliuclar scale seen in LPP and often has more skin atrophy. The skin dips downs with tiny depressions which are referred to as “foot prints in the snow.”
So is it LPP or PPB?
I’ve been part of countless numbers of discussions over the years with patients, physicians, and dermatology trainees as to whether the patient in question has lichen planoplaris of pseudopelade. There is often a great intensity of discussion around the subject. In formal dermatology rounds, physician can debate for extensive amounts of time as if the true answer will be found at the end of the spirited battle.
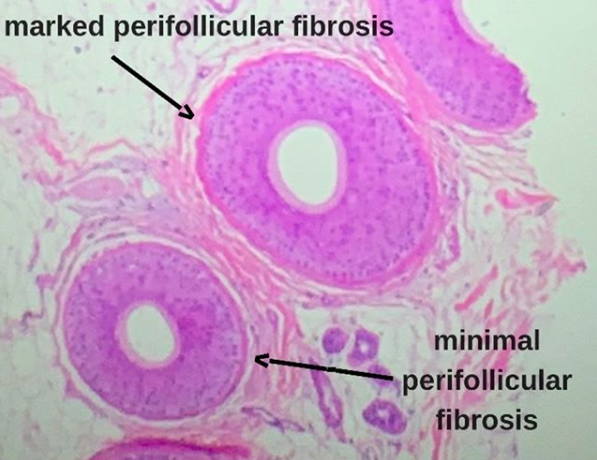
The reality is that PPB and LPP are distinct conditions. Microarray studies from 2010 showed this clearly. PPB is not just a type of LPP. Generally speaking the less scale and redness around hairs and the more atrophic the skin is - the more likely PPB will be given as a diagnosis. There are histological features too that differentiate these conditions - with PP typically showing a preserved elastic fiber network whereas LPP typically shows a destroyed elastic fiber network. Some physicians and reserachers even feel that PPB is so different from LPP that it should not even be called a scarring alopecia but rather should be called a permanent non scarring alopecia. This is subject to ongoing debate.
LPP or PPB: Leaving our Patients Confused
The active debate that physicians like to have between PPB and LPP often leaves patients confused. Discussions often go something like this;
“I went to see Dr. X and he said I don’t have Pseudopelade of Brocq and what I have is actually LPP”
“I went to see Dr. X and he said what I have is LPP”
Ending the Absurdity: Using the Term “Primary Lymphocytic Scarring Alopecia”
Sometimes, I refuse to use the terms PPB and LPP. These are usually patients with massive files and patients who have seen many physicians to date. These are the patients where 5 doctors have said LPP and 5 doctors have said PPB. These are the patients who are not getting better and what to know two things 1) What is the proper diagnosis and 2) what is the best treatment?
Many physicians fail to recogniize that there is not one LPP and there is not one PPB. It’s not a matter of selecting the right answer. There are probably 20 different presentations of LPP and 5-10 presentations of LPP. Debating over whether a patient has LPP or PPB is good for academic purposes and teaching and good for understanding potential treatments. But at the end of the day, what the patient in front of us has is a scarring alopecia that is caused in part by inflammatory cells called lymphocytes doing things they should not be doing.
In the present day, the treatments for PPB and LPP are the same!! The question that must be asked is what is the purpose of so much extensive debate when the treatments in the present day are the same. Topical steroids, steroid injections, doxycycline, retinoids, hydroxychloroquine, methotrexate are among the options. Physicians far too often spend far too long debating and one upping other colleagues with an attempt to present to the patient what they think the diagnosis is that we forget that the treatments for LPP and PPB are generally the same.
One can argue on an on as to the relevant merits of honing down the diagnosis. Knowing that a patient has LPP prompts one to ask about lichen planus of other areas. But nail, mucosal, vaginal symptoms should be asked of all our patients. Knowing that a patient has LPP might prompt one to screen for certain blood tests including thyroid abnormalities. But these same tests are still appropriate in a patient with presumed PPB.
Conclusion
As a clinician, it is helpful to practice in a manner that strives for accuracy. Accurate diagnosis are fundamental to practicing good medicine. But there are times where we can not always make accurate diagnoses because not everything is always so clear cut. In the case of LPP, and PPB there are classic presentations of these diseases and there are aytpical or non-classical presentations of these diseases. We should strive to recognize the classical cases and strive in these cases to give them the proper names (either LPP or PPB). However, there are other times were the efforts that go into pigeon holing our patients into certain disease categories only serves to remove us further from focusing on actually providing care to the patient. There are dozens of variants of LPP not one. There are many variants of PPB not one.
The term “primary lymphocytic scarring alopecia” serves us well in cases where pigeon holing and efforts to force a diagnosis just doesn’t work.
Reference
Yu M et al. Lichen planopilaris and pseudopelade of Brocq involve distinct disease associated gene expression patterns by microarray. J Dermatol Sci. 2010 Jan;57(1):27-36.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.