QUESTION
Hi Dr Donovan,
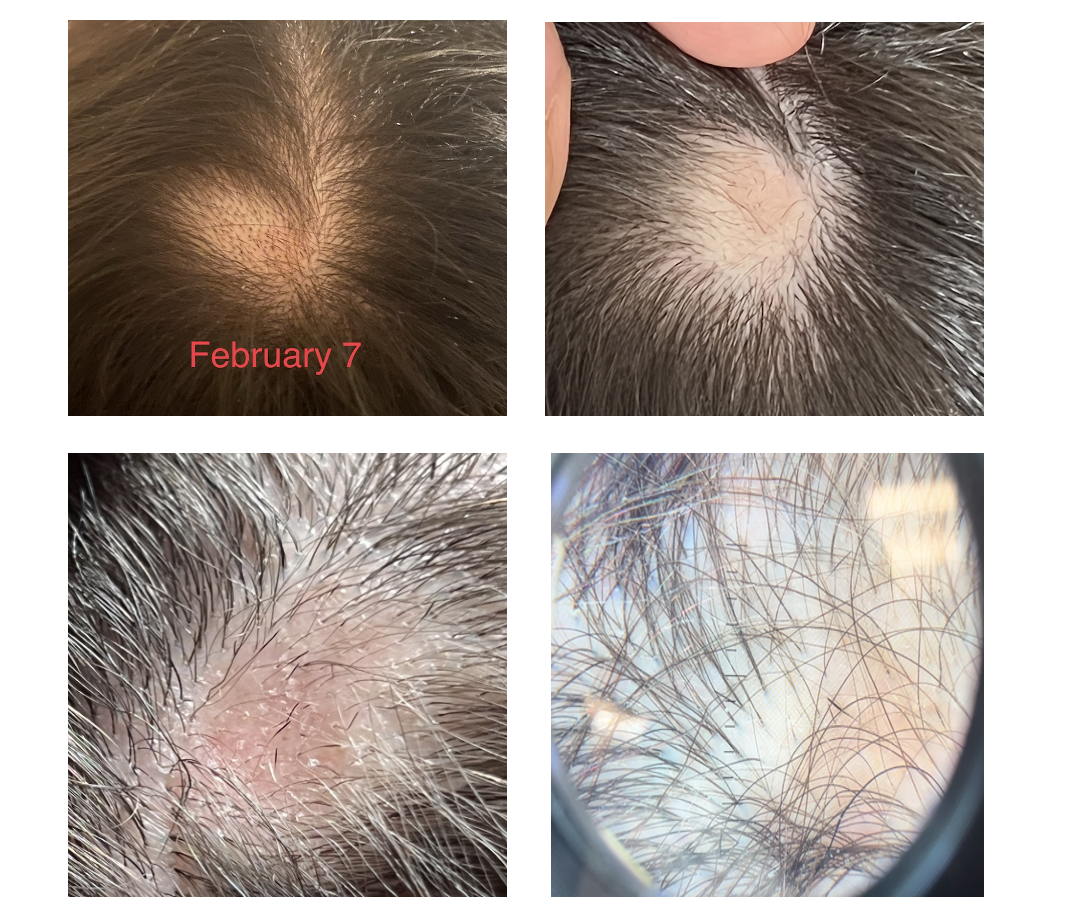
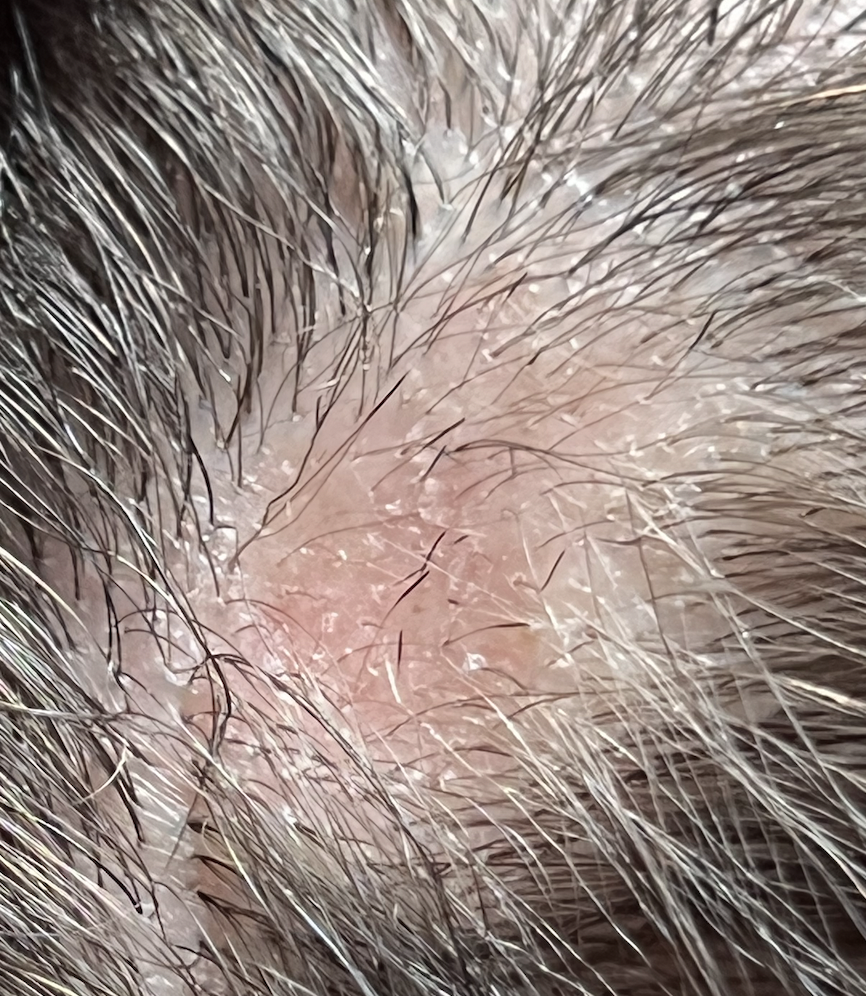
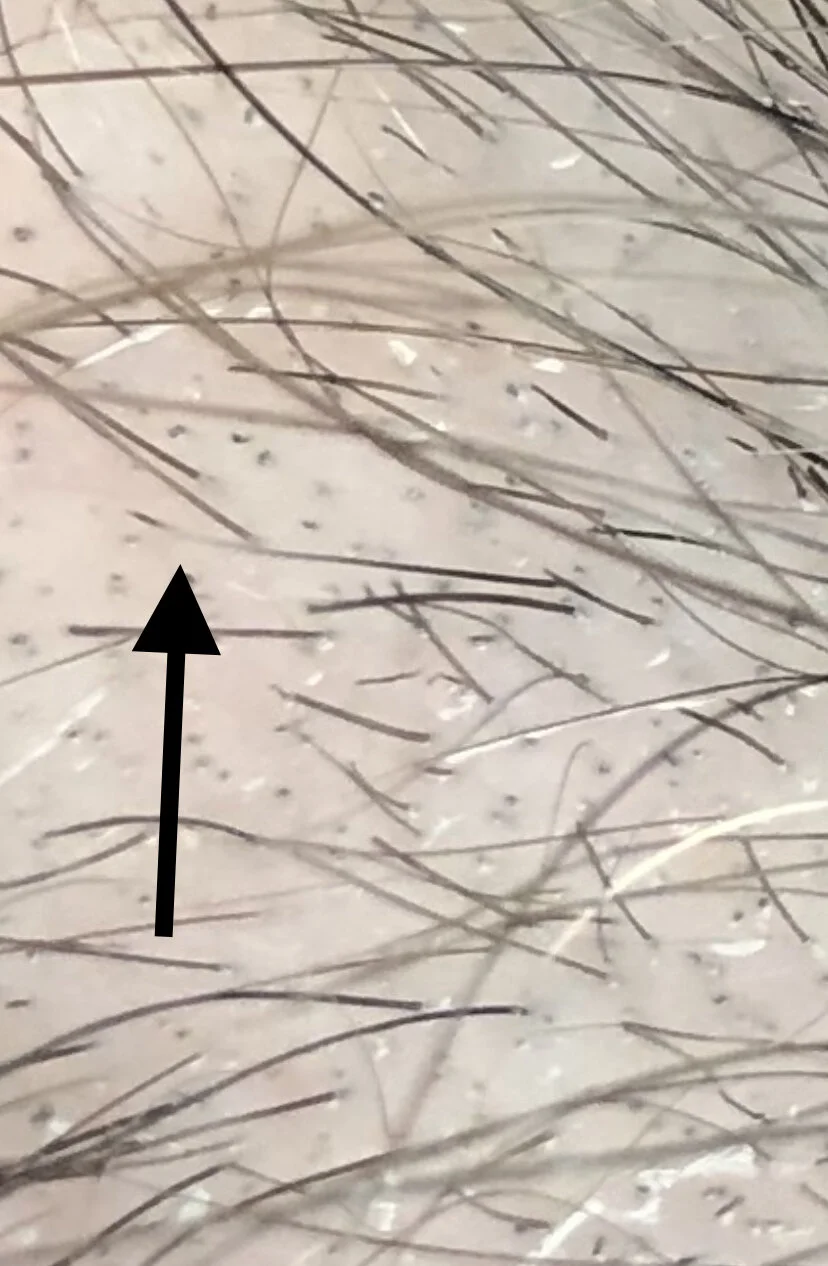
I am a 29 year old female and developed alopecia areata in late January 2021. I first developed a patch at the top of the scalp on Jan 23rd and then a second at the back of the scalp on Feb 8. They have fortunately both now grown back with steroid injections using Kenalog.
I am trying to understand this condition and what might have caused it. There is nobody in my family with this condition so I am perplexed. I am quite healthy, eat well and exercise 5 days per week. I have mild asthma and take puffers only very rarely. I developed a urinary tract infection in December and was treated with the antibiotic trimethoprim/sulfamethoxazole (Septra). I’ve been wondering if this could be the cause.
I have been researching if medications can cause alopecia areata but I’m not sure that medications are really all that commonly implicated.
Can you tell me if some medications are strongly connected with developing alopecia areata?
ANSWER
Thanks for submitting your question.
The short answer is no. Mediations are not really all that strongly connected with developing alopecia areata. That’s not to say that some medications have not been linked - it’s just the chances are very low and the vast majority of medications are not strongly associated with development of alopecia areata.
To date, there have only been about 25 patients reported in the medical journals with suspected drug induced alopecia areata. Could it be that there are more? Absolutely. But one thing is likely that drugs are probably not all that commonly connected with alopecia areata.
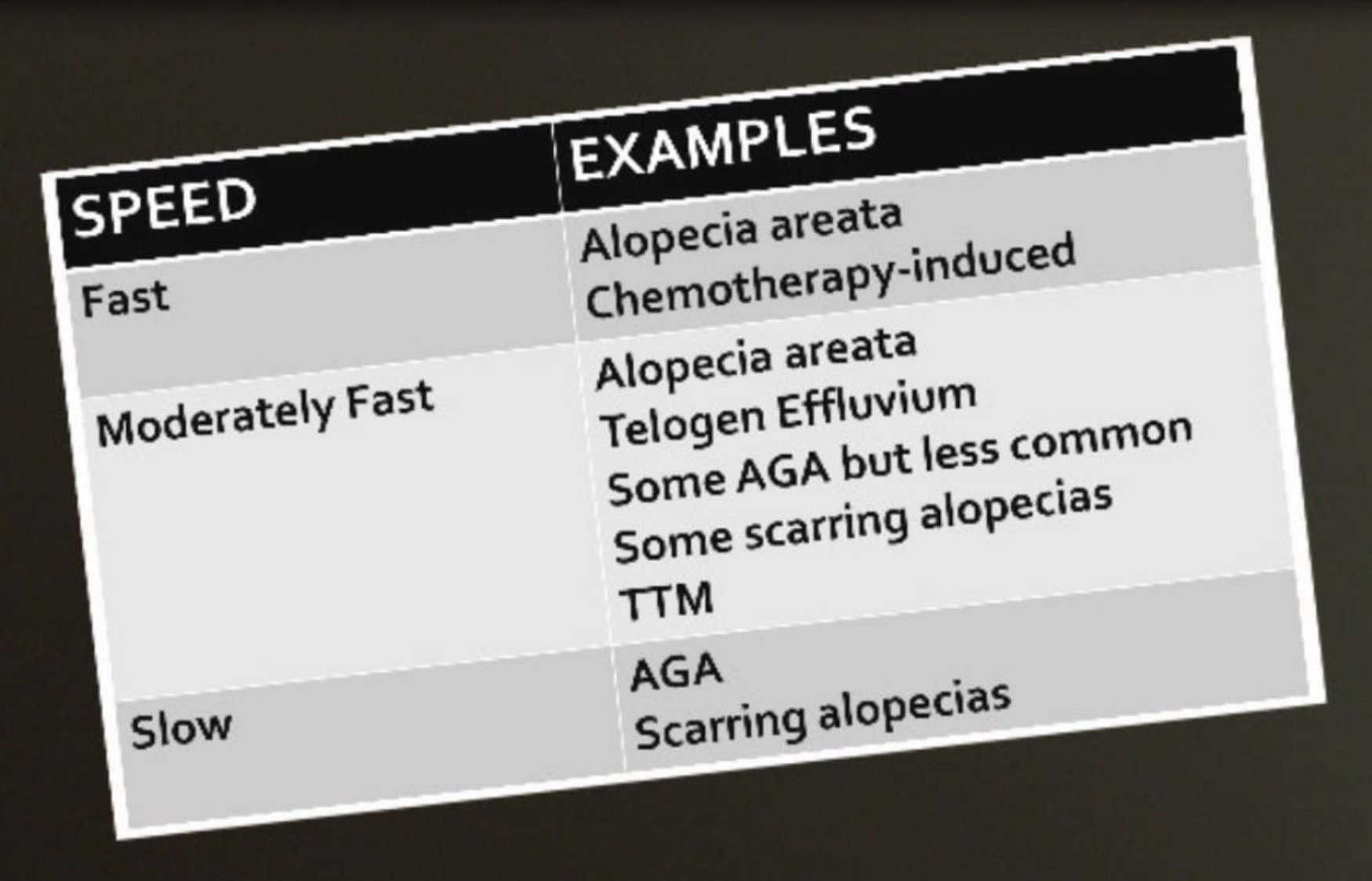
A nice research paper published in the journal called Clinical and Experimental Dermatology looked at these 25 patients so far who were felt to have ‘drug induced alopecia areata.’ The average age of patients with this condition was 42. Alopecia areata developed about 3-4 months after the drug was started.
Features of Drug Induced Alopecia Areata
Here are some of the key features of “drug induced alopecia areata”:
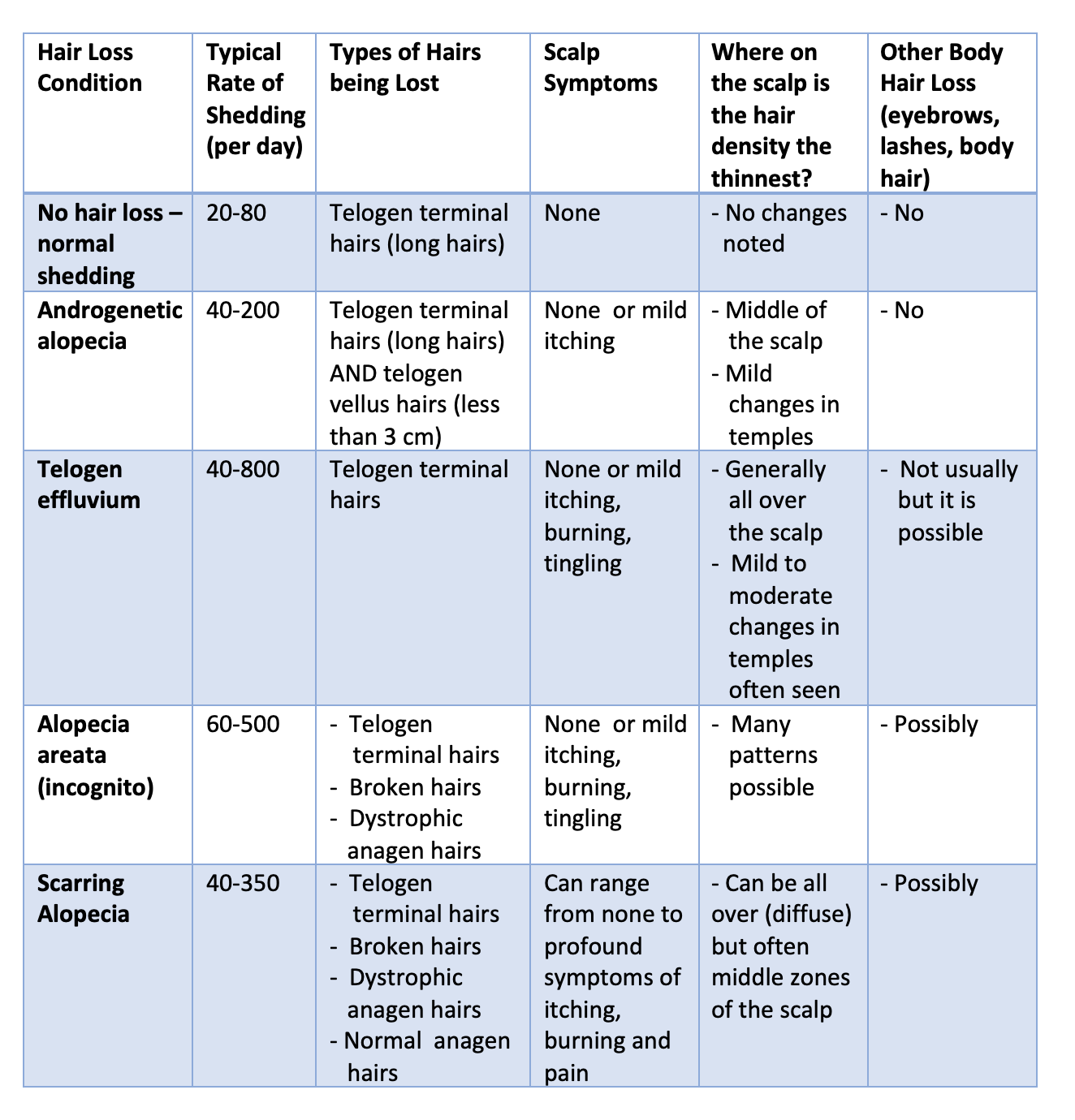
1) There can sometimes be an itchy widespread skin rash on the body plus an itchy scalp eruption that precedes the alopecia by 2-3 weeks. Unlike many drug rashes, the patient here has no fever or joint pains. This itchy rash might not always be present.
2) The hair grows back very rapidly when the drug is stopped and further recurrences of patches of alopecia areata are unlikely to occur provided the drug is avoided.
3) Patches of alopecia areata occur again within weeks when the drug is restarted.
4) Blood tests for autoimmune tests, organ function, etc are normal.
What drugs have been implicated in drug induced alopecia areata so far?
So far, most cases of drug induced alopecia areata that have been published in the medical journals have been with new so called monoclonal antibodies. In fact, ¾ of cases involve a monoclonal antibody. The list of implicated drugs include 14 medications.
The monoclonal antibodies include: Adalimumab, Denosumab, Sulfasalazine, anti PDL 1 inhibitors, Alemtuzumab, Nivolumab, Dupilumab and Secukinumab. The others include Lansoprazole, Rifampicin, Phenobarbital, Acitretin, Abacavir, and Carbocysteine.
Summary
Thanks again for your question. About 2 % of the world will develop alopecia areata during their lifetime and it seems that for 99.999% of patients with alopecia areata a drug is not the cause. But for some it could be. The list of drugs will certainly grow beyond the 14 listed above as we continue to understand this concept of drug induced alopecia areata. Perhaps it’s even a bit more common now than we even realize.
But this diagnosis is so much more complex than simply “I took a drug and then got alopecia areata.”
It’s actually closer to “I took a drug and got an itchy skin rash and then got alopecia areata and then stopped and I did not have a patch of alopecia areata at all until I chose to take the drug again.
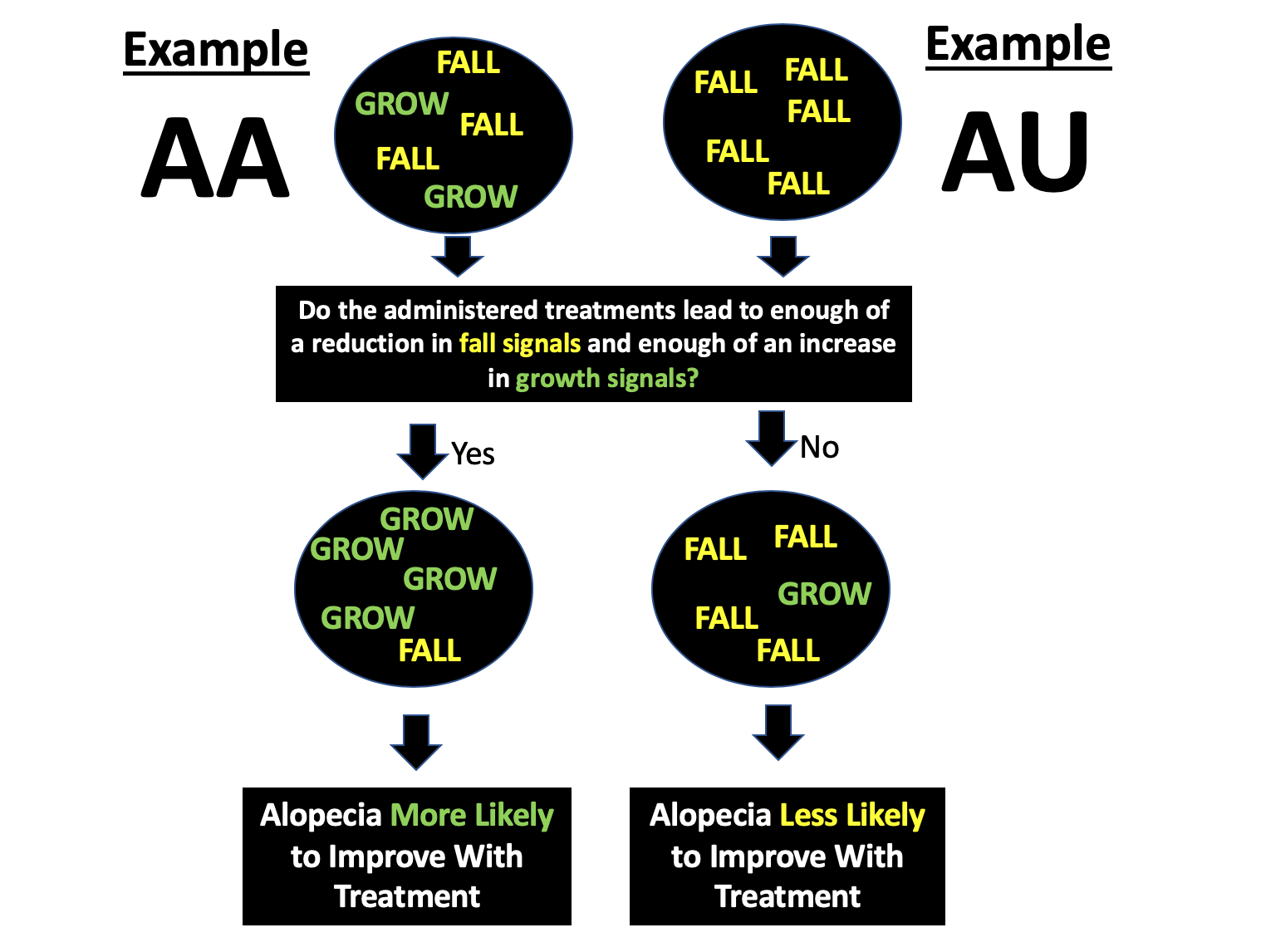
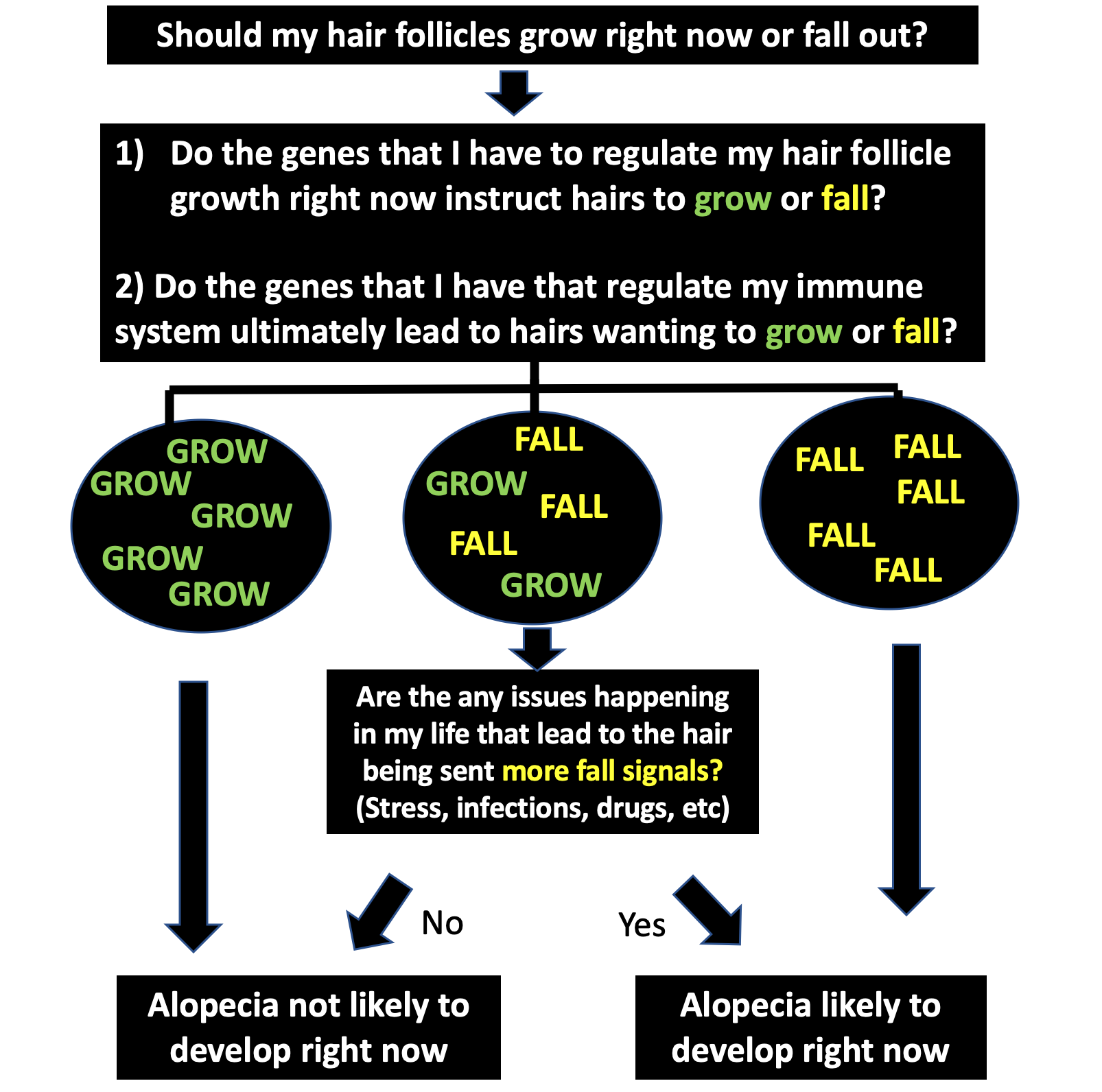
But for most people, the chances of developing alopecia areata was present the day they were born into the world. There’s a number of genes that increase the risk of developing alopecia areata. So these are really the key factors. But there certainly are environmental factors (exposures) that cause the alopecia areata to develop in someone with the right genes. We don’t understand all these environmental factors but the factors that are being studied are include infections, viruses, stress and others. it’s possible drugs are on that list for now.
What’s striking about drug induced alopecia areata is how fast hair grows back when the drug is stopped. Now, we very rarely decide to give the drug again so it’s hard to know in many cases about criteria number 3 (hair loss occurs when drug is restarted). But if hair loss does occur rapidly when the drug is restarted, it really increases the odds that the drug is implicated.
Taken together, trimethoprim/sulfamethoxasole is not on the list of drugs currently implicated in drug induced alopecia areata. That does not mean it can’t be but there is no really convincing evidence. If a person had a rash when using this drug and developed a patch again with the use of this drug it could support a connection. But if there are patches of alopecia areata that develop when a person is completely off the drug, it really makes it less likely that a drug induced alopecia areata is the correct diagnosis.
REFERENCE
Murad A et al. Drug-induced alopecia areata? Clin Exp Dermatol. 2021 Mar;46(2):363-366.