Symmetry and Hair Loss: Which types of hair loss tend to be more symmetrical?
Symmetry and Hair Loss: Which patterns of hair loss are often symmetrical?
They say that nothing in nature is truly symmetrical. But clearly some objects come fairly close. We immediately recognize that there are some planes or axes of symmetry in this plant. In other words, you can draw several lines whereby the right side looks pretty similar to the left side.
Symmetry is something I pay attention to when it comes to hair loss. Many hair loss conditions have what is know as sagittal symmetry- meaning that if you draw a line directly up from the nose through the forehead and back to the back of the scalp you’d find that the hair loss affecting the right side is more or less a mirror image to the left side.
Several of the so called non scarring alopecias have some degree of “sagittal symmetry.” The right side typically looks like the left side. Androgenetic alopecia and telogen effluvium mostly have sagittal symmetry. I use the word “mostly” because even these conditions are not perfectly symmetrical. For example, some males notice one temple recedes faster on one side than the other side (often the right recedes faster than the left). The one non scarring condition that rarely shows sagittal symmetry (unless it is more advanced) is the autoimmune disease alopecia areata. In fact, what makes alopecia areata so unqiue is the random areas it affects the scalp. Symmetry is not usually a part of alopecia areata (except in forms like AA totalis, universalis, ophiasis, diffusa, etc). A circle of alopecia on the left is rarely even matched by a circle of alopecia on the right. Last week I saw a patient who came with a presumed diagnosis of alopecia areata. One sideburn was missing on the right and one side burn was missing on the left. The tip off here for me that something was wrong with the previous diagnosis was the alopecia areata is not usually so symmetrical. The correct diagnosis for this patient turned out to be frontal fibrosing alopecia.
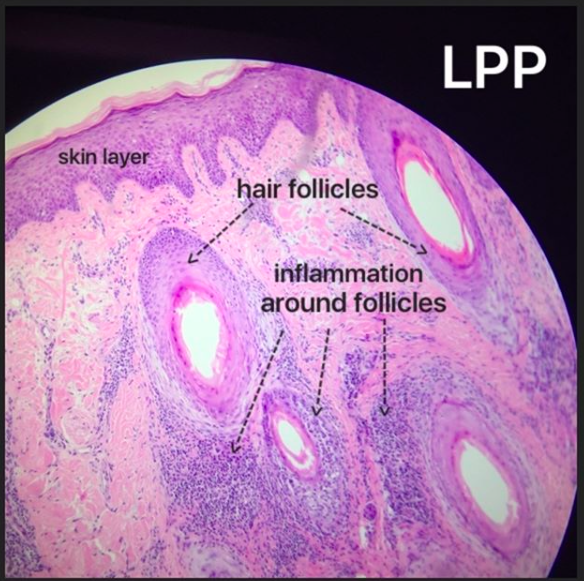
Most scarring alopecias are not so symmetrical. Lichen planopilaris is less symmetrical than pseudopelade. Dissecting cellulitis tends to be less symmetrical than folliculitis decalvans. Frontal fibrosing alopecia often has some degree of sagittal symmetry but of course not perfectly.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.