Exosome Therapy for Hair Loss
What are your thoughts on exosome therapy?
I’ve selected this question below for this week’s question of the week. It allows us to review some concepts in new therapies, including exosomes.
Question
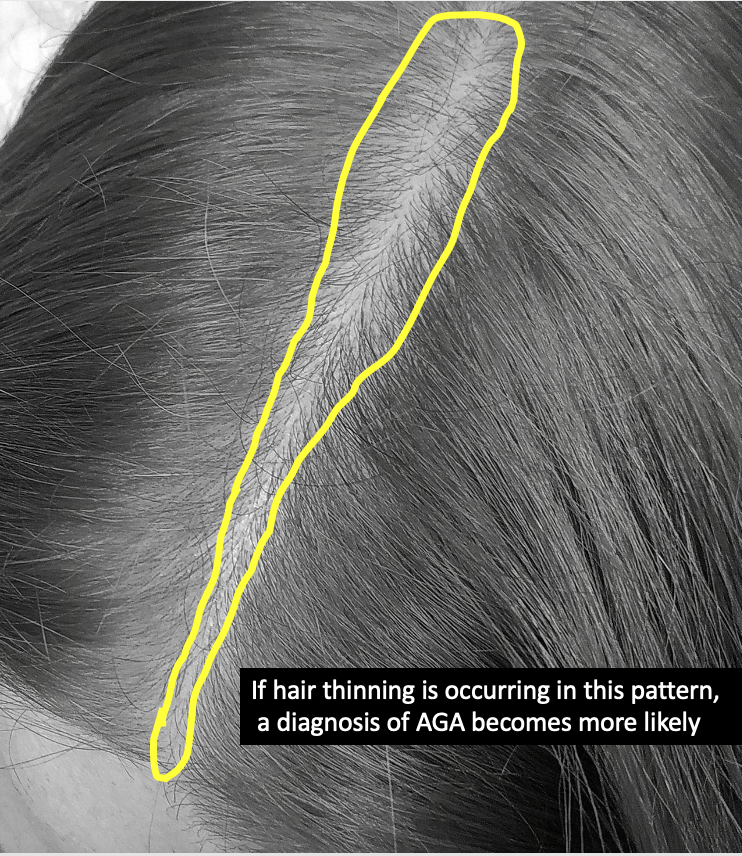
I have been suggested by my dermatologist exosome therapy, one injection per month for three months for MPB. I understand this is a novel therapy with limited studies.
I wanted to know your opinion, if you have had experience or know of results and/or side effects.
Thank you so much,
Answer
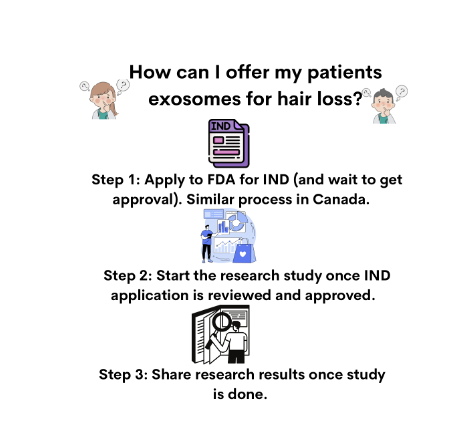
Thanks for the great question. I’m not sure what country you live in but here in North America (Canada and the United States), exosome therapy is not permitted - except under very special circumstances whereby a doctor has applied for and received a special IND application from the FDA (or equivalent in Canada).
I have yet to use it in my practice. In North America, if I wanted to use exosomes, I’d only be permitted to use it in the the context of a research study and I’d need to do all the paperwork to have my study approved. I’ll get back to that in a moment but you can already see how new and experimental exosome therapy truly is (as of the date of your question).
Exosome therapy is a potentially interesting therapy. To date, there have been very few published studies that actually show exosomes are all that helpful for treating hair loss. There was one study, however, by Chang-Hun et al back in 2019 in the Journal of the American Academy of Dermatology. That study had just 20 patients and followed the for just 12 weeks. However, the authors of that study found a 16 % increase in hair density and an 11% increase in thickness with use of exosome therapy. Not a lot - but some improvement. There were no serious side effects. That’s a nice change in hair density - but certainly not dramatic. With only 12 weeks of follow up, it’s unclear really what this means.
There have been a variety of in-vitro studies showing that exosomes can increase proliferation of dermal papillae (DP) cells, hair matrix cells, and outer root sheath cells as well as promote hair follicle stem cell proliferation and differentiation. I follow the world of exosomes closely!
Let’s dive deeper now.
What are exosomes?
Exosomes were only recently discovered - about 40 years ago. They are now being studied in various parts of medicine. Exosomes are extracellular vesicles that are produced by some type of cell. They are essentially tiny communication vesicles about 20-50 nm in size. It was first thought that exosomes were just cellular waste that got booted out of cells. Fortunately, it eventually came to be recognized that exosomes were important carriers of signaling molecules and were used for communication between cells. They contain many things including protein, nucleic acids, growth factors, lipids. It’s the growth factors in particular that are believed to be helpful in hair loss.
There are a wide range of cells that may be used to produce exosomes. However, donated human amniotic mesenchymal stem cells are one common source. Exosomes from adipose-derived stem cells are another source. There’s more yet - including exosomes from bone marrow derived mesenchymal stem cells.
Creation of exosomes. FROM: Graça Raposo and Willem Stoorvogel. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol . 2013 Feb 18;200(4):373-83. USED WITH CREATIVE COMMONS LICENSE. All credit to original source
The FDA Regulates Exosomes in the USA; Health Canada does the Same in Canada
The US Food and Drug Administration (FDA) has authority to regulate regenerative medicine products, including stem cell products and exosome products. The FDA has not given the green light to exosome therapy. It can only be used in a research setting by clinics that have a defined research study in place. The same is true in Canada. In Canada, exosomes fall under the jurisdiction of the Food and Drugs Act.
A US or Canadian physician who uses exosome therapy without having all the documents in place to show that they are conducting a research study could be subject to fines, and a variety of other penalties. It’s a serious issue and so exosome therapy is more common in other countries outside North America. In North America, a clinic needs to have applied for and received approval for an ‘investigational new drug” (IND) application before doing anything with exosomes.
I don’t do exosome therapy in my office. I’ve certainly had lots of conversations and phone calls with various regulatory bodies about these therapies. The message is always the same: A doctor can’t use these therapies unless they have been approved to do a clinical trial. Obviously in these kind of trials, the patient would sign a lot of forms indicating they know they are part of a clinical trial and the patient would be provided with proof that the clinic is part of such a trial. In other words, it would be pretty clear if a clinic in North America has an IND to study exosomes.
At the present time, there are no FDA or Health Canada approved exosome products for treating hair loss of any kind. Clinics can’t offer them (unless the patient receiving them is a research study patient).
The US FDA and Health Canada are very very worried about these types of therapies getting to the public without first doing the proper study. That’s why they want to study them ! In 2019, the FDA published a document for the public to warn of their concerns.
FDA’s Public Safety Message on Exosome Therapy
FDA’s Safety Alert for Exosome Therapy
Health Canada Warnings on Autologous Therapies
Investigational New Drug Applications (IND Applications)
An “IND” is a submission to the FDA to request permission to study a drug. The goal of the entire IND process to help collect information that a given drug is indeed safe to use in humans. An ‘investigator IND’ is a special type of IND submission whereby the IND is submitted by a doctor who then initiates and conducts the clinical study. In order for a doctor in North America to conduct any kind of study with exosomes, they need an investigator IND.
Exosomes are considered “drugs” by many regulatory organizations including the FDA and Health Canada because they are used to treat some sort of medical issue. Here, in our discussion today, that medical issue we are speaking about here is hair loss. That’s the first point that makes an IND needed for anyone wanting to use or study exosomes for hair loss. The second issue is that the drug is used in human beings. Studies on human beings using drugs that have not been approved in the past need an IND. There are no exceptions for exosomes: all users need an IND application. Exosomes are not an approved ‘drug’.
A clinic or researcher with an approved IND application has permission to ship across the country and then to use exosomes in a formal study. It does not give physicians permission to use exosomes in any way they wish - only in a pre-approved research study.
Summary
In summary, exosomes are a potential new therapy. The data to date on effectiveness is promising (although not super exciting). The concept sure is exciting. We don’t really know much about exosome therapy but more information is going to emerge in the next few years. Stay tuned. It seems safe in small studies but these studies are extremely small. We have no idea how often treatments will be needed and no idea if 5 treatments is safe but 55 treatments is unsafe. We have no idea if 1 year of treatment poses different risk than 10 years of continuous treatment. Exosomes are completely new.
Exosome therapy is not FDA approved and not Health Canada approved. Here in North America, clinics can’t offer them without first formally registering and being approved to conduct a clinical trial with the US of Canadian government. A patient in North America can’t receive these therapies yet without being part of a clinical trial. In other words, exosome therapy not just another therapy option like PRP. It’s completely different. It’s not possible to walk into a clinic and choose exosome therapy like one would choose PRP or a hair transplant. Exosomes can only be offered to North American patients in the context of a clinical trial. That’s important for North American readers of this article to be aware of.
Thanks again for the great question.
REFERENCE
Chang-Hun et al. Exosome for hair regeneration: From bench to bedside. J Am Acad Dermatol. VOLUME 81, ISSUE 4, SUPPLEMENT 1, OCTOBER 01, 2019
Graça Raposo and Willem Stoorvogel. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol . 2013 Feb 18;200(4):373-83.