Lichen planopilaris: What works and when do the treatments start helping?
Lichen Planopilaris: Treatment Options
Lichen planopilaris (LPP) is a type of scarring alopecia that affects both men and women. It can affect any region of the scalp although the central areas of the scalp tend to be most affected. There are a variety of different ways that LPP can announce its arrival and so there is no standard way.
Typically, patients with LPP first develop hair shedding accompanied by some degree of scalp discomfort. Scalp itching, burning and pain are often experienced by patients with LPP. Some patients however are quite asymptomatic.
The Clinical Evaluation: What is needed when evaluating a patient with LPP?
Evaluation of the patient with suspected LPP requires collecting information from the patient on a variety of different things including: the precise locations they feel the hair is being lost from (scalp, eyebrows, lashes, body hair), symptoms, actions they feel help improve symptoms. Overall health should be ascertained as should a family history of autoimmune diseases. The scalp should be examined to document the areas of hair loss. Up close examination using dermoscopy is important to document the presence or absence of perifollicular erythema, scaling and confirm the the type of hair loss is truly scarring and that follicular openings are lost.
The Scalp Biopsy: Is it needed?
In typical and classic cases of lichen planopilaris, a biopsy may or may not be needed. Many physicians do choose to biopsy to confirm the disease. However, in classic cases, a biopsy does not usually add any additional benefit. If performed, a biopsy must be taken from a hair containing region of the scalp and ideally an area which has the features of LPP.
The biopsy will show loss of sebaceous glands and lymphocytic infiltration in the hair follicle sheath in a very specific manner known as lichenoid infiltration. Hair follicle cells will show evidence of death (necrosis, apoptosis). The loss of sebaceous glands and hair follicle cell death are the two most important features of the biopsy to search for in the report. The presence of lymphocytic infiltration in the upper part of the hair follicle and the presence of concentric fibrosis (scarring) alone are suggestive of LPP but by no means proof. These findings may be present in non scarring alopecias such as androgenetic alopecia as well.
Blood tests: Which ones?
The exact blood tests that are needed depends on the patient’s story and the findings on examination. In other words, the blood tests required for one patient with LPP may differ slightly from another patient.
Standard blood tests in the setting of suspected LPP include:
CBC - complete blood counts
TSH - thyroid stimulating hormone
Ferritin - iron stage levels
ESR - erythrocyte sedimentation rate
ANA - antinuclear antibodies
Cholesterol profiles - including LDL, HDL and non LDL
Vitamin D - 25 hydroxy-vitamin D levels
Treatment Options for Lichen Planopilaris
There are a variety of treatment options available for LPP. In fact, taken together there are well over 25. However, several options would be considered standard options and have the best medical evidence. These options include topical steroids, topical calcineurin inhibitors, steroid injections, and oral medications such as hydroxychlorqouine, doxycycline, methotrexate, cyclosporine and mycophenolate. Other options that can be considered (especially if these options do not work) include low level laser, low dose naltrexone, pioglitazone, excimer laser, anti-androgens, azathioprine, tofacitinib, and isotretinoin,
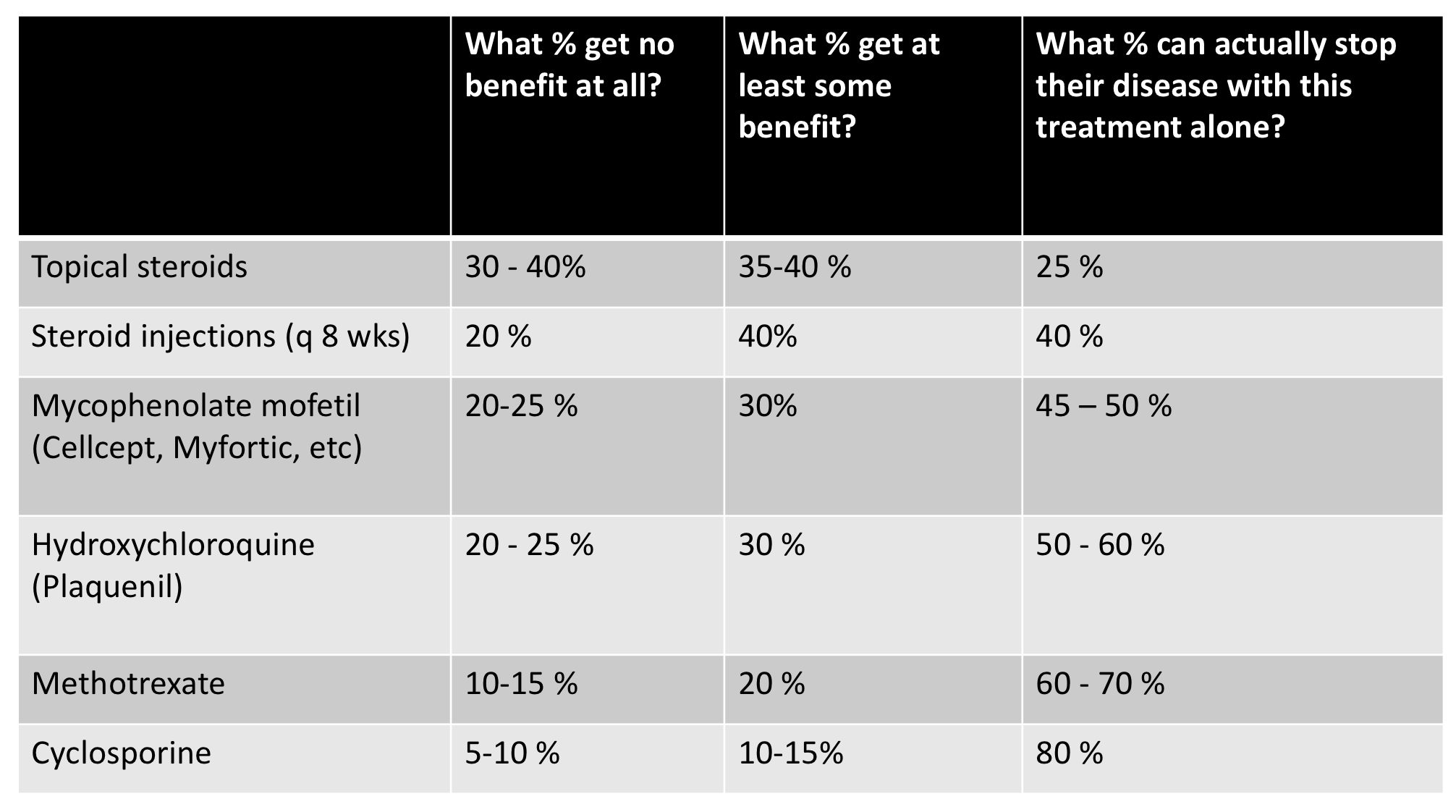
These treatment options do not help everyone. In discussing treatment options with one’s physician, side effects, ease of use, and cost must be taken into account. The proportion of patients who achieve partial of complete disease control with various agents is shown in the table below. Some treatments like topical steroids and steroid injections have a fairly good side effects profile if used correctly. However, they are unlikely to stop the disease completely if used alone. Nevertheless they may provide some degree of benefit. Other options such as the oral immunomodulating medications are superior to topical steroids and steroid injections but have greater potential side effects that must be weighed.
Treatment duration: How long do I need to be on these medications?
A common question from patients pertains to the length of treatment. Treatment duration ranges from 9 months to many decades or even forever. In other words, there is a great variation. Some patients require treatment for a short period of time and some patients require treatment for many years. There is no cure at present for LPP and treatment is geared towards stopping the inflammation which in term stops scarring. In cases of successfully treated LPP, the inflammation will be reduced from the scalp. However, the scarring remains.
Treatment takes many months to determine if it’s helping or not. The following table outlines how long it takes to first see benefits and how long it takes to know the full effects of the treatment. In general, some treatments like topical steroids may reduce inflammation and reduce itching within a very short time. However, it still takes another full 6-7 months to know how well this treatment will work. For example, if topical steroid are used as ‘monotherapy’ (the sole and only treatment), one can determine fairly quickly (1-2 months) if the treatment is having any impact. However, it would take 6-7 months to determine if the use of a topical steroid is sufficient to stop the disease.
Other treatments act much quicker. For example the oral medication cyclosporine acts quite quickly in LPP and one can generally ascertain benefits in a matter of months.
Disease Monitoring: How do we know if treatment is working?
The first signs that a treatment plan might be working is the reduction in redness, scale as well as general reduction in itching, burning or tenderness. However, the most important parameter to monitor is the clear and precise documentation that there is a halting of further hair loss. For this reason, scalp photographs are one of the most important requirements when monitoring scarring alopecia. If two photographs taken 6 months apart show that there has been more hair loss, the disease by definition is active (even if the patient feels better!). The importance of photographs can not be overstated.
Summary and Conclusion
Lichen planopilaris (LPP) is a scarring alopecia which requires immediate action to stop the disease and prevent further loss. Hair regrowth is not possible in most cases but some degree of regrowth may occur if the disease is caught in early stages. A carefully obtained history and examination but the physician are important to document the disease. A biopsy may or may not be necessary. A variety of treatment options are possible and taken several months to take effects. Some of the most effective treatment options are the oral medication and are associated with greater side effects than the topical medications. Nevertheless, many patients benefit from topical medications and these might be considered first or alongside the oral medications.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.