Children of Women with Polycystic Ovarian Syndrome:
What is the latest research ?
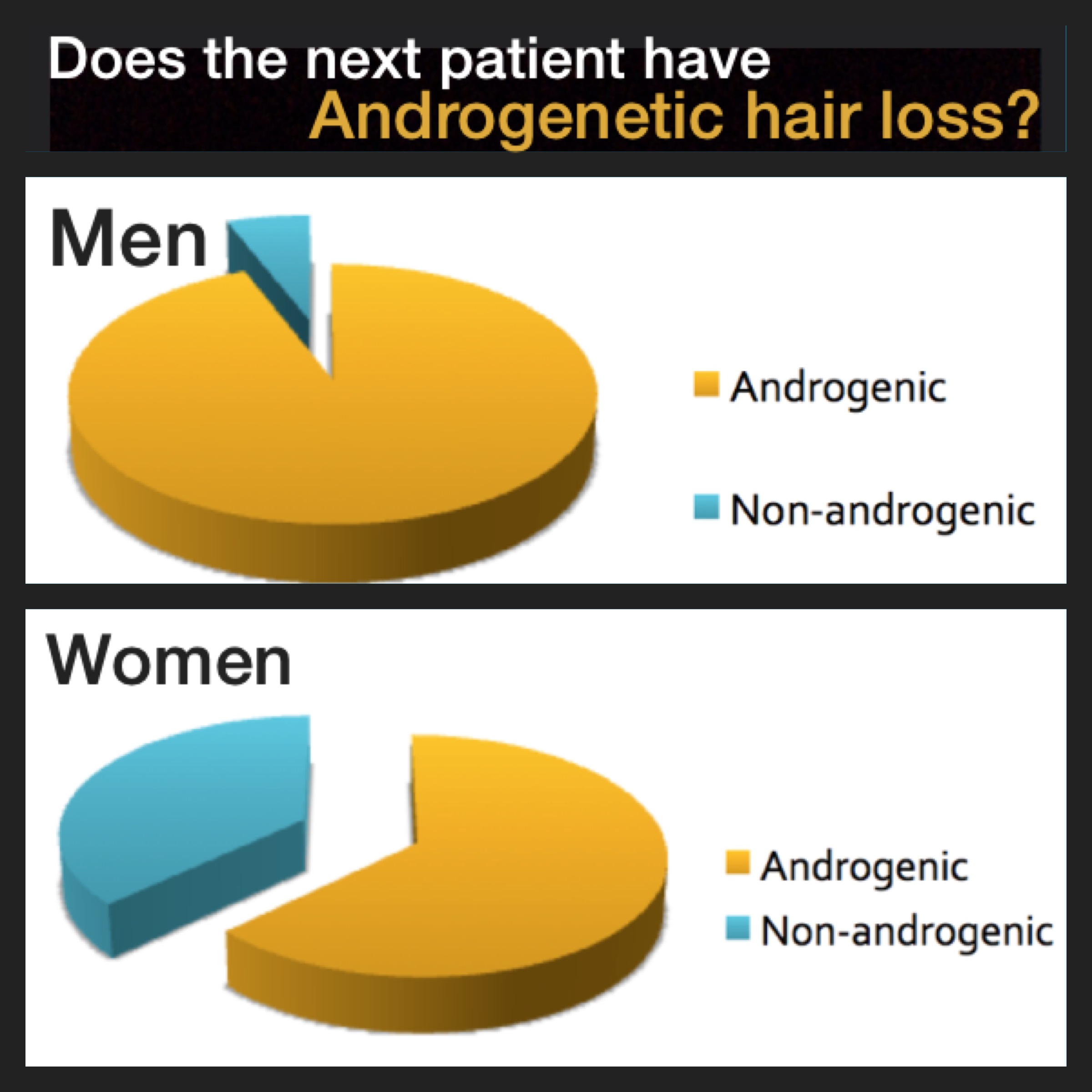
Polycystic ovarian syndrome (PCOS) is a hormonal disorder in women. It is not one condition but a constellation of symptoms. Patients with PCOS typically have evidence of hyperandrogegism (excess male type hormones and irregular periods. Women with PCOS typically have cysts present in the ovaries but some do not. The exact cause of PCOS remains unknown although a genetic component is likely for many women. The ovaries of women with PCOS are known to secrete higher levels of male hormones which contributes to irregular periods and infertility. Women with PCOS may seek medical attention for a variety of reasons including insulin resistance, diabetes, high blood pressure, acne, increased hair growth on the face, irregular periods, infertility. Women with PCOS may also present to a hair clinic with concerns about androgenetic alopecia. It is therefore extremely important that hair specialists understand this condition.
New Research on Children born to Mothers with PCOS
A great deal of research is currently being conducted into the cause of PCOS and how it affects women. Research is also being conducted into the health of babies born to mothers with PCOS. Research has suggested that the hormonal changes in utero influence the development of the fetus.
One issue that has been studied is the risk of attention-deficit/hyperactivity disorder (ADHD) in babies born to mothers with PCOS. ADHD is the most common childhood neurodevelopment disorder. Male hormones may play a role as boys are two to three times more likely to develop ADHD.
A study by Berni and colleagues of over 16,000 women showed that women with PCOS have a slight risk of giving birth to children with attention deficity hyperactivity disorder (ADHD) and Asperger syndrome.
Kosidou and colleagues performed a matched case-control study using health and population data registers for all children born in Sweden from 1984 to 2008. In their study, a total of 58,912 ADHD cases (68.8% male) were identified and matched to 499,998 unaffected controls by sex and birth month and year. The results indicated that Maternal PCOS increased the odds of offspring ADHD by 42% after adjustment for confounders (odds ratio [OR], 1.42; 95% confidence interval [CI], 1.26-1.58). The risk for ADHD was even higher among obese mothers with PCOS and was highest among obese mothers with PCOS and other features of metabolic syndrome.
Conclusion
Recent research suggests that differences in maternal hormones during pregnancy in women with PCOS affect the chances of having children with ADHD and possible other neurodevelopmental issues. Overall the risk is low.
REFERENCES
Berni TR, et al. Polycystic ovary syndrome is associated with adverse mental health and neurodevelopmental outcomes. J Clin Endocrinol Metab. 2018.
Kosidou K, et al. Maternal Polycystic Ovary Syndrome and Risk for Attention-Deficit/Hyperactivity Disorder in the Offspring. Biol Psychiatry. 2017.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.