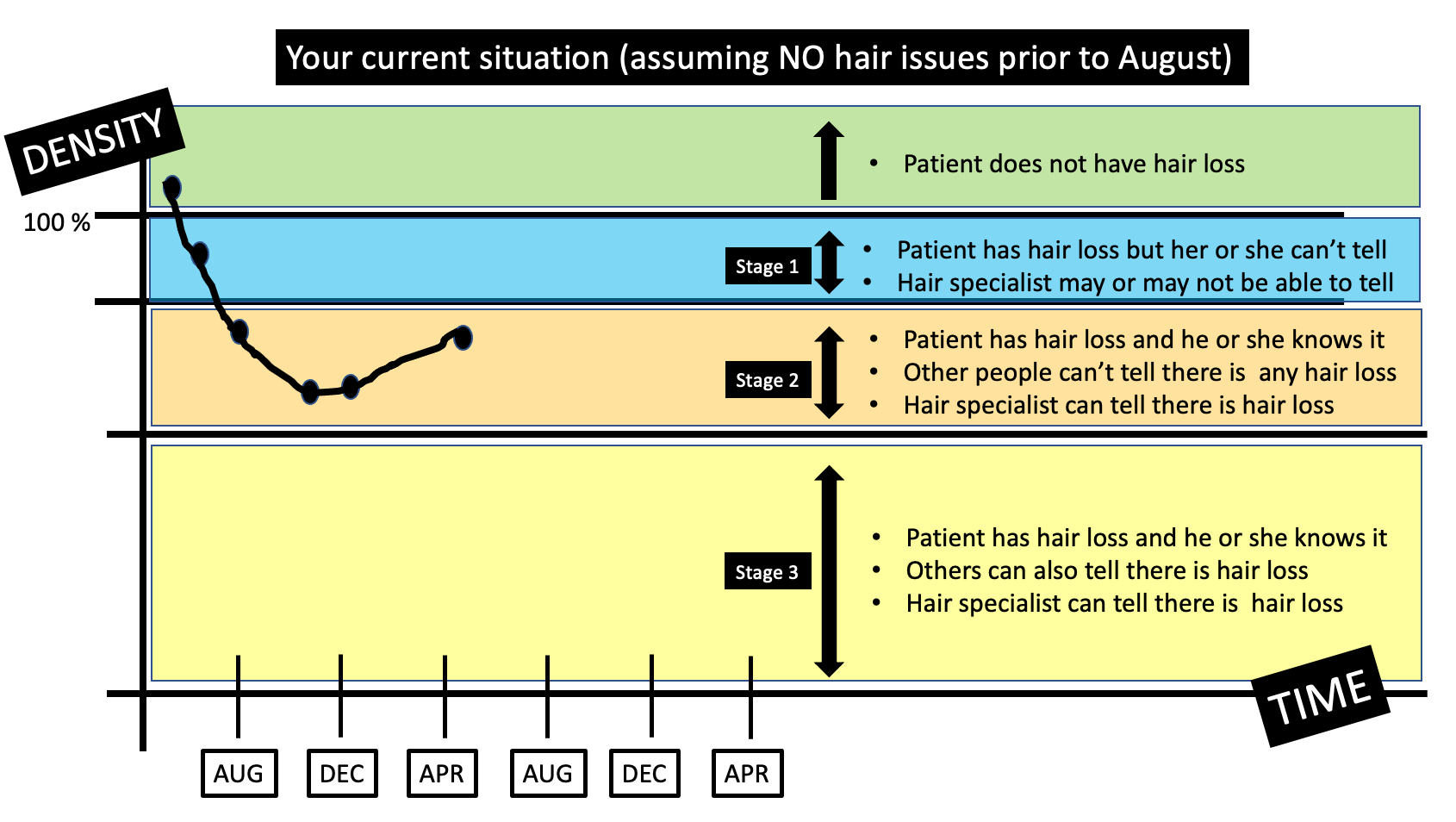
Since the hair shedding began, I experienced massive emotional stress as a result. I was diagnosed with anxiety and depression - which I'm sure I've had for years but got extremely bad once my hair started to fall out. I am thin (weighing only 104lbs) but lost 10 pounds presumably due to stress of the hair loss. I've had two episodes of what was probably telogen effluvium in the past - one was related to low iron (ferritin of 7) back when I was 15, and one episode when I was 18 most likely due to a bad case of the flu. Those episodes only lasted 3-6 months and I grew all of my hair back.
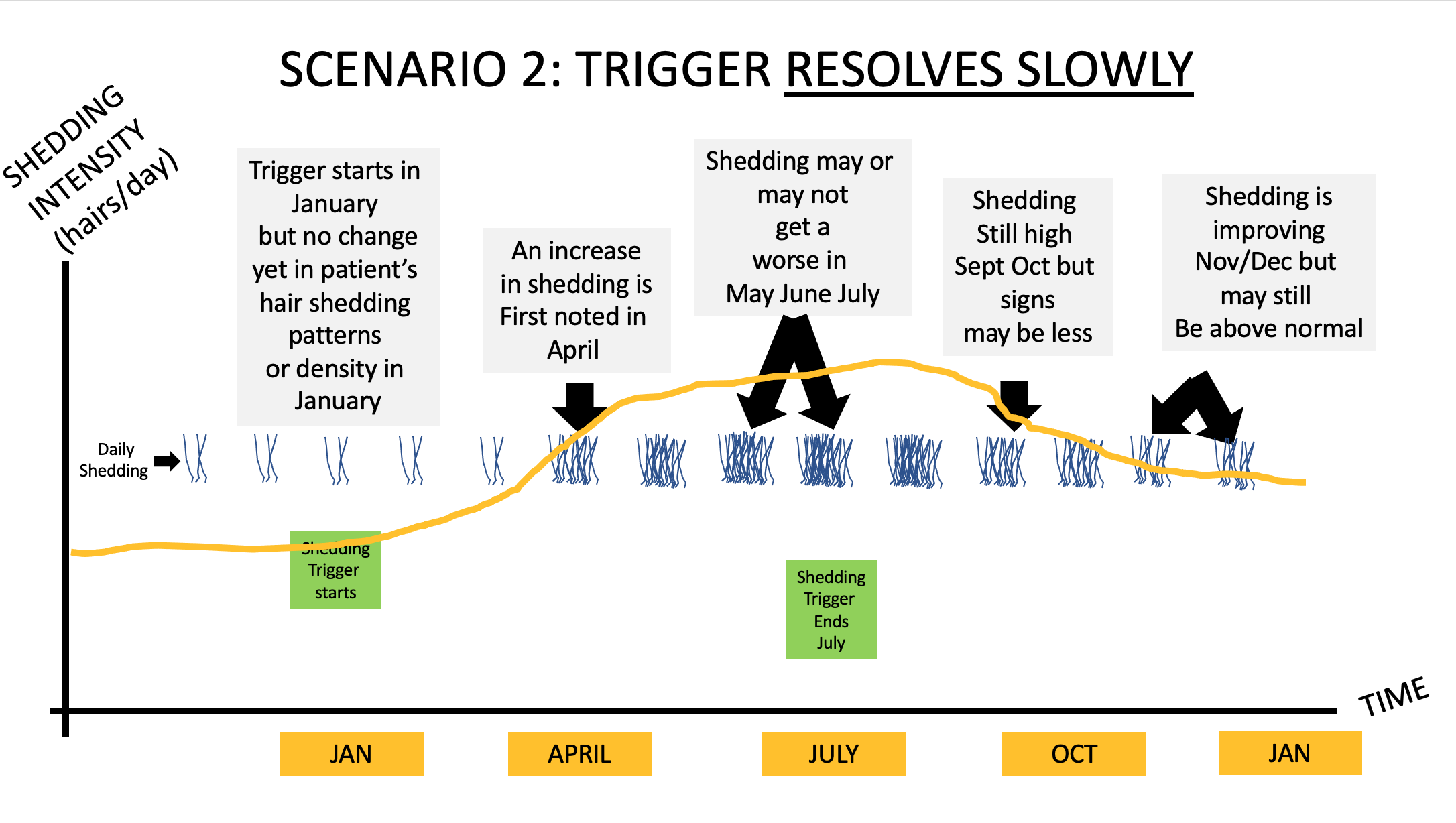
This time, I've been consistently shedding for 6 months with no sign of improvement. My scalp is very tender, sensitive, flaky and itchy still. On an average day, I used to shed maybe 5-10 hairs, now I am shedding roughly 50-150 hairs - which is not normal for me. I'm at a loss for what could be causing this and what I can do about it. Any advice would be greatly appreciated
ANSWER
Thanks for the question.
I’d like to discuss several important things in the question you ask and the information you have submitted.
Before we do go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s story
2) the findings uncovered during the process of the scalp examination including trichoscopy
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
There is lots more to your story that I need. I would want to know about other medications you have started and stopped. I would want to know about other symptoms like joint pains, headaches, fatigue, weight loss, eyebrow changes, eyelashes changes, body hair changes, nail changes, and rashes.
The 2 key questions here in your case are:
a) Is the diagnosis ONLY telogen effluvium … and …. if so what is the trigger?
b) Is this a telogen effluvium with the starting stages of androgenetic alopecia?
Let’s go further into your story.
POINT 1. Many people who take birth control pills shed for the first few months.
First, I think there’s little doubt that at least one of your diagnoses is telogen effluvium. We don’t actually need to debate that. The debate we will get into in a moment is whether anything else is going on.
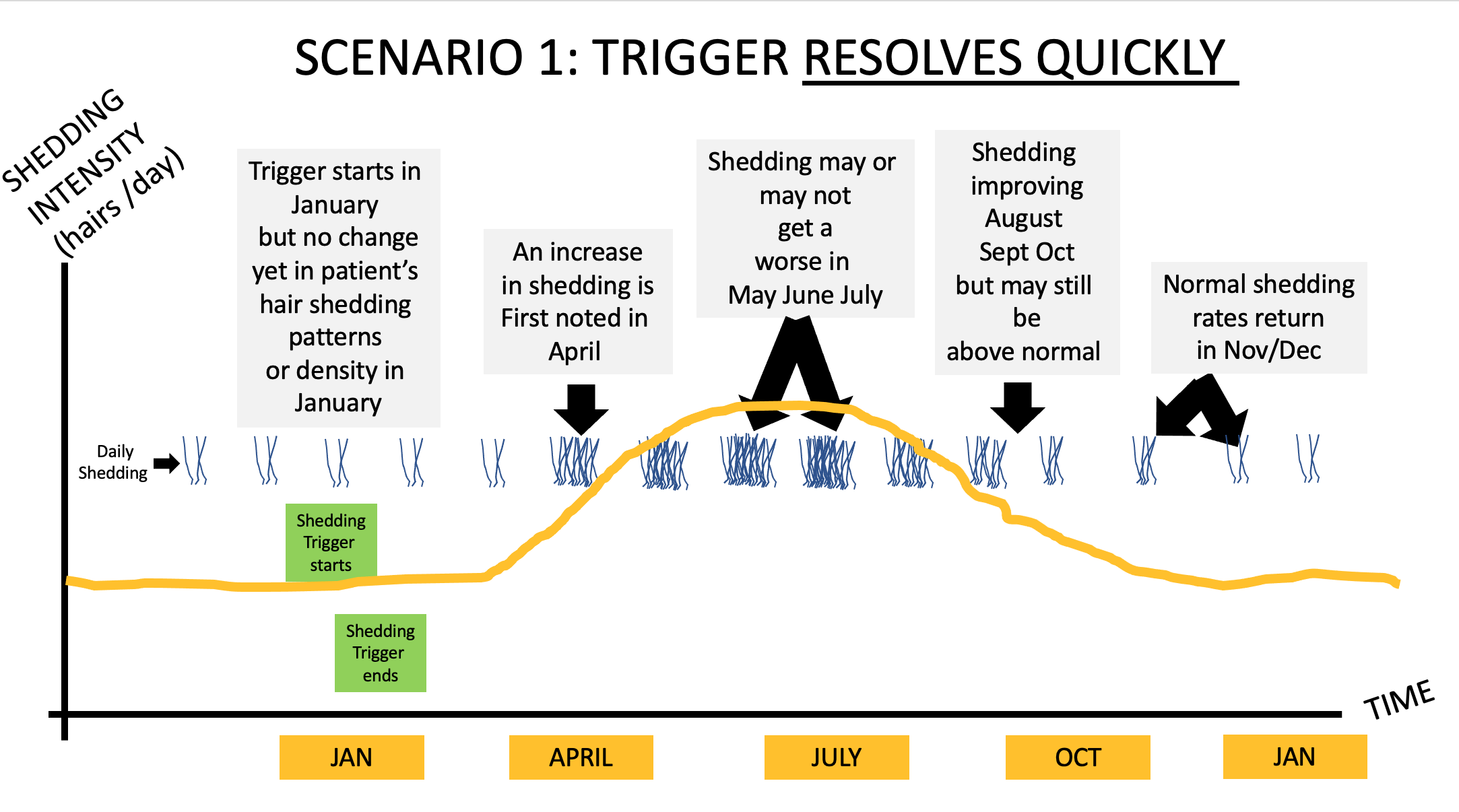
You have several reasons why you could have a telogen effluvium, including starting the birth control pill and starting spironolactone. A large proportion of women shed when starting these treatments, especially birth control pills. The shedding starts 2-3 months after taking the first pill and the shedding lasts 3-6 months provided the pill is continued every day. A lot of women shed when stopping these pills too, especially the birth control pill. The shedding starts 2-3 months after stopping the pill and the shedding lasts 3-6 months provided the pill is not restarted.
So what would I expect to hear from a 21 year old woman who starts spironolactone and then starts a birth control pill? Shedding.
And what would I expect to hear from a 21 year old woman who starts spironolactone and then starts a birth control pill and then stops these pills? Shedding.
What is your story? Shedding.
So in some ways, it’s possible this is entirely consistent with your story.
POINT 2: All patients with hair loss, acne and hirsutism and androgen excess need a proper work up. A work up should be done off birth control.
You have DHEAS 512 (which is 13.9 umol/L in SI units). Any female age 21 with DHEAS 512 and acne and hirsutism and hair loss needs a thorough endocrine work up in my opinion. We need to rule out PCOS and late onset CAH.
With the limited information you have provided here, it would be false to say that you “don’t” have PCOS.
The correct way to say it is more likely “you have a low likelihood of having PCOS.”
Women with PCOS who are thin with low BMI often have regular periods and often have no cysts visualized on ultrasound examinations … but still have elevated androgens. This is a bit more advanced type of knowledge, but I think it’s important especially since you have hyperandrogenism. Anyone who claims there is zero chance you have PCOS is wrong. Anyone who thinks there is a very low chance you have PCOS is correct. I have seen many women with your story exactly who go from being thin to being heavier in their 20s and 30s and ‘develop’ PCOS. I’m not saying that is your case, but sometimes weight gain brings about insulin resistance that then promotes a fuller PCOS clinical presentation.
So what work up do you need? Well, I would advise a proper work up on day 3-5 of your cycle for my own patients that come to see me with a story like yours. The fact that you are off birth control again is a good time to do this. We can’t do these tests when women are on birth control.
The tests that I order on day 3-5 of the cycle for my patients with similar stories are: LH, FSH, estradiol, testosterone, free testosterone, SHBG, glucose, insulin, hemoglobin 1A1c, AM cortisol, prolactin, androstenedione and 17 hydroxyprogesterone, AST, ALT, and cholesterol. These should be done fasting and day 3-5 of the cycle. You have already had your DHEAS measured so there is not a lot of good reason to do this again unless someone suspected levels could be climbing. I would probably include it again for completeness.
What am I looking for in these tests?
a) a high 17 OHP level on day 3-5 that would lead us to a diagnosis of late onset congenital adrenal hyperplasia
b) a high testosterone, high fasting insulin, high LH that would point is towards a PCOS like state
c) A normal prolactin and AM cortisol that reassures us that no other issues are present
In your case, I would want more blood tests if I was your doctor. I would want to know if there is any evidence of insulin resistance that would push me towards PCOS. I would want to know if the other hormones were normal. I would want to know your free testosterone and SHBG. I would want to know your 17 OHP levels to rule out late onset congenital adrenal hyperplasia before moving on.
POINT 3: When it comes to ultrasound examinations, there is a lot that patients don’t realize.
When I hear that a patient had an ultrasound that showed no cysts, my first response is usually that I’m glad to hear that news. But there are a few points to keep in mind. First, it depends on whether the ultrasound examination was a transabdominal ultrasound or transvaginal. There is a big difference in the quality of the studies and what it all means. Transvaginal studies with modern ultrasound techniques are the most helpful. Many people don’t have these studies done. Transvaginal studies can pick up a lot of cysts that the transabdominal can not. Of course, it’s very unlikely this is even an issue with your story but it’s something that we need to keep in mind.
With your ultrasound, I would want to know where it was done (what center? what clinic?) and whether it was transabdominal or transvaginal? What was the volume of the ovaries noted in the report ? Were any ovary measurements more than 10 mL ?
POINT 4: In the early stages of hair loss, TE and AGA can look the same and have the same story. Rarely, they can have a similar biopsy too.
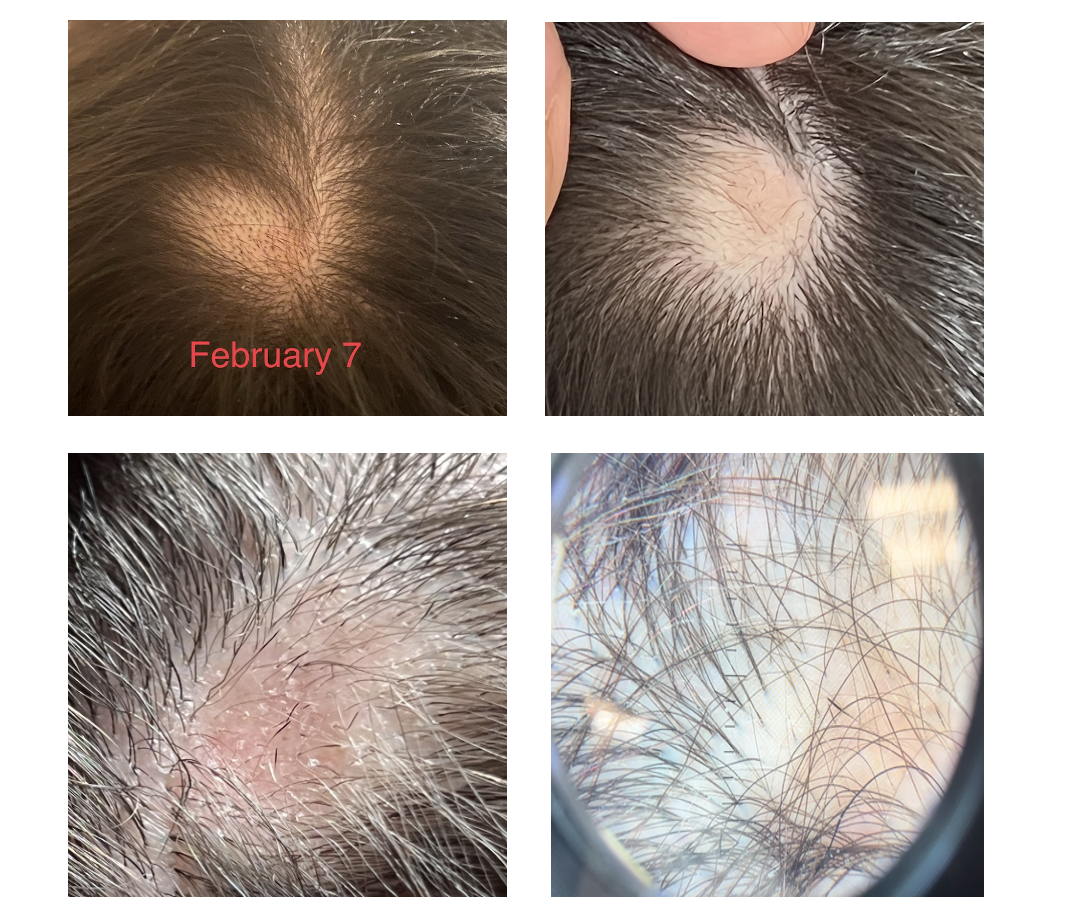
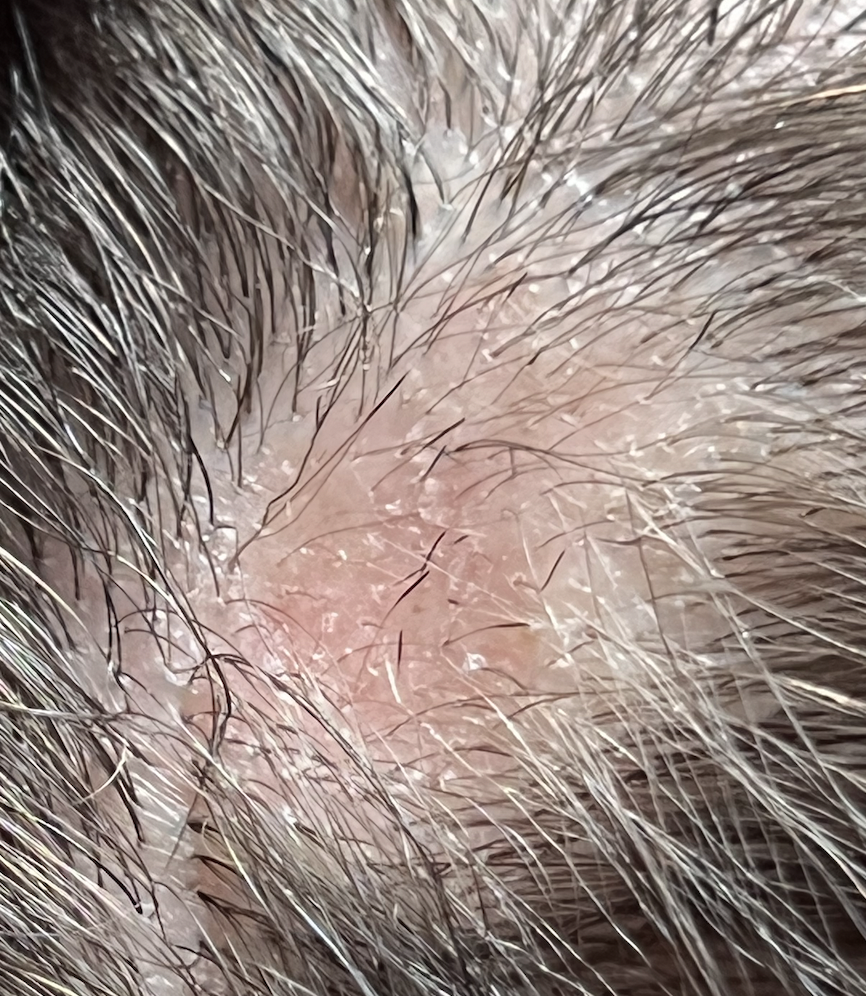
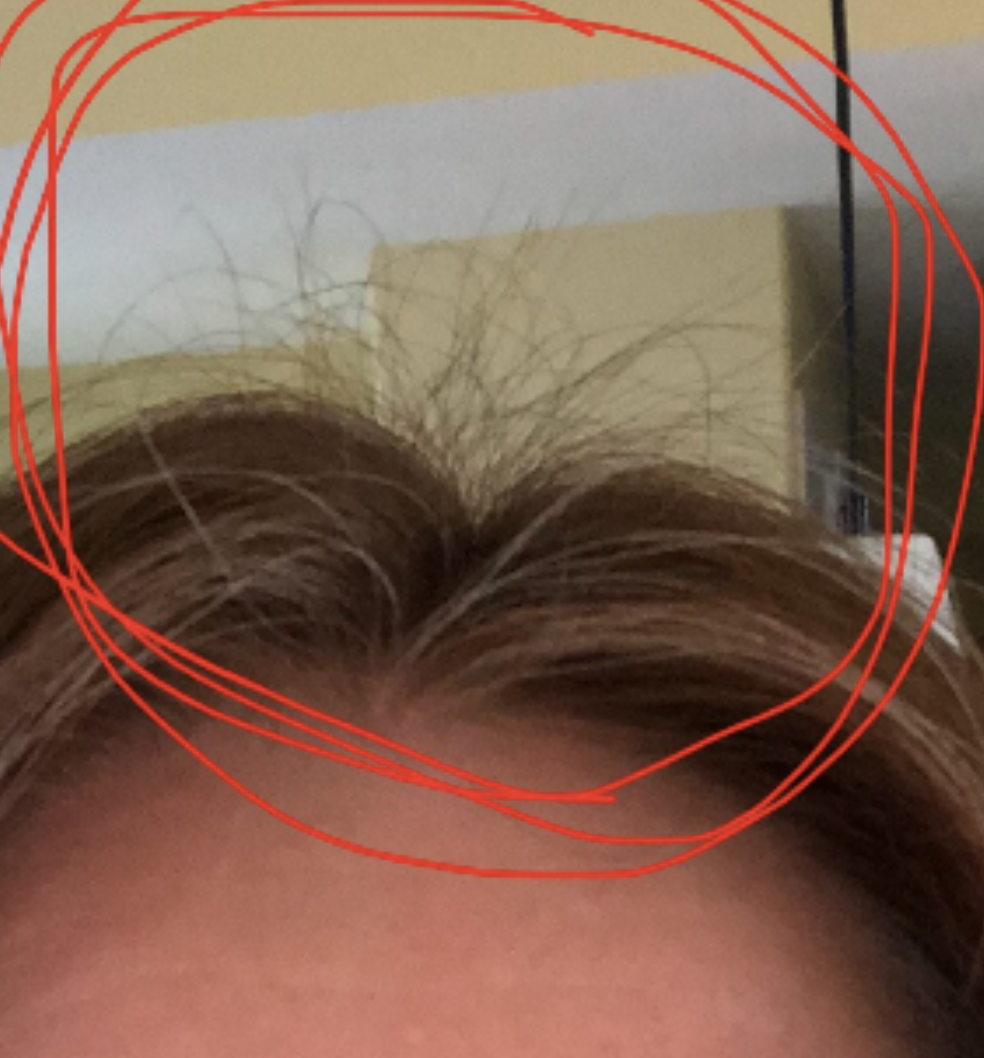
When I look at your photos, I immediately say to myself :
Could this person have AGA?
Could this person have TE?
Could this person have both conditions?
(Also …. whenever we use the word TE, we need to immediate shout out hey could this be diffuse alopecia areata …. but I don’t think that’s what this is. But I include this for completeness of this write up).
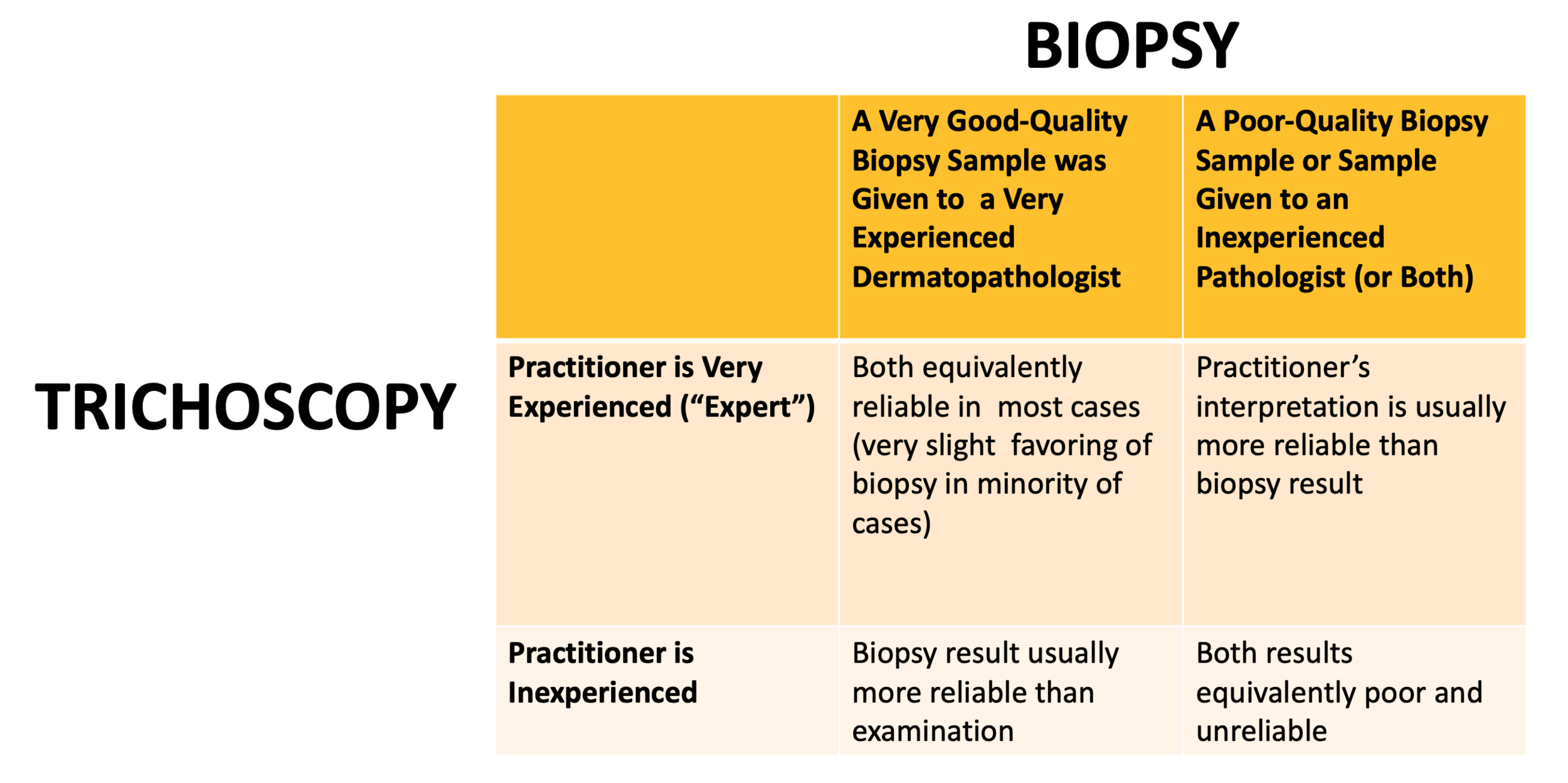
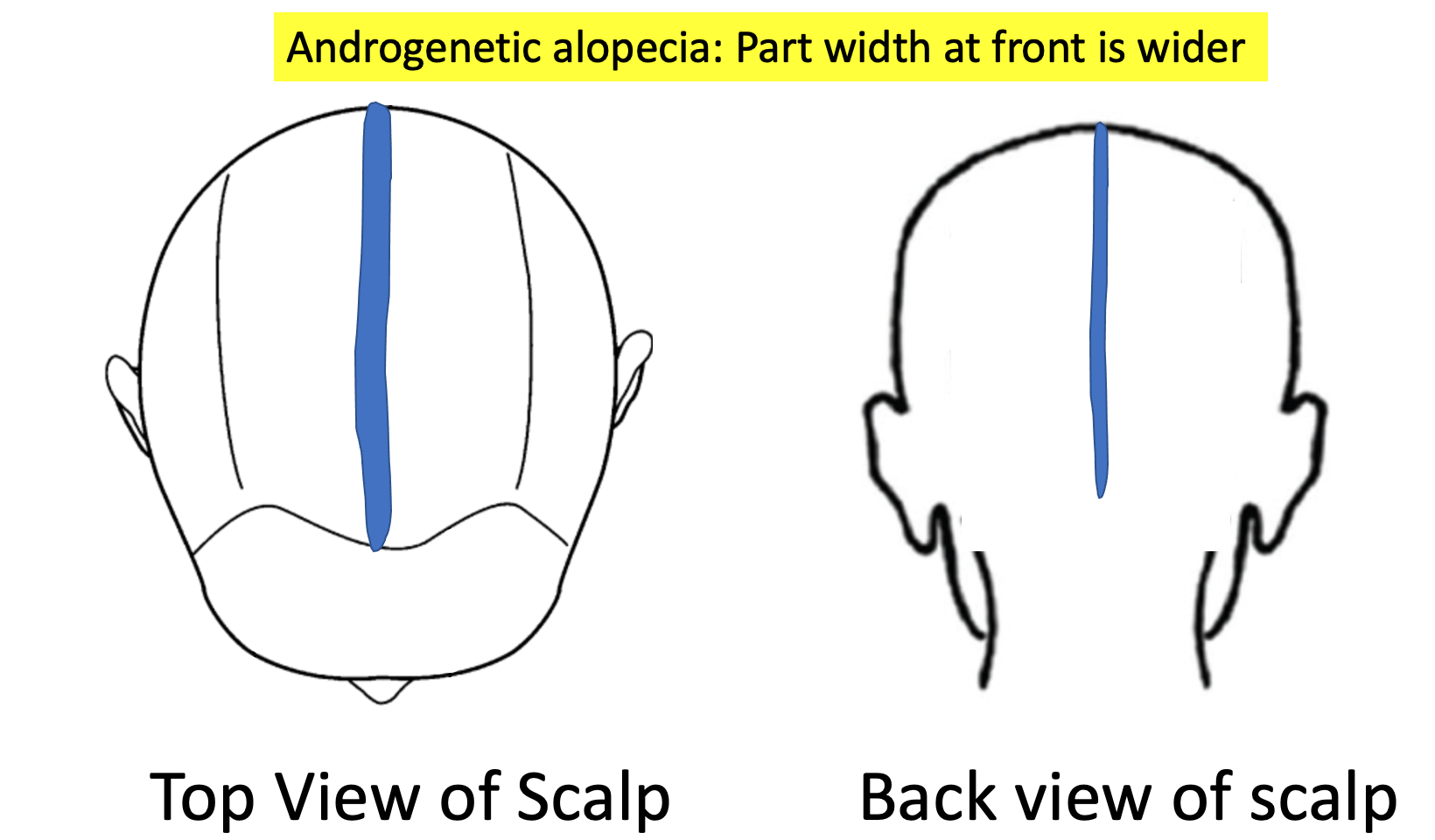
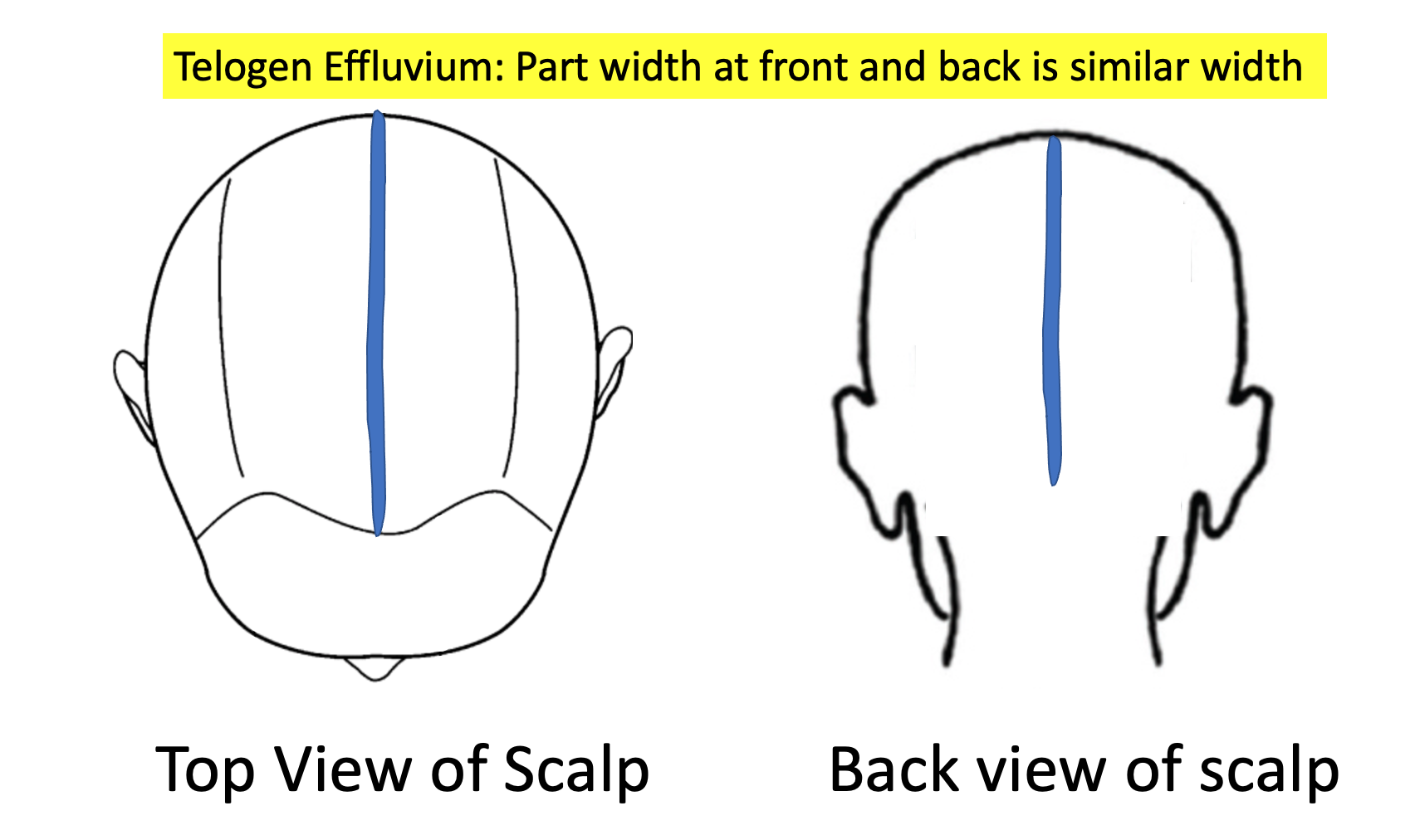
In the early stages TE and AGA look the same. Of course, an up close examination with use of trichoscopy is going to help in your situation. In fact, it’s critical this be done! If the back of the scalp is convincingly thicker than the front of the scalp, I am pushed more towards thinking this could be AGA (with your TE). If the back and front areas are similar density, we are more likely thinking about a sole diagnosis of isolate TE. If there is no evidence of “follicular miniaturization” or variation in the caliber of your hairs when your scalp is examined with trichoscopy, we are likely dealing with an isolated TE. If there is a convincing variation in the caliber of hairs, it could be an early AGA.
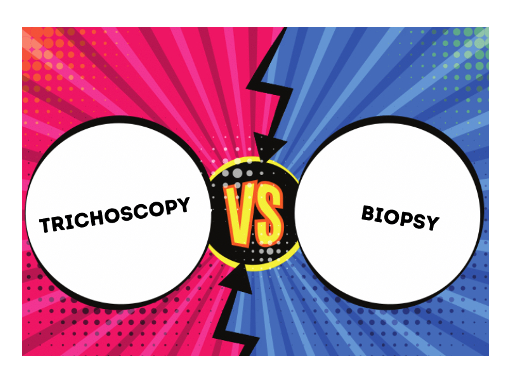
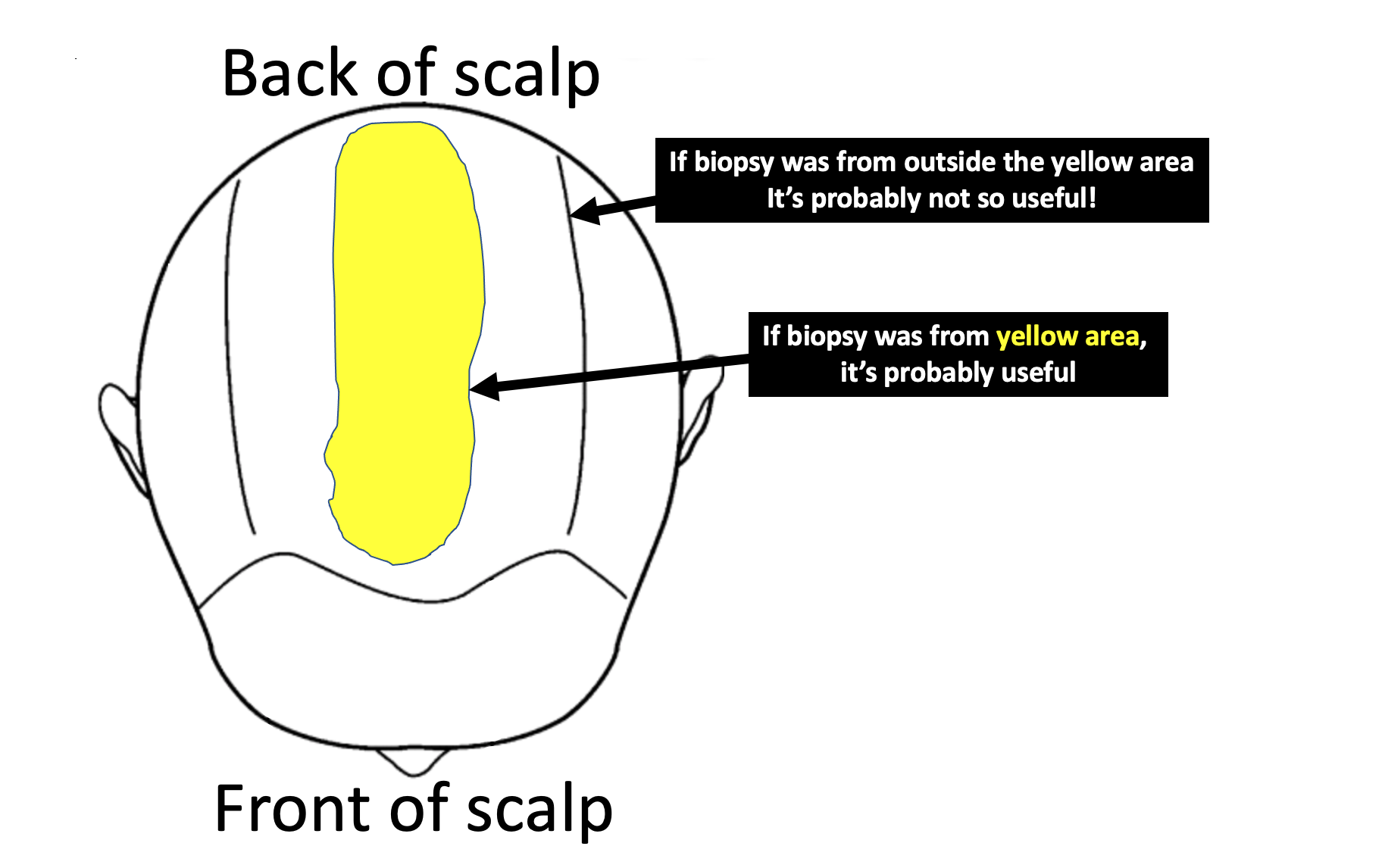
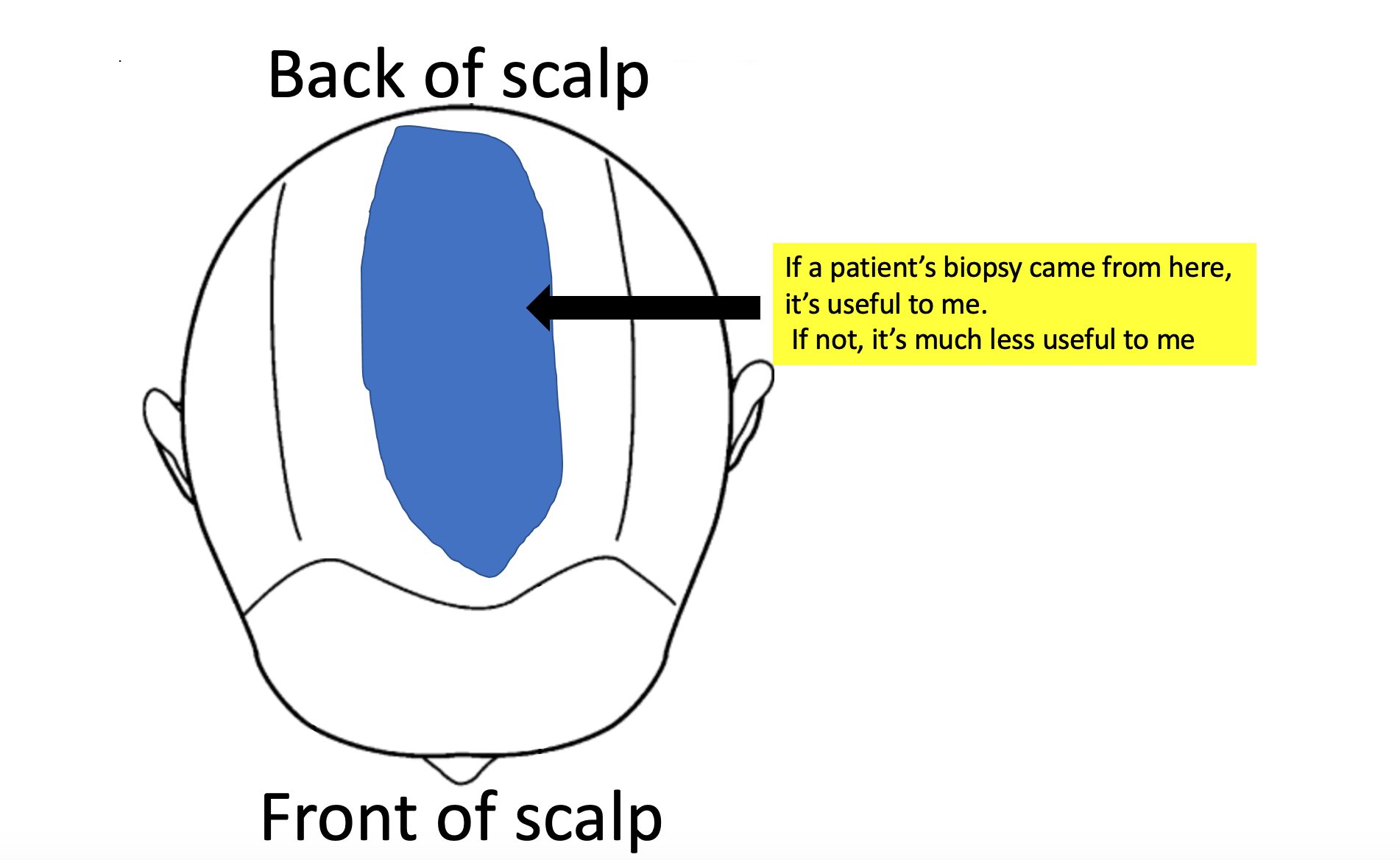
Biopsies can be tricky. There is so much more to doing a biopsy than just doing it and so much more to interpreting a biopsy than just reading the information that comes printed on report. My ability to accurately interpret a biopsy depends where on the scalp it was taken from!. It depends how it was processed (horizontal vs vertical section). It depends who read the biopsy (dermpath vs general path). If a biopsy was taken from the sides or the back or somewhere just to prevent the patient from having a visible scar, then the biopsy is often useless. Biopsies in your case need to come from the top.
Here is where I would need your biopsy to have been taken from for me to feel better about the situation: