Iron Supplements: How can I raise my ferritin levels?
GENERAL PRINCIPLES OF TAKING IRON PILLS
Iron supplements are commonly prescribed for individuals with low iron stores and low hemoglobin levels. I always advise patients to check with their physicians before simply taking a pill. Some causes of iron deficiency are quite serious and need a proper evaluation. Here are some general principles.
1. There is no perfect choice.
I'm okay with my patients taking most supplements provided they are not having side effects and provided it’s doing a good job and helping to raise ferritin levels. There are over 100 iron supplements on the market. There is no right or wrong as a starting point for most people. If the supplement helps raise ferritin levels to the desired range and the patient feels good while taking the supplement, then it may in fact be the right choice.
2. Start with the least expensive (if possible).
Iron supplements range from 5-10 cents per pill to 1.25 to 1.50 per pill. If a patient generally has a good stomach and is not prone to constipation or diarrhea, I recommend to start with the least expensive forms. They often work very well and the patient has the potential to save a lot of money. Any of the formulations listed in the attachment below are reasonable starting points. Ferrous gluconate for example is just pennies per pill.
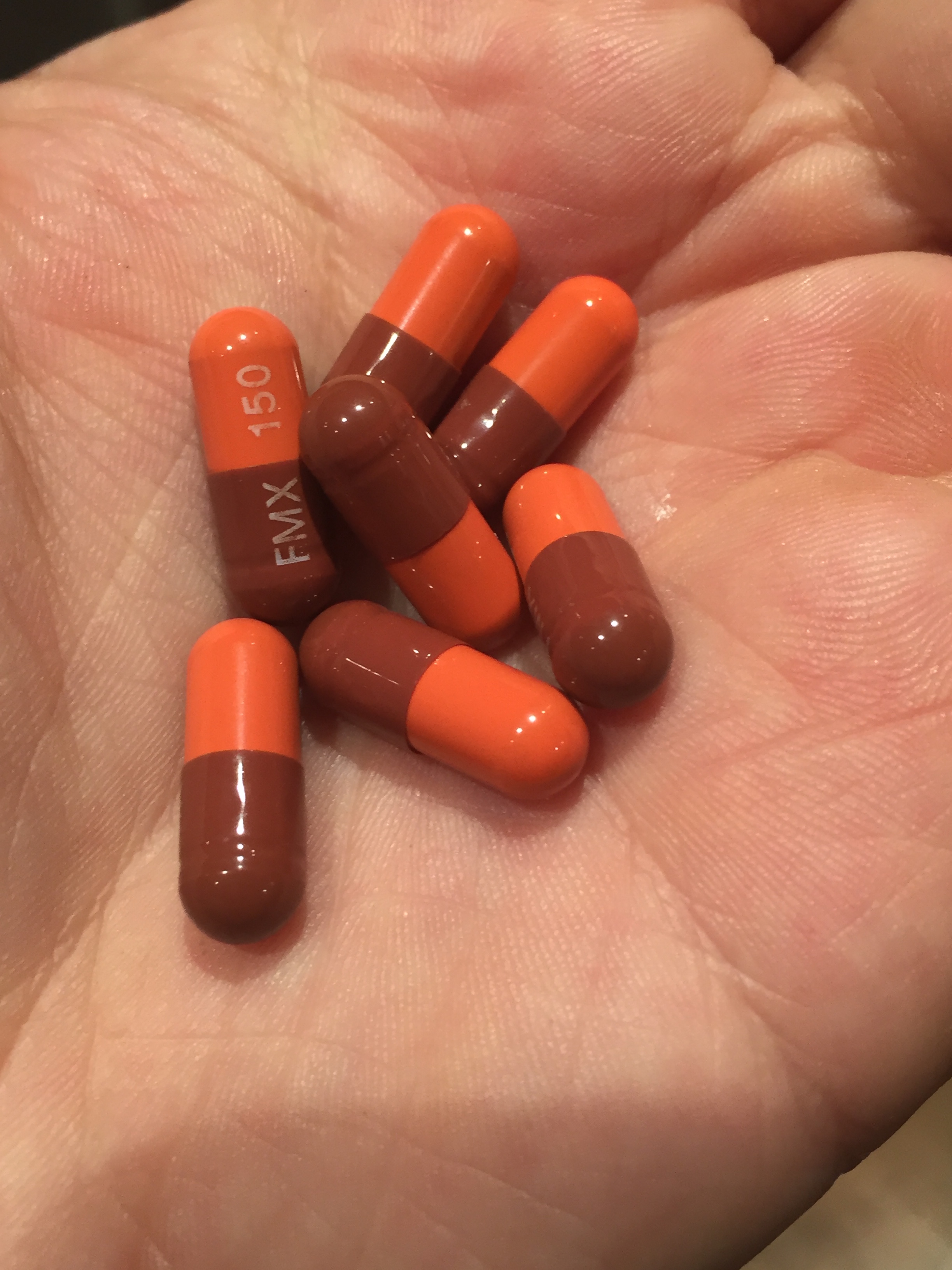
3. I recommend that patients buy specific (more expensive) formulations if they have gastrointestinal issues or use antiacids.
If my patient frequently experiences an upset stomach, or is prone to constipation from previous iron supplements I recommend they consider PROFERRIN or FERRAMAX. Others may also be acceptable. These pills are particularly helpful if patients use antiacids as PROFERRIN and FERRAMAX do not require acid to be absorbed and are therefore acceptable for patients who use antacid medications.
4. Go slowly!
Regardless of which pill a patient chooses, I can't overemphasize the important of the following key message: go slowly! Start with one pill every other day for 5 days and then go up to daily for 2 weeks. I may advise patients to go higher than once daily but it depends on the exact pill they are using.
5. Take the iron with a source of vitamin C.
Vitamin C (ascorbic acid) helps increase iron absorption. Taking iron pills with a glass of orange juice or with an actual vitamin C tablet can help iron absorption. If a patient is using ferrous gluconate, fumerate or sulphate, I advise them to be sure to take their iron supplements 1 hour before a meal or 2 hours after.
6. Avoid milk, calcium, high fiber food and caffeine
If patients are having difficulties raising their ferritin levels, I may advise them to avoid milk, calcium, high fiber foods and caffeine containing beverages. These can impair iron absorption.
7. If more than 1 pill is recommended, spread them out throughout the day.
Iron absorption is much better if the dose is spread out throughout the day rather than taken all at once. In addition, this may help to limit gastrointestinal side effects, such as nausea and vomiting.
8. If liquid iron is chosen, be aware that it may stain teeth
Liquid forms of iron may stain the teeth. If patients are using liquid iron they may wish to combine with fruit juice or tomato juice to limiting staining. Drinking the iron with a straw may also help.
9. If necessary, oral lysine supplements at 500 mg twice daily can also help to increase iron absorption.
Lysine is an amino acid (a building block of protein). Studies have shown that L-lysine can help increase iron absorption. If patients are having difficult with raising their ferritin levels, I may advise them to include L-lysine in their plan.
10. Follow your ferritin levels.
One should never ever start iron pills unless they plan to test their levels again at some point in the future. This is important. The precise time point to retest ferritin levels will differ from patient to patient but is never sooner than 3-4 months and never more than 9 months. Testing ferritin levels weekly or monthly is pointless. However, re-testing a few months down the road is a good idea.
11. If one has low hemoglobin and low ferritin, further evaluation and tests might be needed.
Anyone with low hemoglobin and low ferritin needs to speak to their doctor about a range of tests. They may not be necessary of course, but one needs to consider celiac disease, excessive menstrual bleeding (women), gastrointestinal bleeding, dietary issues, and a range of other illnesses. In my clinic, I generally screen for celiac disease (gluten sensitivity) in all patient’s with low hemoglobin and low ferritin. Patients with persistently low levels need a full evaluation by physician.
Conclusion
Taking iron is easy for many individuals but presents its challenges to some people. For some, the ferritin levels simply don't budge upwards despite taking iron. For others, any amount of iron causes gastrointestinal upset. A slow are methodical approach such as that suggested above often helps increase levels.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.