Frontal Fibrosing Alopecia (FFA) in Males: A Closer Look at Diagnosis and Treatment
Frontal Fibrosing Alopecia (FFA) in Male Patients: What Things Should We Consider?
Frontal fibrosing alopecia (FFA) is a type of scarring alopecia that causes hair loss along the frontal hairline and sideburns but can also affect the back of the scalp, eyebrows, eyelashes and body hair. For every 100 patients that I see with a diagnosis of FFA, 97 patients are women and 3 patients are male. I am seeing a very slightly greater proportion of male patients in recent years with FFA and so this ratio has changed a bit. Perhaps 5 years ago, I would have said that ratio was 99 to 1 …. but it’s no longer. Of course, we still have no idea what causes FFA so I can’t really give a clear reason why more male patients are being diagnosed with this either.
Let’s take a look at some of the studies that have been published of males with FFA and then I’ll close with some key summary points.
STUDY 1: Ormaechea-Perez et al, 2016
In 2016, Ormaechea-Perez and colleagues studied 12 men (mean age was 75 years) with FFA. About one half of the patients had facial papules, and 83% had androgenetic alopecia (male balding) or hair loss on eyebrows or extremities. Only 25% of the men reported pruritus. The most commonly prescribed treatments were topical corticosteroids in 8 patients (66%) and topical minoxidil in 4 (33%).
In this study facial papules, androgenetic alopecia, and loss of body hair were more often observed in men with FFA than in women. The men in this series were older on average than in other FFA case series in the literature, possibly accounting for the higher prevalence of associated androgenetic alopecia.
STUDY 2: Alegre-Sanchez et al, 2017
In 2017, Alegre-Sanchez reported clinical findings of 12 male patients with FFA. The average age was 47.3 and this ranged from 21 up to 73. These 12 patients had their disease fro an average of 5.6 years with a range 1 to 21 years.
Eyebrow loss was noted in 58 % of patients (i.e. 7 of 12 patients), body hair loss in 42 % of patients (i.e. 5 of 12 patients), beard loss in 42 % of patients (i.e. 5 of 12 patients). Facial papules were noted in 33 % of patients (i.e. 4 of 12 patients). 67 % of patients had androgenetic hair loss (i.e. 8 of 12 patients). None of the 12 patients had hypothyroidism or a positive ANA.
STUDY 3: Tolkachjov et al, 2017
In 2017, Tolkachjov and colleagues performed a study of 7 male patients with frontal fibrosing alopecia to gain a better understanding of how these patients present and what type of hormonal or endocrine abnormalities might be present.
Of the 7 patients, 4 showed loss of the sideburns, 3 showed loss of eyebrows, 2 showed loss of hair in the occipital scalp. 1 patient had hair loss on the legs, 1 had hair loss on the arms and 1 had loss of hair from the upper lip. None of the 7 patients in this study had facial papules and only 1 had androgenetic alopecia. Interestingly, none have evidence of thyroid disease and none had low total testosterone levels (although 2 had evidence of low free testosterone). All patients were ANA negative or only weakly positive.
Of the 7 patients, 4 started systemic therapy with oral hydroxychloroquine and 3 of these patients were able to achieve disease stabilization with use of this drug.
STUDY 4: Peterson et al, 2020
In 2020, Peterson reported findings of 7 male patients with FFA. Average age was 53, and patients ranged from 40 to 67.
Facial papules were present in 4 of 7 patients (57 %), and scalp lichen planopilaris was present in 5 of 7 patients ( 57%). Eyebrow involvement occurred in 5 of 7 patients (57%). Body hair loss noted in 3 of 7 patients (43%). None of the 7 patients had nail involvement.
Androgenetic alopecia was present in 57 % of patients (5 of 7) and alopecia areata was present in 29 % (2 of 7). Oral lichen planus was present in 1 of 7 (14 %). Endocrine issues were not reported so the frequency of low testosterone is not given.
The most common treatments that felt to be involved in achieving disease stabilization were steroid injections (7 patients, 100%), clobetasol (7 patients, 100%), minoxidil (6 patients, 86 %), topical tacrolimus (5 patients, 57%), doxycycline (3 patients, 43%), finasteride 1mg (3 patients 42%), pioglitazone (2 patients, 29%), isotretinoin (1 patient, 14%), hydroxychloroquine (1 patient, 14%), PRP (1 patient, 14 %), low dose naltrexone (1 patient, 14 %).
In this study, the mean time to initial treatment response was 3 months but ranged from 1 month to 1 year. All patients in this study had a complete response with the time to complete response being 5 months (range was from 1 month to 14 months). The mean treatment duration was 14 months with a range, 1 to 51 months).
Overall this was an interesting study. The study highlights that beard hair thinning, eyebrow thinning and body hair loss are sometimes seen in males in FFA and must be asked about by clinicians. Facial papules were common in this particular study but whether they are truly all that common in male FFA will need to be studied further. A large proportion of males with FFA have scalp LPP so this always needs to be evaluated. A full scalp examination is necessary for anyone with any hair loss anywhere but especially in FFA to search for scarring alopecia elsewhere. It’s not surprising that a majority of males had androgenetic alopecia given how common androgenetic alopecia is in the general population and the more advanced age of this study group. What is surprising is the high proportion of males with FFA who also had alopecia areata (2 of 7).
It’s challenging in this study to determine which of the individual treatments actually had a role. Minoxidil, finasteride, steroid injections and clobetasol were commonly used in those who responded to treatment so these likely had an important contribution to disease stabilization. Finally, this study did not evaluate associated endocrine or other issues.
All 7 of these patients had complete responses. I don’t think the follow up was long enough for all patients nor the study size big enough to confidently lead us to believe that FFA in males is easy to treat and that all should respond in an average of 5 months. I think this can not be concluded here.
What can be concluded is that good options exist and that typical options used for women with FFA are very much a part of the treatment algorithms for males.
STUDY 5: Westphal et al, 2021
The most recent study was a study of 35 patients with frontal fibrosing alopecia. This is one of the largest studies of male FFA to date. What was particularly nice about this study is that the authors included a control group of 60 patients without FFA. This control group allowed the authors to better understand some of the risk factors.
Of the 35 males with FFA, 74 % had involvement of the frontal hairline (i.e. 25 of 35 patients), 68 % had eyebrow loss (i.e. 23 of 35 patients), 32 % had involvement of the beard (i.e. 11 of 35 patients), 35 % had sideburn hair loss (i.e. 12 of 35 patients) , 18 % had occipital hair loss (i.e. 6 of 35 patients). Facial papules were noted in 21 % (i.e. 7 of 35 patients), hair loss was noted on the lower limbs in 44 % (i.e. 15 of 35 patients), on the upper limbs in 26 % (i.e. 9 of 35 patients), and on the chest in 3 % (i.e. 1 of 35 patients).
When the authors compared the use of facial moisturizers, sunscreens or other skin care products in men with FFA compared to controls, there was no statistically significant different in patterns of use.
STUDY 6: Lobata-Berezo et al, 2021
In 2021, Lobata-Berezo published a study of 39 male patients with FFA. 76.9 % of patients (i.e. 30 of 39) had androgenetic alopecia. The mean age was 69 (range 46-89 and patients) and patients had their FFA for an average of 7. 1 years.
Sites of involvement were somewhat similar to other studies. Sideburn hair loss was present in 89.7% of patients (i.e. 35 of 39), beard hair loss in 74.4 % (i.e. 29 of 39), eyebrow loss in 94.9 % (i.e. 37 of 39), body hair loss in 59 % (i.e. 23 of 39), occipital hair loss in 23 % (i.e. 9 of 39), and eyelash loss in 2.6 % (i.e. 1 of 39). Facial papules were noted in 33 % of patients (i.e. 13 of 39). Depression of the forehead veins was noted in 12.8 % (i.e.5 of 39).
There were several important associations that were studied. Hypothyroidism was noted in 5.1 % of patients (i.e. 2 of 39), benign prostate enlargement was noted in 33 % (i.e. 13 of 39), and prostate cancer was noted in 15.4 % (i.e. 6 of 39). 3 of the patients with prostate cancer had undergone treatment with antiandrogen drugs including bicalutamide, goserelin and triptorelin before the start of the FFA. Rosacea was noted in 30.8 % of patients (i.e. 12 of 39).
The Lobato-Berezo study did not assess hormone levels in much depth. Of a small number of males who did have hormone testing most had normal hormones. A small number of those tested had low testosterone but given that 10 % of healthy males in the 40s have low testosterone anyways (rising to 20 % in the 60s and 30 % in the 70s), it’s difficult to know if really there is all that much of a difference in testosterone levels in males with FFA. It doesn’t seem to be.
STUDY 7: Doche et al, 2021
Doche and colleagues reported the clinical findings of 33 male patients with FFA. The average age was 53.1 years with a range 24-82). 57 % of patients were normal weight. 36.3 % were overweight and 6.1 % were obese. 63.6 % of patients had androgenetic hair loss.
90 % hair frontal hair loss (i.e. 30 of 33 patients), 69.7 % had beard hair loss (i.e. 23 of 33 patients), 69.7 % had sideburn hair loss (i.e. 23 of 33 patients), 66.6 % had eyebrow hair loss (i.e. 22 of 33 patients), 21.2 % had occipital hair loss (i.e. 7 of 33 patients), and 30.3 % had axillary hair loss (i.e. 10 of 33 patients). Scalp LPP was noted in 27.2 % of patient (i.e. 9 of 33 patients), and 6 % had cutaneous lichen planus (i.e. 6 of 33 patients). None of the patients in this study had oral or nail lichen planus. Facial papules were noted in 42.4 % of patients (i.e. 14 of 33 patients),
There were several disease comorbidities that were evaluated. Hypertension was noted in 24.2 % of patients, depression was noted in 12.1 % and hypothyroidism was present in 9 %. Rosacea was noted in 33.3 % of patients (i.e. 11 of 33 patients). This was not a case controlled study design so we don’t really know if these numbers differ from the general population.
A very small proportion of the patients in the study had hormonal abnormalities but the study was too small and not controlled to really assess the precise significance of these observations. It was interesting that a large majority of patients who did have hormonal abnormalities were obese.
STUDY 8: Bernardez et al, 2021
Bernardez and colleagues studied beard hair loss in 20 males. The average age was 52 with a range from 30 to 72). Androgenetic hair loss was present in 70 % of patients. The lateral cheek was a common area of hair loss with 100 % of patients affected. The sideburn was affected in 90 % of males. The moustache was affected in 90 % of males, although the very central area was often spared. The chin area was affected less commonly with only 60 % reporting hair loss. Facial papules were present in 70 %.
STUDY 9 : Rayinda et al, 2021
Rayinda and colleagues reported data on 17 males with FFA. Eyebrow loss was present in 65 % of patients (11 of 17 patients), eyelash loss in 12 % (2 of 17 patients)., limb hair loss in 59 % (10 of 17 patients), and facial hair loss in 65 % (11 of 17 patients). Facial papules were present in 47 % ( 8 of 17 patients). Oral lichen planus was present in 6 % of patient (1 of 17 patients), vitiligo in 6 % (1 of 17 patients) and lichen sclerosus was present in 6% (1 of 17 patients). Androgenetic alopecia was noted in 18 % (3 of 17 patients). Lab abnormalities were studied. Low testosterone was present in 18 % (3 of 17 patients), abnormal SHGB in 24 % (4 of 17 patients). Overall, the data are similar for the most part to the other FFA studies in males. However, this study does highlight the possibility of oral lichen planus and lichen sclerosus in male patients with FFA.
FINAL SUMMARY & COMMENTS
POINT 1. Studies of FFA in males to date are small but patterns are emerging.
These studies are small and somewhat inconsistent. This reflects the different populations studied and the sizes of the studies. FFA in males is fairly uncommon so it’s hard to recruit large numbers of patients.
What do I mean by inconsistent?
Facial papules were rare in the Tolkachjov study yet common in the Ormaechea- Perez study and Peterson study. Furthermore, androgenetic alopecia as a second diagnosis was common in the Ormaechea-Perez study and Peterson study yet rare in the Tolkachjov study. The Peterson study suggested males with FFA are younger than most women with FFA yet the Ormaechea-Perez study suggested that males with FFA are actually older than most women with FFA.
Only the Tolkachjov study sought to understand the potential endocrine issues in males with FFA. It appears that endocrine issues are fairly rare in males with FFA but again this really has not been well studied. For example, although hypothyroid disease occurs in 15-23 % of female patients with FFA, it does not appear males have quite that degree of association. The Lobato-Bereza study suggested that just 5 % of males with FFA had hypothyroidism. Similarly, about 1/3 of women with FFA have low androgens - this does not seem to be the case in men in these small studies. Most males with FFA seem to have androgen profiles that match males of the general population. More studies of course can confirm this but it does not seem that male FFA has a clear underlying endocrinopathy that we should go looking for.
It still probably makes sense to order CBC, TSH, testosterone, free testosterone, cholesterol, PSA in males with FFA. TSH is probably the most evidenced based one of this list, but these are the tests I order. I like to order ANA, AST, ALT, creatinine, urinalysis so that we’re ready in the future if we need to consider more advanced therapeutics. It’s unlikely to find a relevant ANA but given a seemingly very rare link between some FFA and discoid lupus, I like to include it. Again, probably the only evidence based one to order is still TSH.
Patterns are emerging for males with FFA, including:
1. Androgenetic alopecia is common in males with FFA
2. Beard, eyebrow and sideburn hair loss is fairly common.
3. Facial papules are often seen.
4. Leg hair loss is often seen.
5. Most males with FFA are healthy.
6. Blood tests usually return normal although checking TSH is useful.
7. Male FFA can affect men at young ages.
2. A really, really good history is needed with suspected male FFA.
In my opinion, a proper history is needed to understand where the hair loss is occurring and whether any clear endocrine or autoimmune issues exist. Medication history is important as hormone blocking agents in my opinion are an important contributor to some males in older age groups especially those on hormone blocking cancer drugs. A history of autoimmune disease should be elucidated as many patients with FFA have a family history of various autoimmune diseases.
Comorbidities need to be considered in males with FFA given that conditions like vitiligo, lupus, psoriasis are more common in women with FFA than women who do not have FFA. We need to ask alot of good questions!
3. We need to at least consider FFA/LPP in all males with beard/facial hair loss.
It’s important to understand and document whether there has been eyebrow, eyelash, facial or body hair loss. Beard hair loss in FFA is extremely common and it’s one of the earliest changes for many men. For women with FFA, the eyebrows seem to be one of the earliest changes. While this can be true for males, the sideburns and beard hair are often involved early on in the disease.
It’s really important to have one’s radar on for FFA/LPP whenever they see beard hair loss. Now of course, most males with beard hair loss will have alopecia areata. But unless one is thinking about FFA, you’ll miss these early cases.
Males with beard hair loss must trigger the clinician to ask “Could this be alopecia areata or could this be scarring alopecia?
There are two types of beard hair loss in FFA. One is patchy - just like alopecia areata. The upper lip moustache area is often affected too. The second is a diffuse thinning of hair. The patient just feels their density is less than before.
4. We need to at least consider FFA/LPP in all males with leg hair loss.
Leg hair loss is a feature of male FFA. Just like beard hair loss, it’s often a presenting issue in males with FFA. Leg hair loss is often misdiagnosed. We often bail out to diagnosing leg hair loss as aging, or frictional in nature, or peripheral vascular disease. Luckily, these are often the reasons so choosing one of these is not a bad idea.
The reality is that we need to keep FFA on the list. I am not of the opinion that every 4 mm biopsy of leg FFA is going go beautifully capture the diagnosis of a lymphocytic scarring alopecia. It does not. So we certainly need to get out of the mindset that “I did a biopsy and it didn’t show much so it can’t be FFA.”
The best way to diagnose hair loss is with a full history and good examination. Leg hair loss with arm hair loss that is of recent nature together with other features like bilateral sideburn loss or beard loss is pretty convincing for FFA. The more symmetric the whole thing is the most convincing the diagnosis is probably FFA.
5. We can’t be afraid to consider male FFA in males 20-30 years of age.
Male FFA occurs at younger age groups that female FFA. IT can be challenging to distinguish a receding hairline that is red from seborrheic dermatitis from a receding hairline that is red from FFA. Features such as eyebrow hair loss, sideburn hair loss, body hair loss, facial hair loss will be helpful to solidify the diagnosis. Of course a biopsy is likely to be of help in many cases.
6. We need to be on the lookout for hair loss patterns in males undergoing advanced prostate cancer treatments.
It really should come as no surprise that hormone blocking drugs can contribute to FFA. For women with FFA, tamoxifen is a potential risk factor to FFA. The Lobato-Bezero study reminds us that we need to keep studying hormone blocking drugs. I have little doubt there will be a link of some kind between advanced prostate cancer drugs and FFA. It’s important to be aware that this does not mean that patients who take these drugs will develop FFA. Not at all. It just means that there is probably a slightly increased chance compared to people who don’t take these drugs. For example, if 1 in 6000 women in the general population develop FFA, it could be possible that 1 in 500 or 1 in 1000 women using tamoxifen develop FFA-like features. We need studies to confirm or refute this. If there truly is a link of this kind, most clinicians will never draw a link unless good studies are done simply because most clinicians don’t see large enough volumes of patients. Rare diseases need meticulous collaborative studies. The same is probably true with many of these prostate cancer drugs. Good studies are needed to confirm a link. Given that FFA in males is rare and drugs contributing to FFA in males is probably pretty rare too - good studies will be needed to get answers. I suspect there is probably a link of some kind with some advanced prostate cancer drugs. How strong the link is will need some pretty good studies.
7 . We need to ask about oral and genital LP.
When taking a history from patients, we need to ask about oral and genital lichen planus as well as nail LP. These are not common in published studies that have been done so far but I don’t think we fully understand these issues well enough yet. It’s becoming clear, in my opinion, that we probably miss a fair number of cases of vulvar lichen planus and lichen sclerosus in women with FFA. It’s possible for men with FFA that these issues are also very much underdiagnosed. Studies are small but the key point is that we need to be on the lookout for these issues. If there are any concerns about genital itching, burning, pain, pigmentation changes, growths, bleeding, referral to a specialist is helpful to confirm the diagnosis.
8. Treatment of Male FFA Follows A Similar Plan to Women with FFA - At Least for Now!
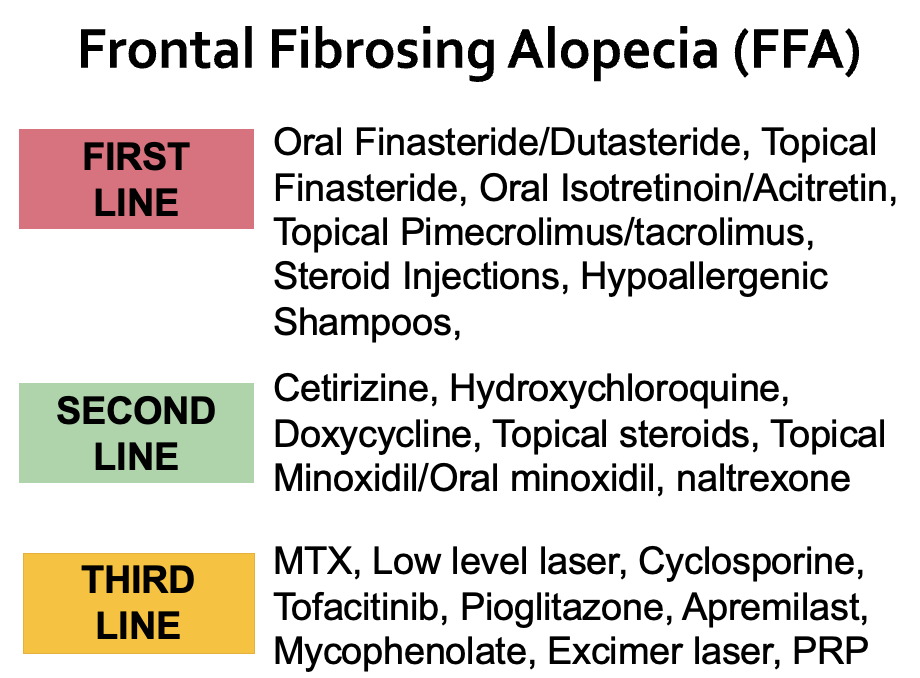
I think of treatment in terms of first-line, second-line and third line options. The goal is to start with a few first line agents that are most likely to help based on the patient’s history and concurrent conditions.
Topical steroids, steroid injections, finasteride/dutasteride, pimecroliumus/ tacrolimus, isotretinoin are very much a part of an initial (first line) approach to treating FFA in males. Hydroxychloroquine (Plaquenil), doxycycline, cetirizine, minoxidil can be added on very early in the course if needed. In many ways, the first and second line agents for FFA are somewhat bundled together. I don’t want to start 10 treatments if 2 or 3 will work but I have a low threshold to bring on board another treatment.
I typically start with a topical steroid, pimecrolimus (or tacrolimus), steroid injections and topical or oral finasteride. Hypoallergenic shampoos are a must. I will quickly move to adding either isotretinoin or doxycycline (not both) depending on the scalp and body hair loss. if not helping, I may add either hydroxychloroquine to doxycycline or stop isotretinoin and start doxycycline.
It’s pretty rare that we need to go on to using third line agents in FFA.
Personally, I am a big fan of getting male FFA patients off all allergen containing products. Hypoallergenic shampoos are best added early in the treatment plan and hair gels, pastes, sprays need to be abandoned or switched to hypoallergenic versions. I do think that hypoallergenic scalp products are very important for male patients with FFA. It’s something I’ve witnessed many times. Options for my patients include Vanicream Free and Clear (regular and antidandruff), SEEN Fragrance free shampoo, Sensinol, AFM SAFE CHOICE, EXEDERM SHAMPOO, NO NOTHING and NATURE CLEAR.
PRP, Exosomes, microneedling, hair transplants, hair and nail supplements have little role in the initial management of active FFA in my opinion.
Questions that Still Need Answering for Male FFA
a) Is fertility altered in male FFA?
There is still many questions that we don’t know much about. Although early menopause is thought to be a feature of some female patients with FFA, we don’t know if fertility is impacted in male FFA. The role of FSH and sperm counts is completely unknown for males who wish to have a family.
b) What is the incidence of low testosterone and other endocrine issues in male FFA?
A proportion of women with FFA have androgen deficiency. We don’t know the exact incidence in males but studies like the Lobata-Berezo study would seem to suggest most males with FFA have fairly normal hormone levels compared to the general population. It’s a bit of a stretch right now to try to tie in a major hormonal abnormality in males with FFA. If one is going to propose that we need bigger studies with control. Hormone test results are all over the place even in healthy patients.
In my opinion, it’s probably worth routinely testing testosterone levels in males with FFA until we learn more.
In general though, thyroid disease in women with FFA is increased quite a bit above the levels in the general population. To date, it would seem that the frequency of thyroid disease is lower in men with FFA than women with FFA. . However, we don’t really know if the incidence of thyroid disease overall is higher in men with FFA than men without FFA. For this reason, TSH should be tested.
c) What is the incidence of rosacea in male FFA?
It’s clear there is a risk of ‘rosacea’ (or what I believe is better termed a “rosacea-like” disorder) in women with FFA. Whether the incidence of rosacea truly increased in males with FFA is unknown but it certainly may be. Many of my own male patients with FFA have rosacea. This form of rosacea often responds to laser therapies.
d) What is really the best treatment plan for male FFA?
We don’t really know the best treatment plan moving forward once FFA is diagnosed. We have no reason to believe that treatment in males is different than females - but that’s simply a guess. The above treatment protocol offers a guide.
I think male FFA is not necessarily difficult to stabilize but the literature to date would suggest it’s quite easy and straightforward. The studies above suggested that every patient responded to treatment. I don’t think that’s quite accurate. Treatment for FFA is successful in many with a good solid plan but not universally. Follow up in these studies is really short (really really short) and I think one really needs to follow a patient 2-3 years before you can be convinced FFA is quiet.
e) What is the incidence of oral, genital and nail lichen planus in male FFA?
As I have discussed above, we really don’t know all these answers. Most studies suggest these incidence of oral, nail and genital lichen planus is pretty rare in males with FFA. However, the incidence is possibly more common than we currently believe - given that we currently believe it’s not common at all.
f) What other “co-morbidities” are present in male FFA?
We don’t really know all the co-morbidities might exist. Heart disease appears reduced in women with FFA and LPP but whether this is the case in males is unknown. Similarly whether meibomian gland dysfunction is common in male FFA will need to be determined. It is a concern among many women with FFA.
Psoriasis, lupus and vitiligo are markedly increased among women with FFA according to a 2021 study by Trager and colleagues. We’ll just need to wait to see if male FFA truly has these similar associations or not.
One study by Peterson and colleagues suggested alopecia areata is more common in male FFA than we might have otherwise expected. We’ll need to figure out if this is really the case in larger studies. Most studies other than the Peterson study have not really shown this. Many male patients with FFA do have very strong family histories of autoimmune disease so I suspect there may be a connection.
Rosacea and male balding are the most closely associated.
Below is a table of common co-morbidities in women with FFA and LPP
g) Are facial forehead grooves (depressed forehead veins) more common in FFA?
Linear grooves or ridges in the forehead are sometimes seen in FFA. It has been described in women with FFA. Whether it is a frequent finding in male FFA is not clear. Depression of the forehead veins was noted in 12.8 % of patients in the Lobata-Berezo study.
h) Do we really need to advise patients to avoid sunscreens?
To date, the evidence linking sunscreens and facial moisturizers to FFA is getting weaker and weaker. There is a faint whisper of support from some. The reality is that whole lot of good studies suggest there is no link. There is only one study of sunscreen use in male FFA - and that is the 2001 Westphal study. As reviewed above, there was no association between sunscreen use and facial moisturizers in that study.
REFERENCES
Alegre-Sanchez et al. Frontal fibrosing alopecia in male patients: a report of 12 cases. J Eur Acad Dermatol Venereol. 2017 Feb;31(2):e112-e114.
Bernardez C et al. Beard loss in men with frontal fibrosing alopecia. J Am Acad Dermatol. 2021 Jan 20;S0190-9622(21)00179-1.
Doche I et al. Clinical features and sex hormone profile in male patients with frontal fibrosing alopecia: A multicenter retrospective study with 33 patients. Journal of the American Academey of Dermatology. 2021.
Lobata-Berezo et al. Frontal fibrosing alopecia in men: A multicenter study of 39 patients. Journal of the American Academy of Dermatology. 2021
Ormaechea-Perez N et al. Frontal Fibrosing Alopecia in Men: Presentations in 12 Cases and a Review of the Literature. Actas Dermosifiliogr. 2016 Dec;107(10):836-844.
Peterson et al. Frontal fibrosing alopecia in males: demographics, clinical profile and treatment experienceJ Eur Acad Dermatol Venereol. . 2020 Feb;34(2):e101-e104.
Rayinda T et al. Clinical characteristics of male frontal fibrosing alopecia: a single-centre case series from London, UK Br J Dermatol. 2021
Tolkachjov et al. Frontal fibrosing alopecia among men: A clinicopathologic study of 7 cases. Journal of the American Academy of Dermatology 2017; 77:683-90
Trager MH, et al. Medical comorbidities and sex distribution among patients with lichen planopilaris and frontal fibrosing alopecia: A retrospective cohort study. Am Acad Dermatol. 2021. PMID: 32781188 No abstract available
Vañó-Galván S et al. J Am Acad Dermatol. 2015 Jun;72(6):1087-8.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.