Treatment of LPP
I’ve selected this question below for this week’s question of the week. It allows us to the review some key concepts in the treatment of lichen planopilaris and the importance of photos in the long term evaluation of LPP disease activity.
Question
I have been diagnosed by biopsy 18 months ago with lichen planopilaris. I am a 74 year old woman and I noticed about three years before that I was thinning at the front of my head. My dermatologist has tried to help me with an antibiotic which I took for 6 months, to help the inflammation, or lower it. It wasn't effective and I don't think one should remain on this antibiotic for a longer time. The hair loss is also behind my ears and a little on my crown.
Since the beginning of April, I have been taking Hydroxychloroquine 200 mg every day in an attempt to stem the hair loss. I have not had any of the possible side effects thankfully. In fact, in the two months since I started this medication, I notice that I really don't have an itchy scalp any longer and much less frequently, an itchy back, My scalp isn't tender and not red close to the hairline as it was before this medication. Thankfully, I do not have any health problems and the only medication I take is for an under active thyroid.
Can you please advise if this would be a plan of action that you would advise?
Answer
Thanks for the great question. I’m so glad things seem moving in the right direction for you.
I can’t tell you if you are using the perfect plan because not enough time has elapsed. What I can say is there are good things in your story above that indicate you are indeed on track.
However, if you take a photo of your scalp in 2 years from now and it looks 100 % the same (or better) than the that photo that I’m going to enoucrage you to please take tonight ….. I can tell you that you are indeed on the right track!
Let’s look at some important points.
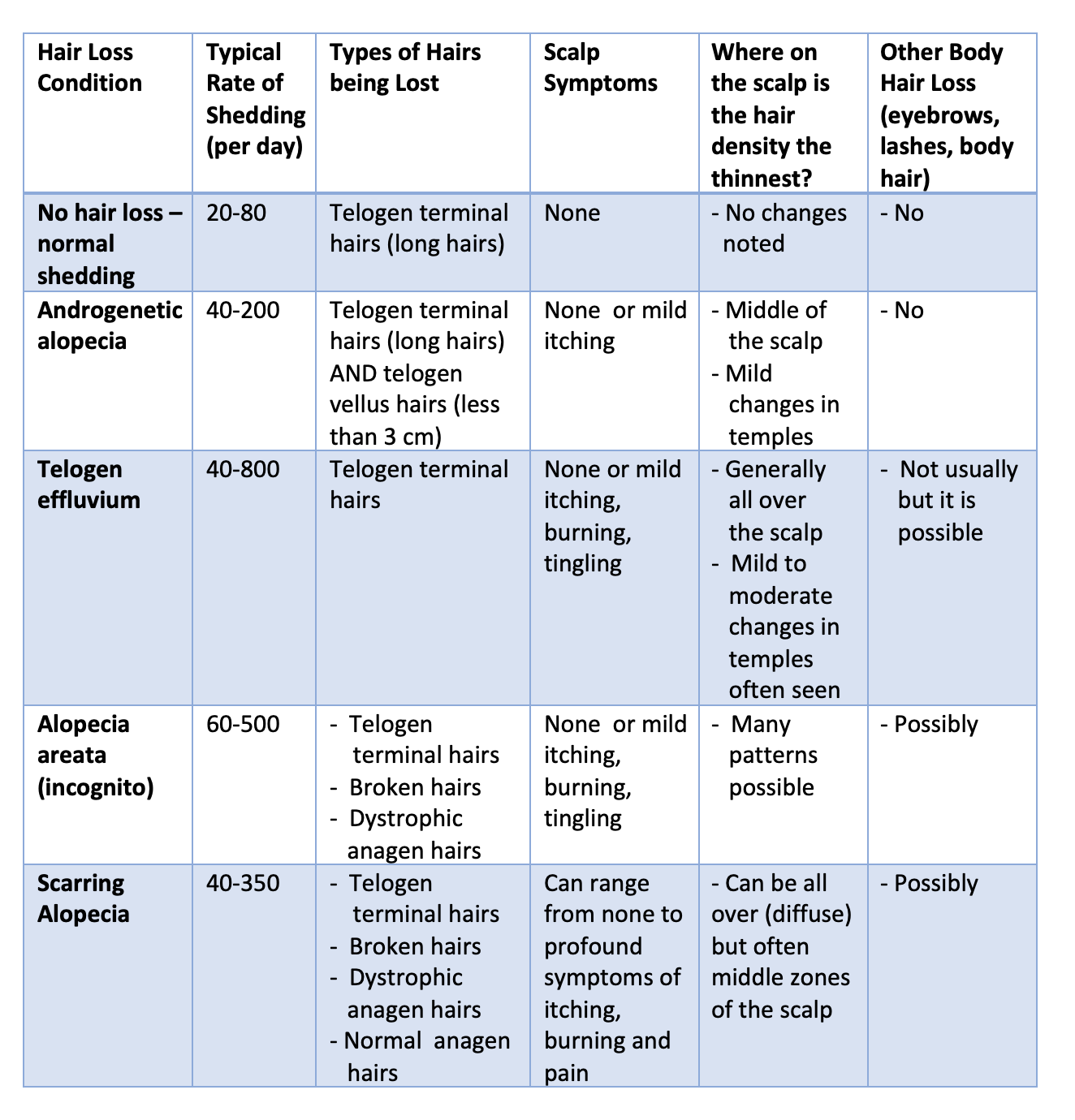
When we successfully treat scarring alopecia, we want several things to happen:
a) We want the rate of hair shedding to return back to ”normal”
b) We want scalp symptoms to disappear such that there is no itching, burning or tenderness
c) We want any scalp redness to disappear
d) We want hair loss to stop such that it’s not getting worse and worse over time.
e) Finally, if we catch LPP “early enough” in its disease evolution, we even want a bit of improvement in hair density to occur.
So are you successfully treating your scarring alopecia ?
It certainly sounds like you are treating your LPP quite well so far in your treatment journey. However, I can’t know for sure if the disease activity has “stopped”. Sometimes there will be clues when your dermatologist examines your scalp up close with trichoscopy that the disease activity has been reduced. For example, if you once had perifollicular scale (scale around the hairs) or had perifolliicular redness (redness around the hairs) when the scalp was examined by trichsocpy and now you do not have these findings, it means that your LPP disease activity has been reduced. If it was once possible to easy pull a great number of hairs from the scalp (i.e. a positive pull test) and now it is not so easy to extract hairs, then it may mean your disease activity has reduced.
The mistake that many patients and physicians make is assuming that zero redness, zero shedding and zero scaling means zero scarring alopecia disease activity. That’s not quite accurate. However, it sure sounds good. But it’s certainly a really important “first step.”
You see, it could be that for some patients that the redness goes away, and shedding reduces and flaking goes away and still the hair loss continues a little bit. That’s why photos are so important! I would encourage everyone with scarring alopecia to take photos or have someone take them for you.
I often get referrals from doctors who ask me to help the figure out if their patient’s disease activity is zero or not. If I don’t see much activity on the scalp when I perform a scalp examination, I reply to the patient and referring doctor by saying “things seem quiet today but I’ll give you my final answer in two years.”
I’ll take a photo now and then again 6 months, 12 months, 18 monks and 2 years. Sometimes we will take even more photos. If the photos look the same over a 2 year period of careful observation and there has been no further loss at all … then the scarring alopecia disease is deemed inactive.
I will point out at this juncture that the word inactive is not the same as burnt out. Inactive means the disease is quiet but it could be that the use of medications brought it to that state. Burnt out means the disease is completely over. One can take away all medications from true burnt out scarring alopecia and the disease still stays quiet.
Is your disease active?
You are only a few months into hydroxychloroquine treatment. It could be that the medication has slowed your LPP disease activity down or it could be that the medication has completely stopped the disease. We won’t know for sure a while. For some patients, it takes just a matter of months to see that the hair loss has in fact still continued. For others, it will take a full 1 or even 2 years to really get an appreciate that the hair loss is still continuing. It just depends one the speed of the hair loss.
If one’s LPP is progressing along fast, I can tell in 1- 2 months if the disease is still active
If one’s LPP is progressing along moderately fast, I can tell in 4-6 months if the disease is still active
If one’s LPP is progressing along moderately slowly, I can tell in 9-15 months if the disease is still active
If one’s LPP is progressing along really slowly, I may need 18-24 months to tell if the disease is still active
So I would encourage you to take lots and lots of photos every 3-6 months. When it comes to treating scarring alopecia, photos are so so important.
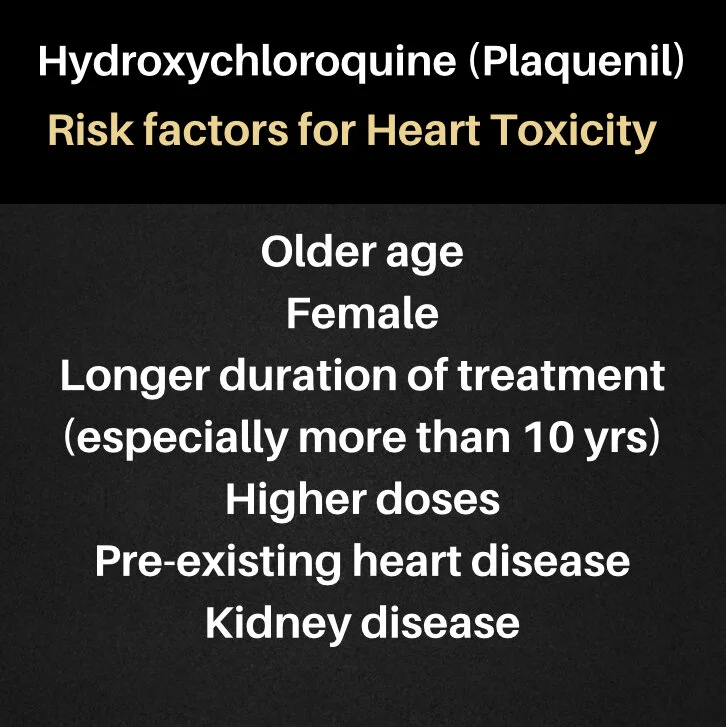
Of course, you’ll want to check in sooner with your doctors than 2 years in order to figure out how well you are doing on your treatment. In fact, you’ll probably want to be checking in with your doctors every 4-6 months. I’m glad you have no side effects with hydroxychloroquine but do keep in mind that some side effects with hydroxychloroquine happen after 1-2 months (ie changes in blood counts or liver enzymes) and some side effects don’t really become all that common until 5-10 years have gone by (ie retinopathy) So, if you do stay on this medication, be sure to have periodic follow up to monitor side effects.
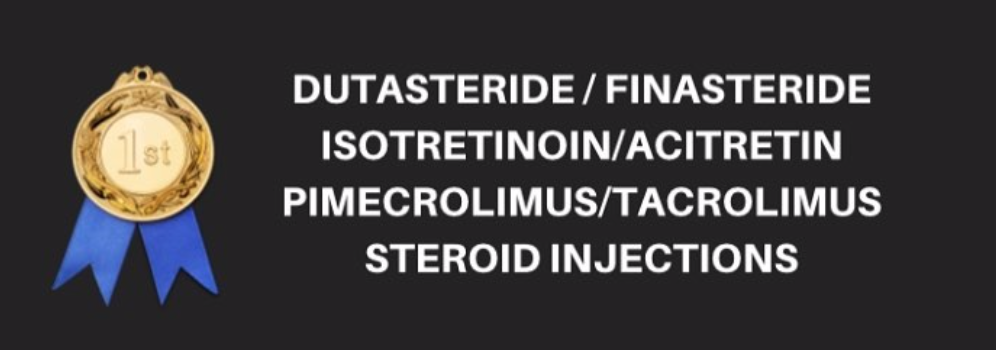
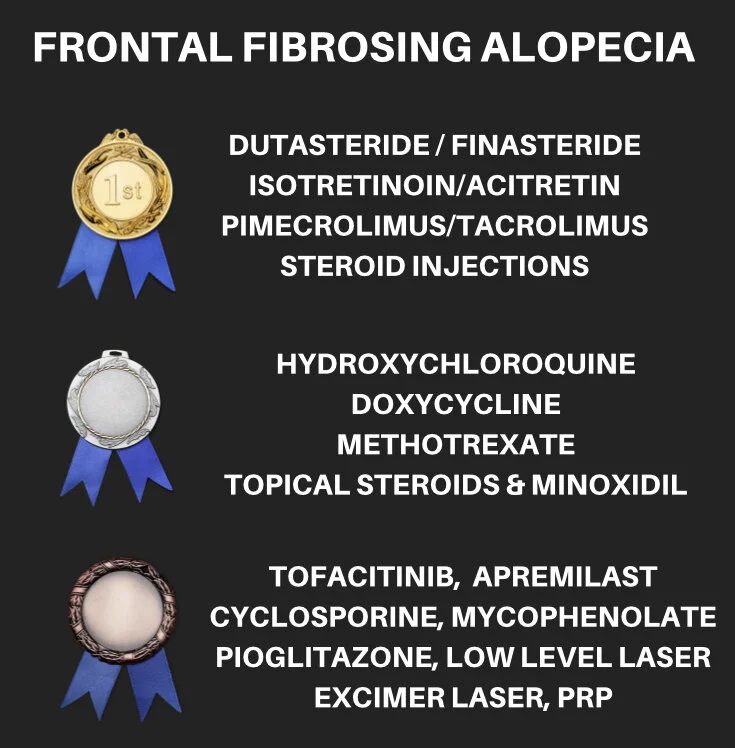
If you find that hair loss seems to be continuing when when see your doctors at the 4-6 months follow up or the 1 year follow up, then that means you may want to bring on board other treatments to help the hydroxychloroquine. There are many treatments for LPP.
Sometimes, a patient keeps losing hair despite the fact that the every doctor thinks the scarring alopecia is quiet. In some cases, the scarring alopecia is not quiet and the impression of the doctors is wrong. In other cases, the scarring alopecia is, in fact, really quiet but other types of hair loss are present in the patient too that nobody has picked up on.
For example, if a patient’s scarring alopecia has been brought under good control but they have a telogen effluvium present from some other medication they recently started then guess what? Hair shedding is going to continue and hair density is not going to get better. Every hair loss condition needs to be addressed!
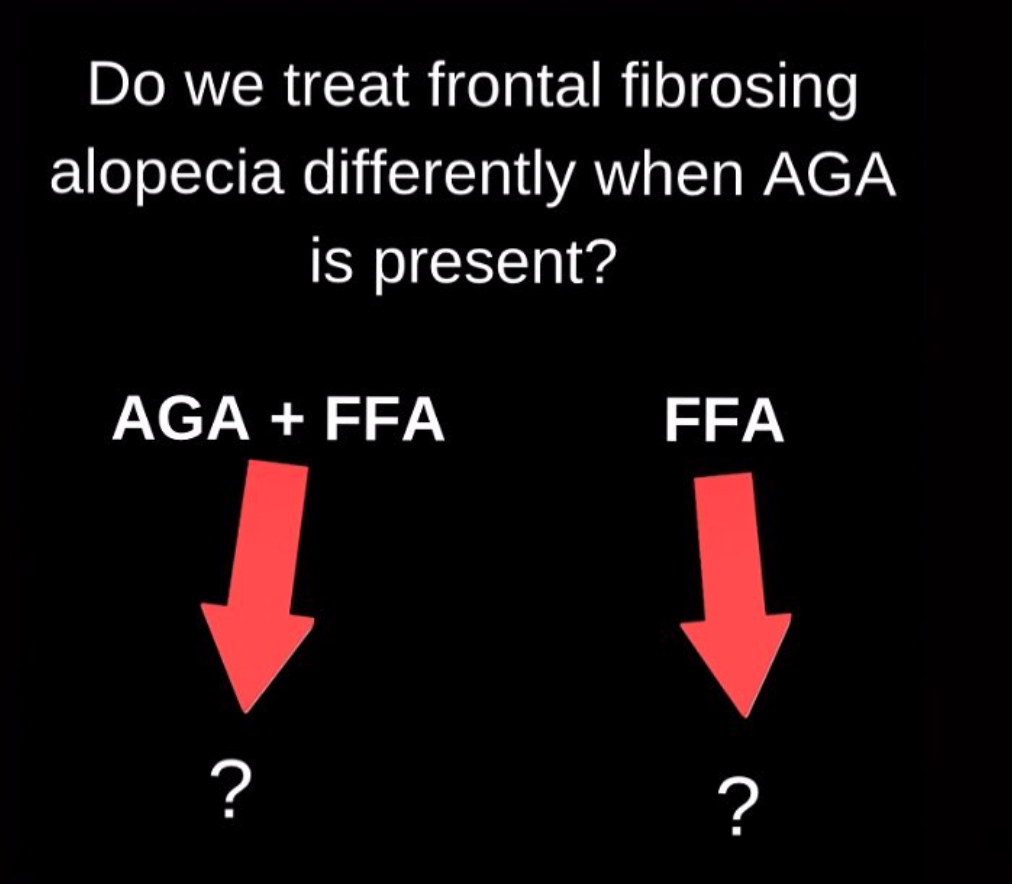
If a patient has both a scarring alopecia and a telogen effluvium, then both the scarring alopecia and the telogen effluvium need to be properly treated. If a patient has scarring alopecia and androgenetic alopecia, then both the scarring alopecia and the androgenetic alopecia need to be properly treated in order to maximize regrowth. If a patient has scarring alopecia and a telogen effluvium and androgenetic alopecia (all three), then a treatment plan needs to be created that addresses all three of these conditions.
Conclusion
Thanks again for the great question. I am glad things have improved. I would encourage you to take photos as this issue going to be the best way to get a really good sense of how well you are doing in the long run. I am always encouraged when patients report they are improving but what matters most to me is really how well a person is doing over a very extended period of time.
Doctors and patients can sometimes debate about whether they are better or not after a few months. However, there is absolutely no debate after 1 or 2 years. A photo captures the essence of the disease activity completely.