Do I just need patience or is my hair density not going to fully return?
Is my hair density going to return?
I’ve selected this question below for this week’s question of the week. It allows us to the review some key concepts in the diagnosis of hair loss in the early stages.
QUESTION
I am a 40 year old female. I have always had a lot of hair, and coarse hair. I have always been a shedder, but it never made a difference on how dense my hair was. Until now. I had my "normal to me" hair up until August/September 2020. But, in September/October, I started to see a lot more hair coming out in the shower/brushing afterwards/when blowdrying.
Handfuls would come out in the shower when in the shower. It was definitely the worst/at it's peak in November 2020.
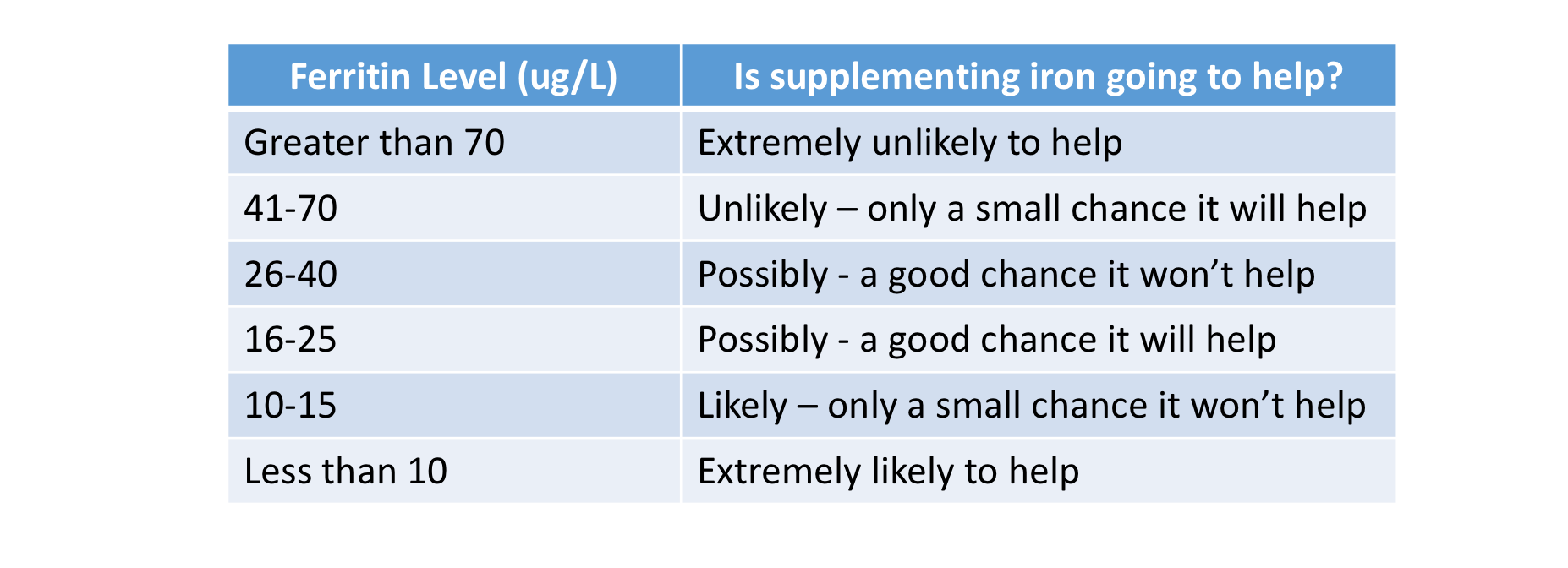
I remember after one shower the entire wall was covered with the hair I collected. By this time I started to freak out a bit. It was definitely making a difference on my head now as far as density. I went to my family doc, and he did blood work. My ferritin came back at 21, but my hemoglobin was ok. I started taking iron supplements at the end of November. At the end of Jan 2021 I went to see a dermatologist. She only had a physical look at my scalp, did not do a biopsy and did not look at my scalp with any sort of magnifying tool or anything. She said based on my story she thought it was either Androgenetic Alopecia or Telogen Effluvium. She had my vitamin D tested. It was a bit low, so I started taking 2000IU of vitamin D daily. The hair shedding continued like this until end of February-ish/beginning of March. (The lost hair was mostly long hairs, some medium length, barely any short hairs)
In March/April 2021 the hair fall slowed down a lot, and now I would say it is back to a normal amount with each wash.
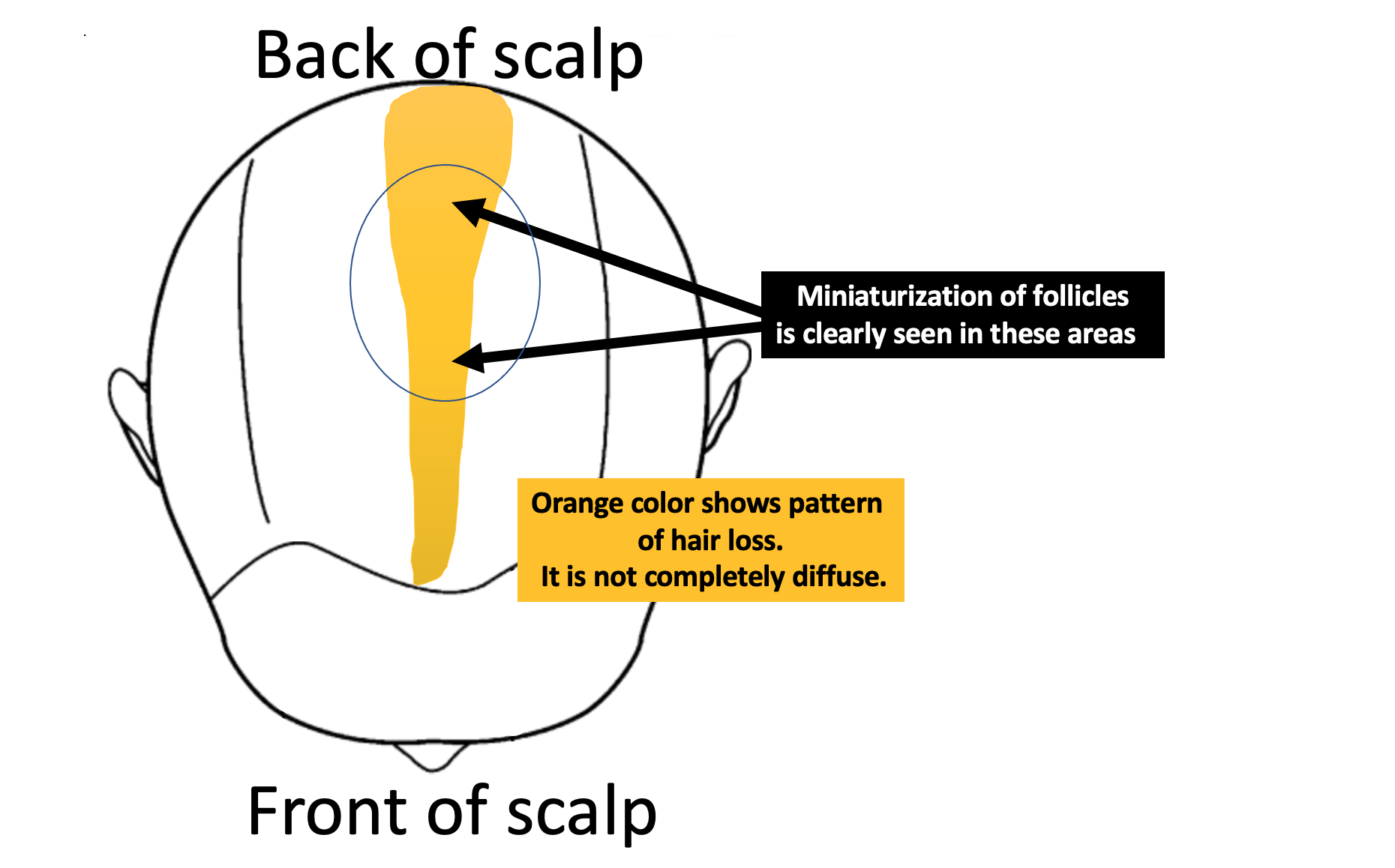
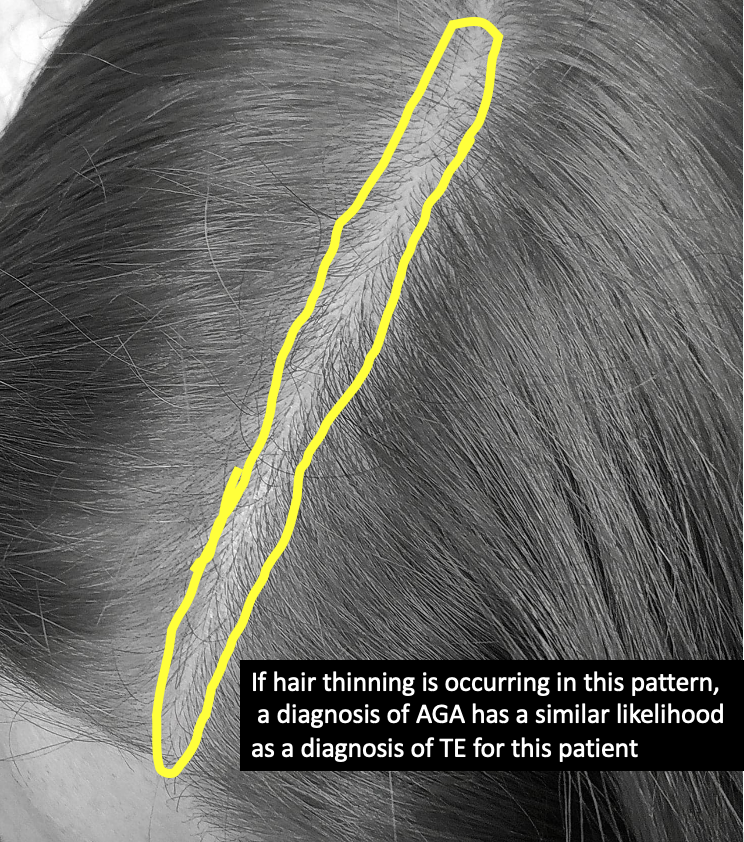
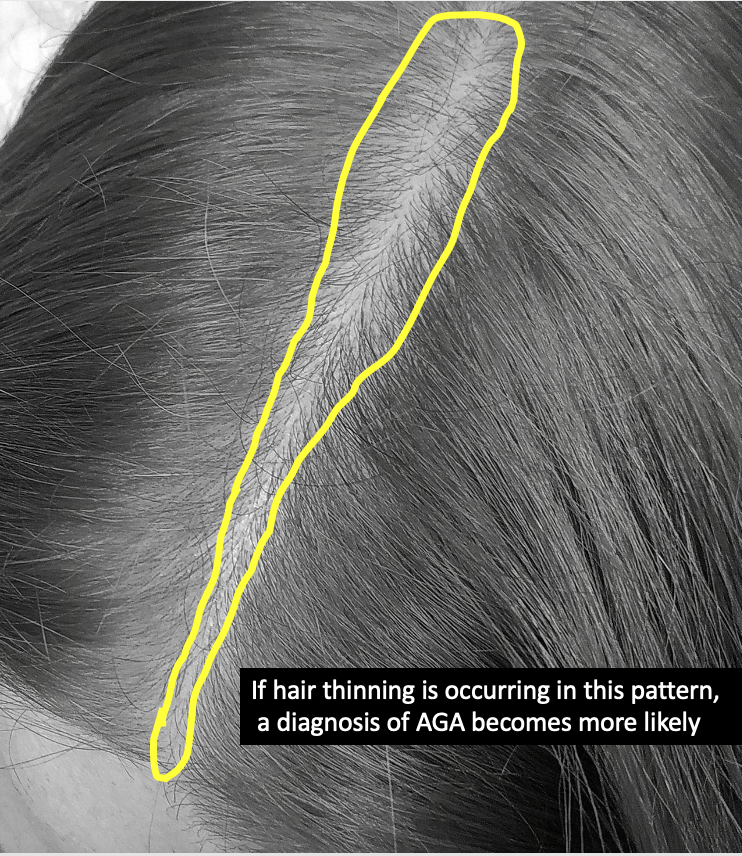
But, I can definitely see a difference on my head. It is most noticeable on the top/sides of my head, and down the back of my head (I have weird parts all along the back of my head). It also sort of looks like I lost hair at the nape of my neck. My part has not gotten wider at all, but sparser. I do have a lot of new growth at the top and back of my head, but it doesn't seem like enough to make a difference in terms of overall thickness, even when it grows longer.
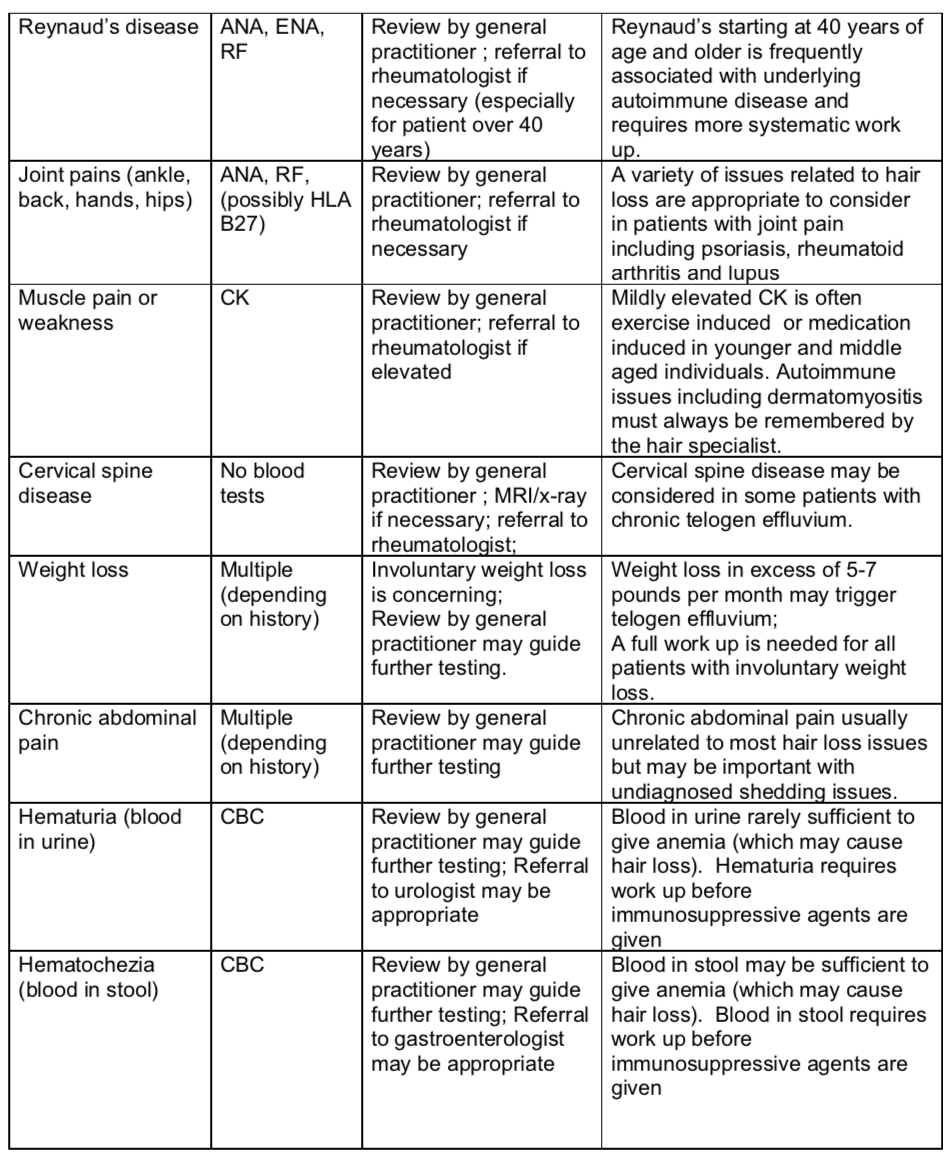
My scalp hurts often, as if it has been in a super tight ponytail, even though it has not. Sort of hurts to move it around. My scalp can be quite dry/itchy at time (always has been like this, even before hair loss)
I am still taking iron supplements, as when I was re-tested in February my ferritin had only gone up to 30. I am also still taking the vitamin D daily. I should mention I take 2.5 or Ramipril daily.
My question is … would Androgenetic Alopecia happen that quickly and then taper off that quickly? And, if it is Telogen Effluvium would I expect to have more re-growth by now? Or, is there any chance I could have some sort of diffuse Alopecia Areata, based on what is happening at the nape of my neck and the weird parts down the back of my head? I have attached some photos. I am trying to be patient, as I know hair takes a long time to grow.
Thank you for your input!!
Image 1. Hair density in the central part.
Image 2: Hair density in the crown.
Image 3: Hair regrowth.
ANSWER
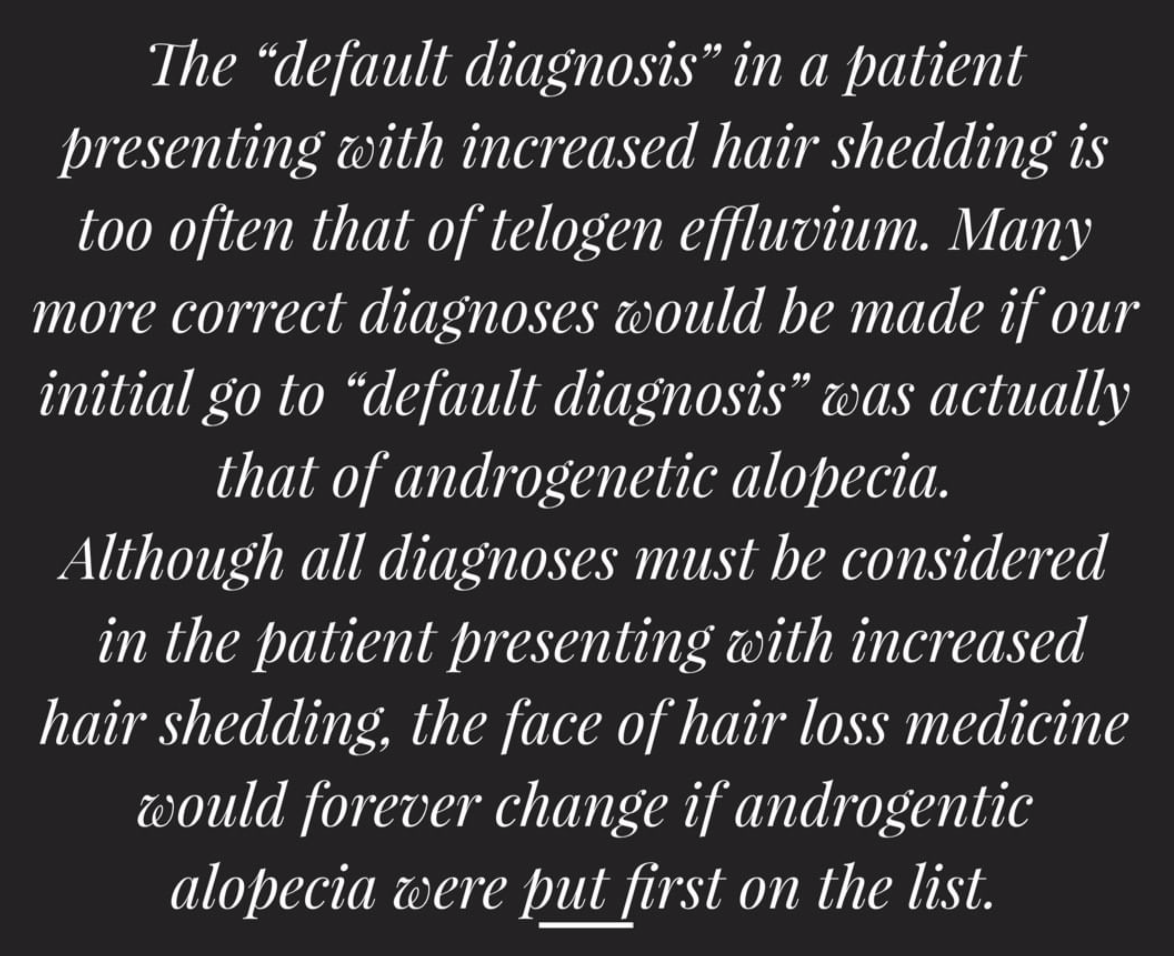
Thanks for the great question. The short answer is that many diagnoses are possible for you. I’ll get into these in just a moment.
I would need to see your scalp and know more about your full story to tell you which diagnosis (or diagnoses) you actually have…. but the 6 possibilities are outlined below. Each of these possibilities has different probabilities for being your actual diagnosis. If I was to see your scalp, these ‘estimated’ probabilities would change. However, with the information provided, we have six scenarios. The most likely is scenario 1 and 2 followed by scenario 3.
Six Possible Scenarios for Your Hair Loss
There are six possible scenarios for your hair loss. The most likely is scenario 1 and 2 followed by scenario 3.
Scenario 1) You have a telogen effluvium due to low iron or low vitamin D. This has now been fixed and you need to give it until October/November in order for your density is going to come back.
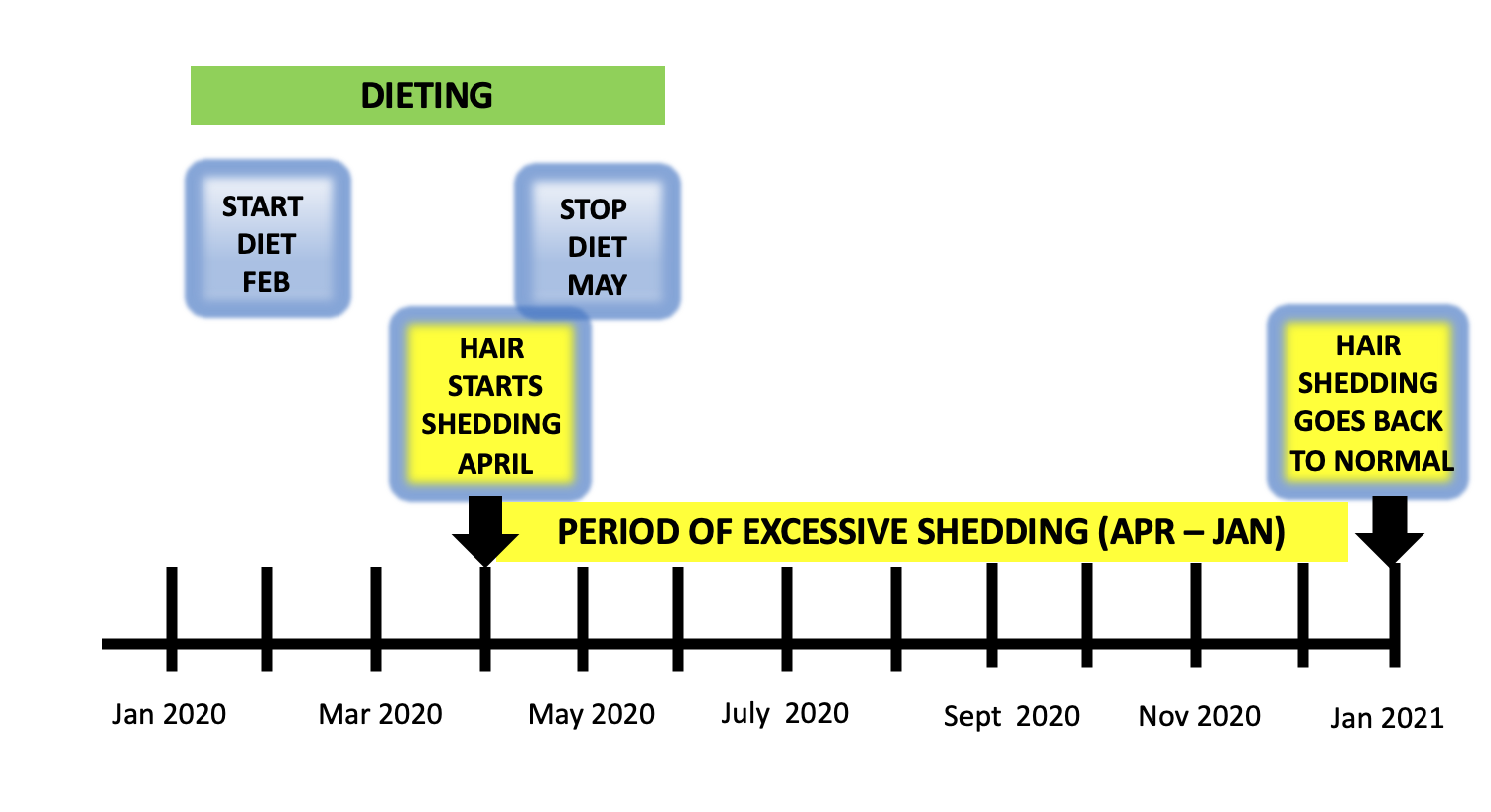
Scenario 2) You have a telogen effluvium for some other reason (other than simply low iron and vitamin D) and it has now somewhat resolved and you need to give it until Oct/November in order for your density is going to come back. Causes of telogen effluvium that could be relevant for you would include stress last summer 2020, low iron (which you might have), thyroid problems, medications started last summer, weight loss last summer, COVID infection last summer. Other causes are possible too.
Scenario 3) You have actually had a hint of subtle “subclinical” androgenetic alopecia for a while and this recent telogen effluvium has “unmasked” the subtle androgenetic alopecia. Your density is going to improve by the Fall 2021 now that your telogen effluvium is resolving but you might or might not get back all your density - but you may come pretty close.
Scenario 4) You have an inflammatory scalp condition that has been present for a while and is now acting up to give periods of hair shedding. The iron and vitamin D are unrelated in this particular scenario and are simply a true red herrings. Your inflammatory scalp condition has now settled again but you need to give it until November/December to see if things will fully settle. Such inflammatory condition could include seborrheic dermatitis, psoriasis, scarring alopecia or contact allergy (ie to some ingredient in a shampoo, conditioner, hairstyling product or dye). This scenario number 4 carries a risk of flare again.
Scenario 5) You have an inflammatory scalp condition that has been present for a while but it’s not enough to give hair loss. A new telogen effluvium has come along that will resolve and time will tell whether the inflammatory scalp condition also settles fully. If the inflammatory scalp condition is a low grade scarring alopecia, density won’t come back fully but still will improve to some degree when the current telogen effluvium resolves.
Scenario 6) You have an inflammatory scalp condition that has been present for a while but it’s not enough to give hair loss. You also have a subtle amount of androgenetic alopecia that has now been unmasked by the new telogen effluvium. If the inflammatory scalp condition or androgenetic alopecia is active enough it may prevent density from coming back to your full normal by Fall 2021.
Detailed Review of the INITIAL Situation (August 2020 to Dec 2020)
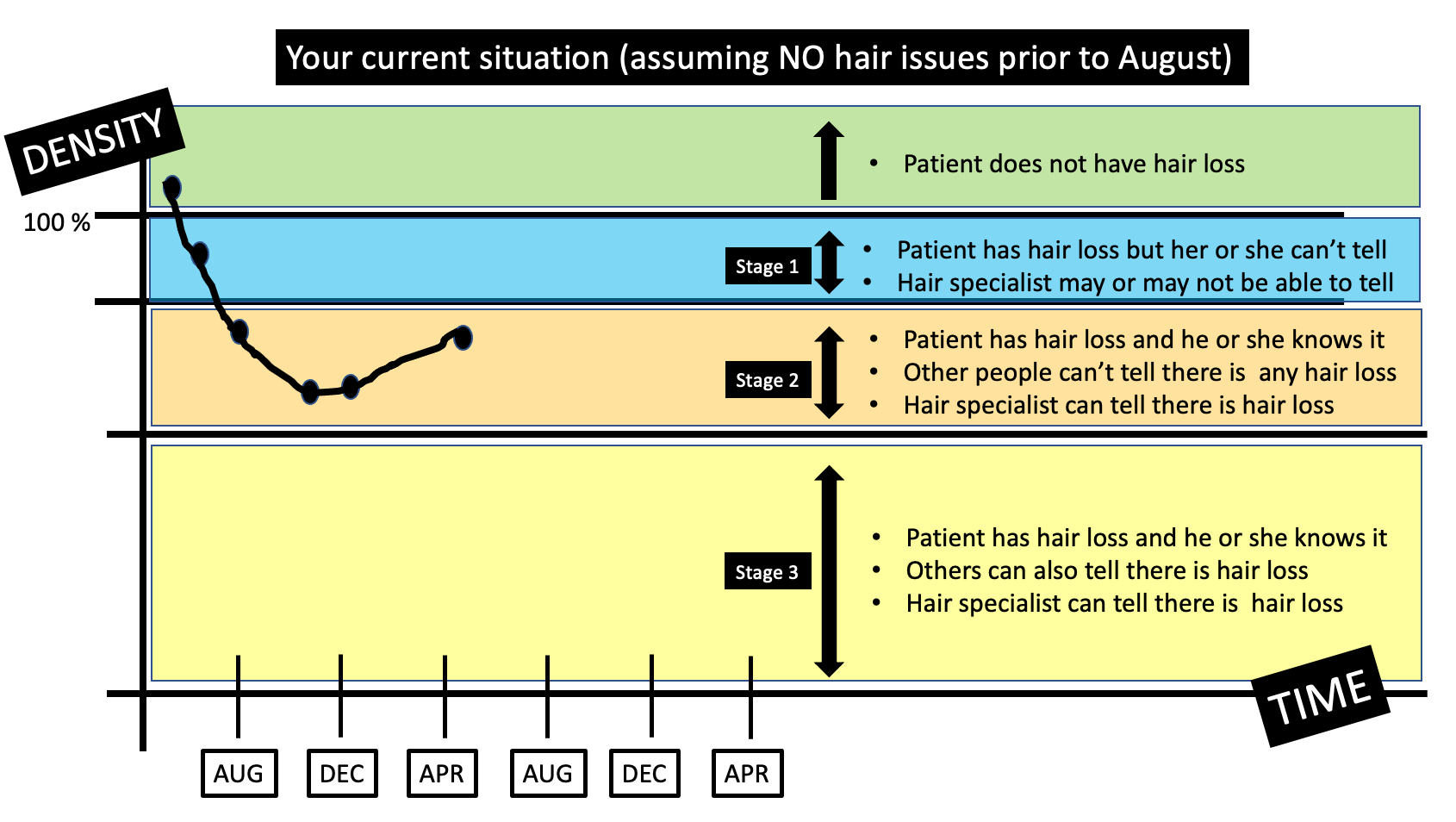
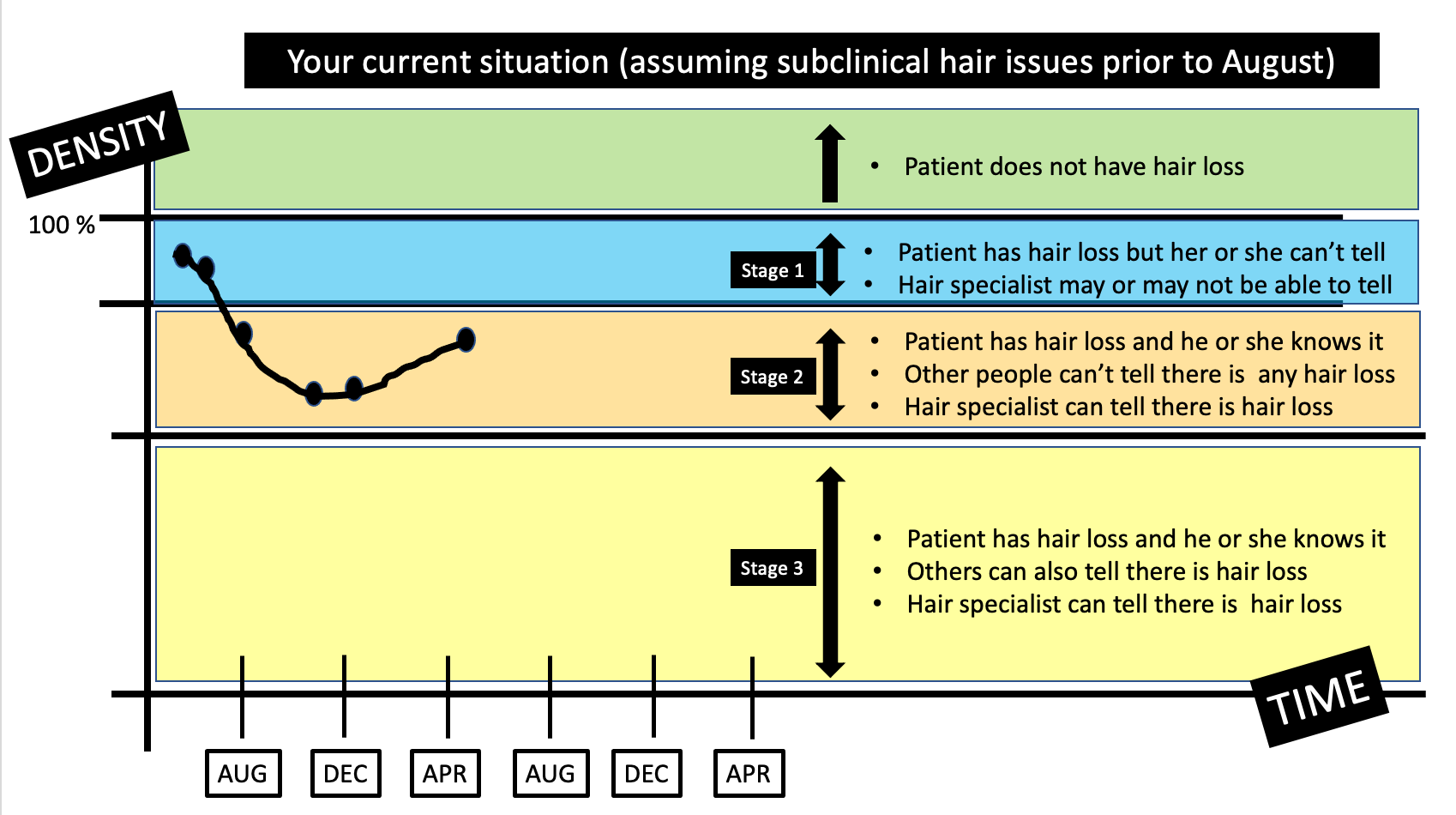
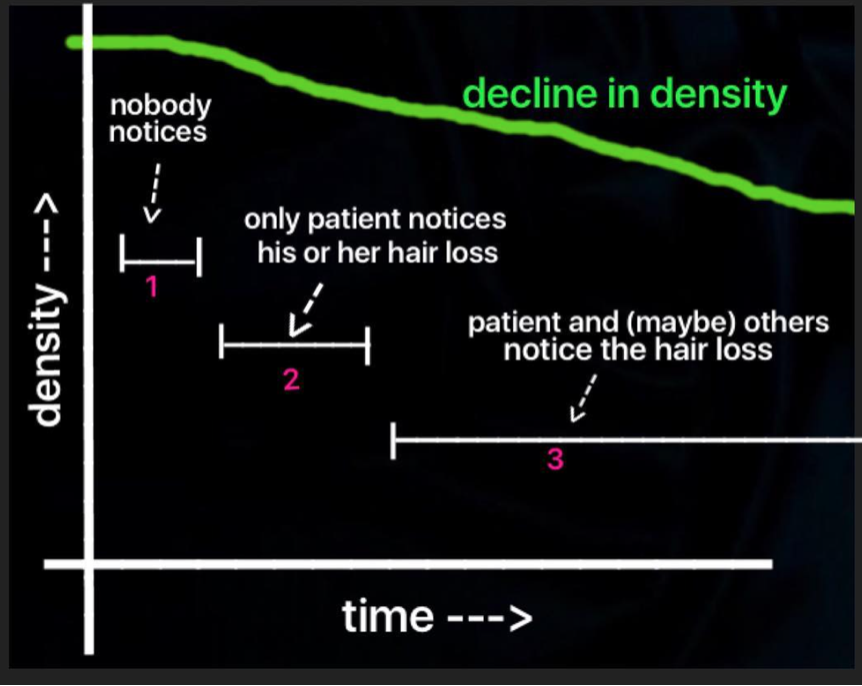
Let’s go further into the situation that you describe in your question. Before we do, let me point out that there are three stages of hair loss for most people. At least that’s a helpful way that I view hair loss. These stages are important to appreciate because it impacts how I approach your question.
In “stage 1” of hair loss, the patient has hair loss but doesn’t really know it. For all practical purposes, the patient feels the hair looks the same as it always did and feels the same as it always did. Perhaps when they look at a photo from years gone by they might say something like “Wow, I can’t believe how much hair I had back then!” Otherwise stage 1 of hair loss is unrecognizable by anyone - patient, doctor, specialist or hairstylist.
In “stage 2” of hair loss, patients themselves realize they have hair loss - but others around them don’t believe it or don’t realize it. The patient feels the pony tail is smaller or the scalp is more see through or something is just not the same. A spouse, sister, parent, daughter, son, barber, hairstylist or friend usually say the same thing - “You’re exaggerating ! Everything looks fine to me! Sometimes that sentence is delivered by the doctor or other hair expert that has been asked to help.
Stage 2 is sometimes frustrating and lonely and anxiety provoking. Patients feel something is wrong but the world around them says repeatedly that everything is just fine.
Now, some patients in stage 2 resolve their hair loss and go back into stage 1 and so they do end up feeling they were exaggerating because everything resolves itself. Some patients stay in stage 2 and eventually find an answer to their hair loss issues. If specialist A does not believe them, they move on to specialist B. If specialist B does not believe them, they move on to specialist C.
Some patients in stage 2 do progress on to stage 3 of hair loss where hair loss becomes more noticeable to others. With hairstyling and camouflage a patient in stage 3 might still be able to hide their hair loss. With treatment of course, a patient may be able to return to stage 2 or even stage 1.
With these stages in mind, let’s delve a little further into this situation you have mentioned in your question.
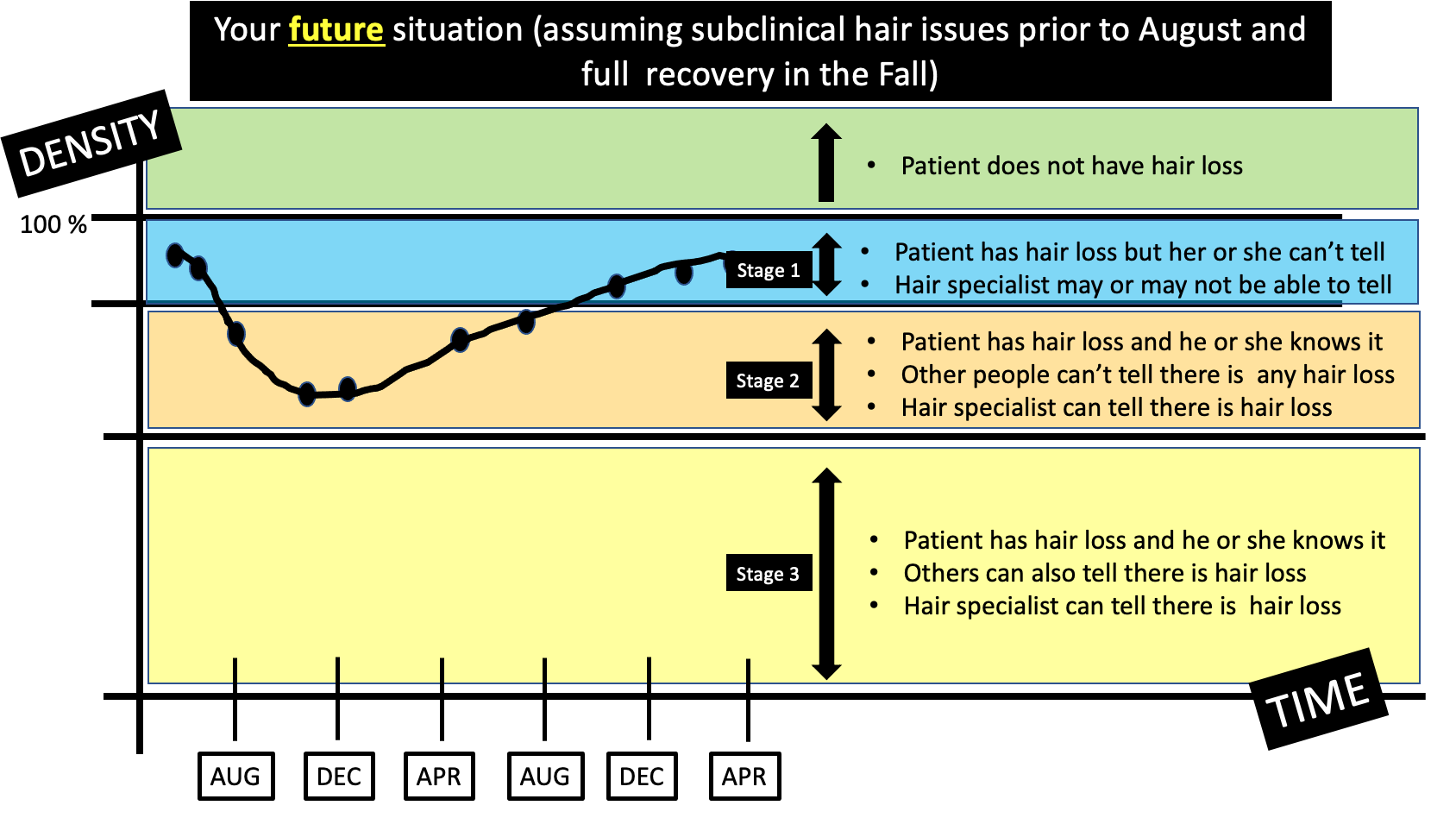
There are two main scenarios that may have been present before you noticed hair loss in August. The first is that your hair density was completely normal and the same as it was when you were 20. You then lost hair in the August - December period and the density went down. In other words, you went from no hair loss to stage 2. This is shown below.
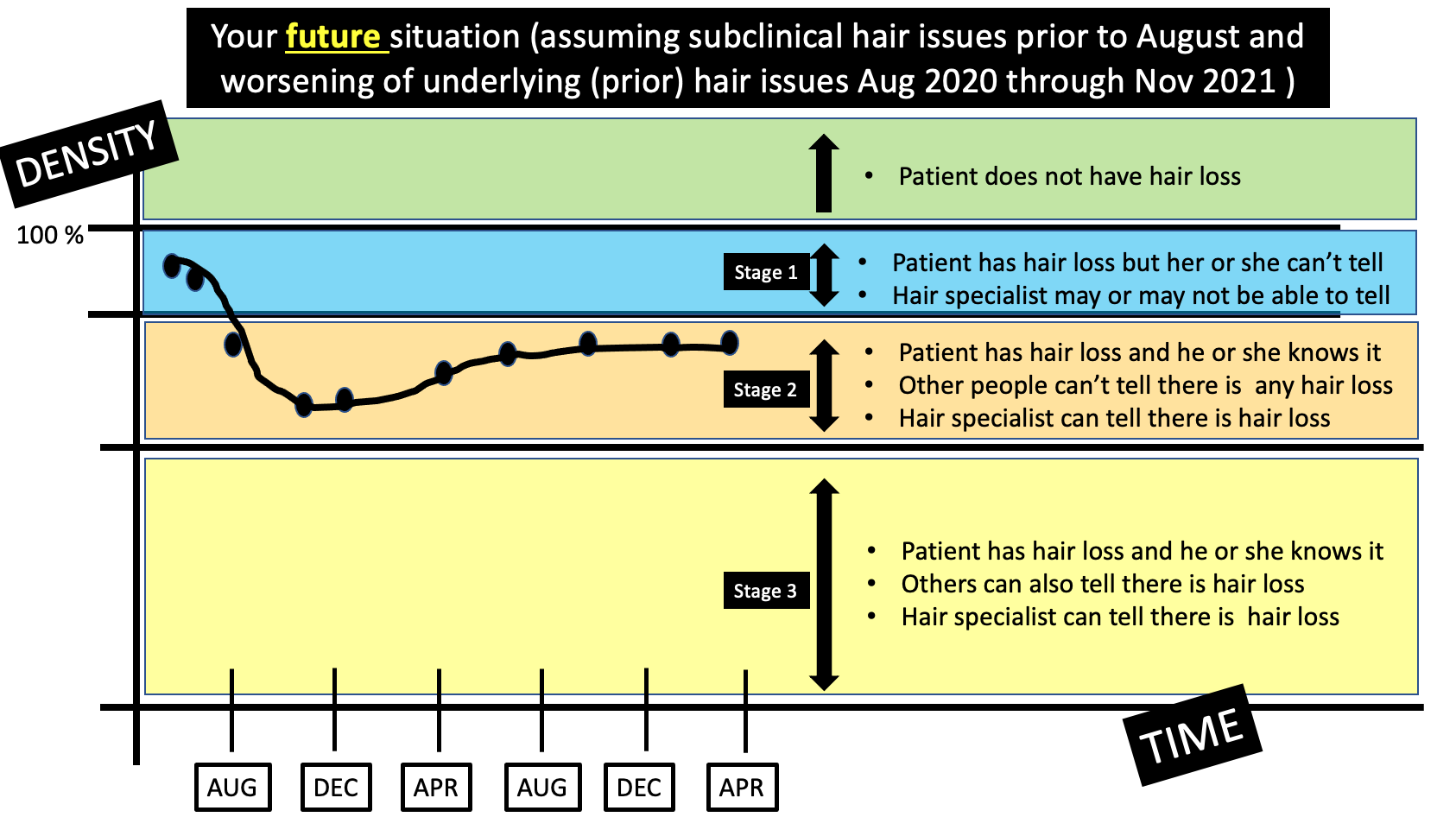
The second scenario is that you felt that your hair density was completely normal but it was not, in fact, completely the same as it was 20 years ago. You then lost hair in the August - December period and the density went down. In other words, you went from stage 1 of hair loss into stage 2. This is shown below
Both of these situations above would appear identical to you. In the first situation, you had normal hair to start and then you lost density. In the second situation, you had (what you thought was) normal hair to start and then you lost hair. The only difference is that in the second sitatution you actually didn’t have quite normal hair - it just seemed that way to you (and everyone else).
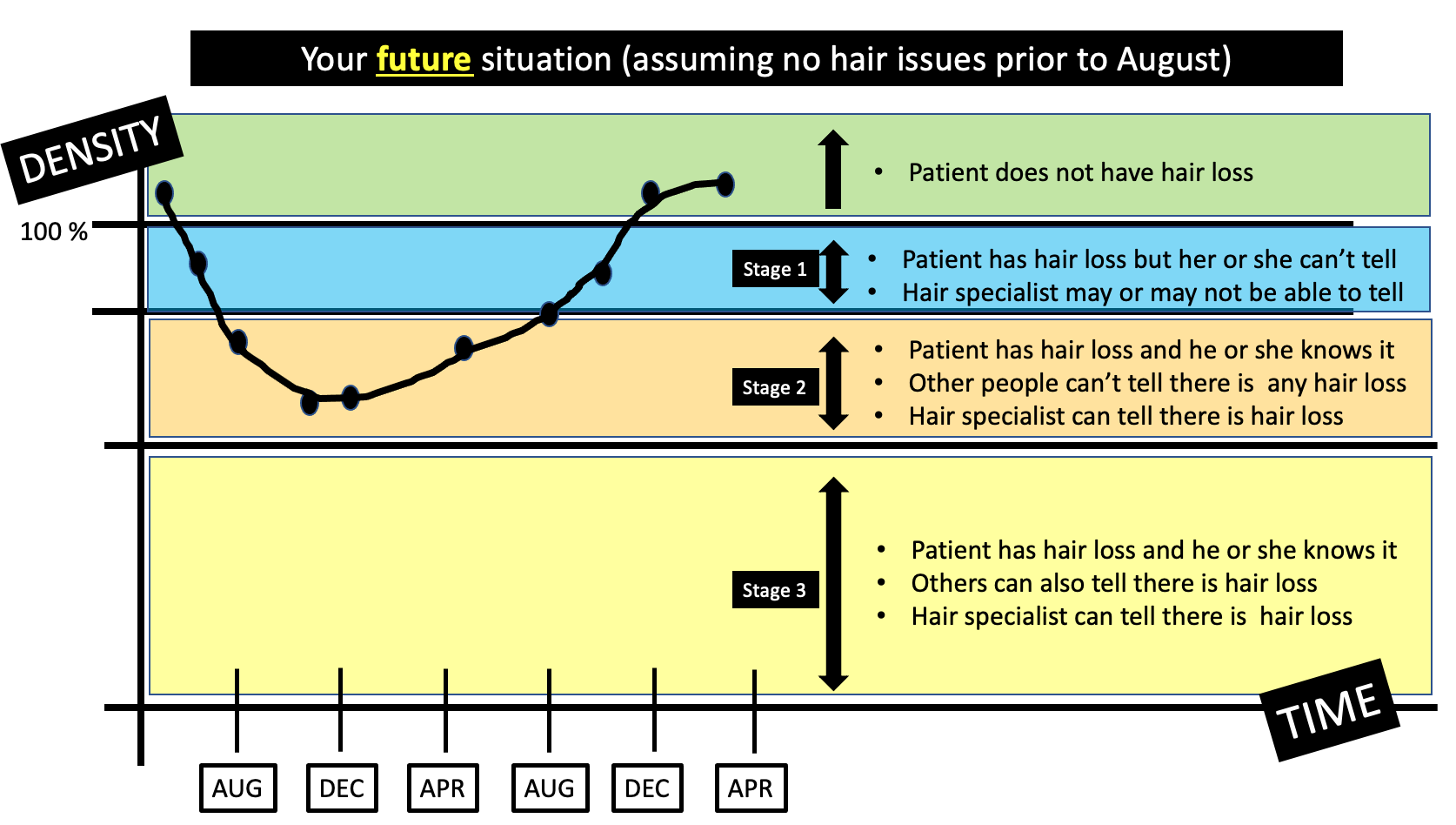
Detailed Review of the RECOVERY (April 2021 to Dec 2021).
Your hair loss is now in a recovery phase. Your shedding has stopped. You are sprouting hair everywhere!
Let’s spend some time looking at the recovery of your hair loss and how the hair might respond over the next few months. The most likely are the following 2 scenarios.
If you don’t have any underlying issues that are affecting how hair grows, then it’s likely that this telogen effluvium will continue to settle and a you’ll get a return to full growth by the end of the year. In other words, you’ll go from stage 2, into stage 1 and back to full hair. The chapter on hair loss will be closed
Even if you do have some kind of “subclinical” hair loss situation happening in your scalp, there is still a good chance that you’ll recover your density by the end of the year and you’ll return feeling that your hair feels ‘full’ to you. In other words, you’ll move from stage 2 into stage 1. Stage 1 of hair loss looks just as good of having no hair loss at all so for all practical purposes it does not matter.
What happens if my density does not recover by the end of the year?
The final scenario is a bit trickier to explain. If you did in fact have some sort of subclinical hair loss situation going on in the scalp before August 2020 and this condition got a little bit worse from August 2020 through summer 2021, then you might not find that you have a full recovery by the time the Fall 2021 comes around. This could be due to several situations including
a) you had some subclinical androgenetic alopecia prior to August 2020 and the androgenetic alopecia got a bit worse from August 2020 to August 2021.
b) you had some subclinical scarring alopecia prior to August 2020 and the scarring alopecia got a bit worse from August 2020 to August 2021.
c) you had some subclinical psoriasis or contact dermatitis prior to August 2020 and the inflammatory issues got a bit worse from August 2020 to August 2021.
In these situations, it’s possible you stay in stage 2.
This final scenario is the least likely but a proper scalp examination and full review of your story is going to help me decide just how likely it is in your specific situation. For now, I estimate it as unlikely (but not zero).
What you can see here in these examples above is that you really need some definite diagnoses. If you allow time to help you with a solid diagnosis then that’s one good strategy. For example, if your density comes back perfectly to normal by the end of the year, then there’s probably no real hair issues at all that need treating or need any kind of workup. In other words, if your density returns back to full by December 2020 (and you enter stage 1 or no hair loss), it’s pretty unlikely there’s any other hair loss issue going on.
But if density does not return, I strongly believe that you need to have some formal diagnoses put on paper for BOTH the hair loss and the scalp symptoms. The reason we need different diagnoses is because every hair loss condition is treated differently. Unless we have a diagnosis, we can’t formulate the right treatment plan.
My Final Comments
Thanks again for the great question.
I’m really glad you are seeing all this hair growth sprouting everywhere as it’s a really good sign. The hairs are about 5-6 cm so it seems that the telogen effluvium you had in Aug/Sept 2020 is settling down. It could be that the iron and/or vitamin D is helping or that could just be a coincidence. It’s difficult to prove.
I do feel your scalp symptoms (dry, itchy, hurts to move) needs a formal diagnosis. Your scalp symptoms need a name of some kind. Now, keep in mind that the diagnosis of that situation might not be anything concerning given how long you have had it, but it still needs a formal diagnosis. If nobody is sure of what to call your itching and soreness, then you need a scalp biopsy. That is pretty clear in my mind. There is flaking present in some of your photos so there is some kind of inflammatory issue present. I would need to see the scalp up close to give a diagnosis. Please be sure to follow up on that.
I am glad you are taking photos as that will be key over the next 6 months. If you feel by November/December 2021 that you are really happy with your hair and how the density has returned, then this chapter of your hair story is likely done: you had a telogen effluvium and it resolved. It went away. In this situation, it’s unlikely there is some subclinical androgenetic alopecia present but it does not really matter much. I wouldn’t treat hair loss if you go back to feeling good about your hair. I’d simply repeat photos in 1 year. Put the shedding episode behind you for now.
If your density does not return to normal by the end of the year, then there is a good chance that there is some androgenetic alopecia that has entered the picture. No, it’s not 100% but that becomes increasingly likely. There’s very small chance that another diagnosis besides androgenetic alopecia is responsible but that’s pretty rare. Of course, the itching and tender issues on your scalp need to be diagnosed properly. That may or may not have any role here. But someone needs to give it a name.
But if you are pleased with your density in November/December 2021 and your shedding is completely back to normal (and stays normal), and your scalp symptoms are not worrisome to you and your doctors …I would put it all to rest and simply take a photos again in 1 year. It’s helpful to have your doctors follow you closely but nobody really knows their hair better than you. If you feel your hair has not returned back to normal, then you have remained in stage 2 and need a solid convincing diagnosis.
I hope this helps.
Many thanks for the question.