When Latisse Won't Work
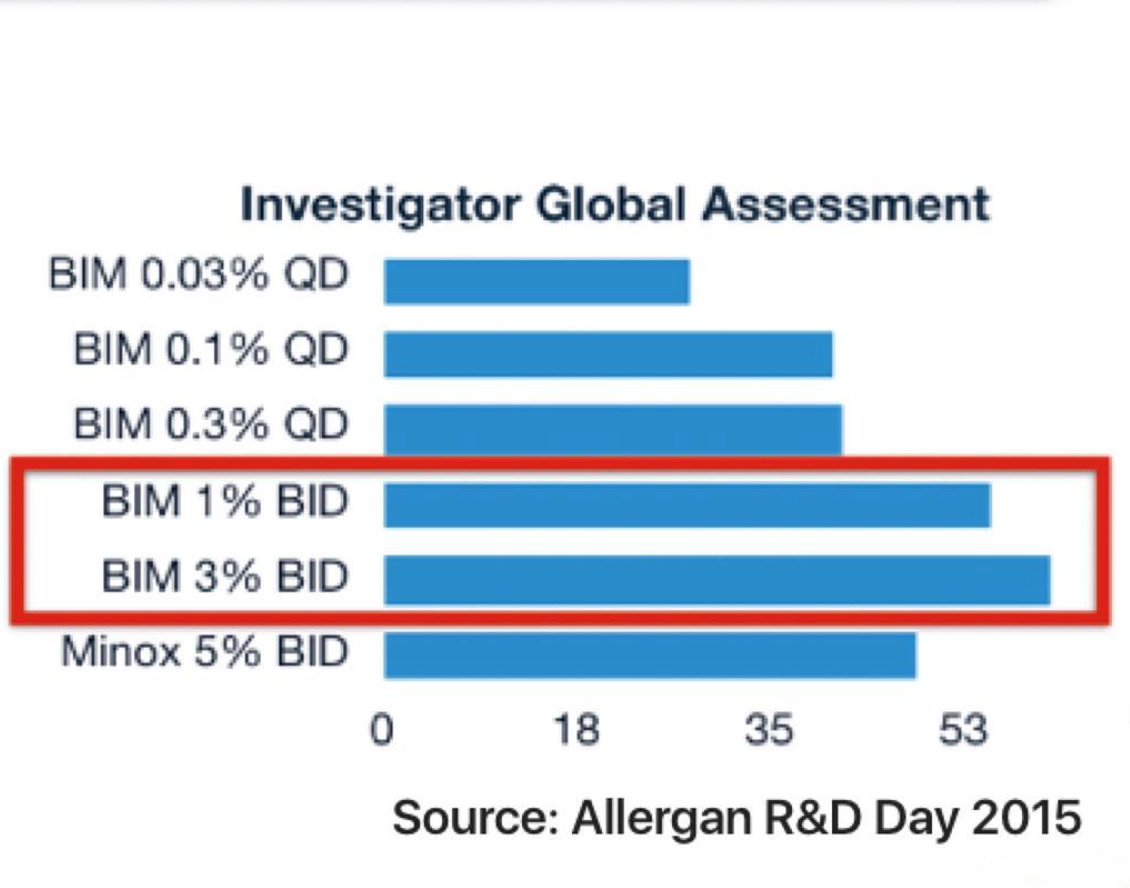
Latisse is an FDA approved and Health Canada approved treatment for improving eyelash length, thickness and darkness in patients with eyelash hypotrichosis (not enough eyelashes). Latisse contains the ingredient bimatoprost.
Clinical studies have shown that Latisse is very effective for many user. Many notice changes as early as 4 weeks and 50 % have changes by the second month. By 16 weeks, 80 % will have an improvement.
Latisse Non-Responders: When Latisse just doesn't work
Latisse is effective for many individuals. However, about 1 out of every 5 users is not going to find that the medication worked all that well for them. A large proportion of the patients I see in my office come to see me wanting to know why Latisse did not work as good as the advertising stated it should. Let's review some of the reasons for poor results.
1. The patient is simply in the "20 % group."
Latisse does not help everyone. By 16 weeks, 80 % will be pleased with the money they spent. 20 % won't. I tell my patients that someone has to be in the "80 % group" and someone has to be in the "20 % group." Not everyone responds to Latisse.
2. The bottle does not contain bimatoprost and so it is not Latisse.
Latisse is available through physician's offices (and some drug stores), but there are many other ways of obtaining Latisse and products that claim to be Latisse. I encourage readers to simply enter phrases such as "buy Latisse online" in their Google search engine to see the array of possibilities. Most of these sites will ultimately lead to a box of Latisse (containing the true ingredient bimatoprost) showing up at the door. But not all. Patients need to keep in mind the possibility of counterfeit products. It's rare but most certainly does happen.
3. The method of application is wrong.
One needs to apply Latisse nightly to the lower eyelid margin of the upper eyelid with the brushes provided. I can't tell you how many variations of this simple sentence there actually are. Like any drug, it needs to be used according to instructions.
4. The individual has a medical condition of the hair follicle.
It comes as a surprise to many individuals that there are well over 100 reasons for eyelash loss. Not all lash loss is simply due to "aging" or a "tainted bottle of mascara" that was used in the past or improper use of a heated eyelash curler. These certainly can cause temporary or even permanent lash loss. Rather a variety of inflammatory and autoimmune conditions are associated with eyelash loss.
Eyelash Loss: What else?
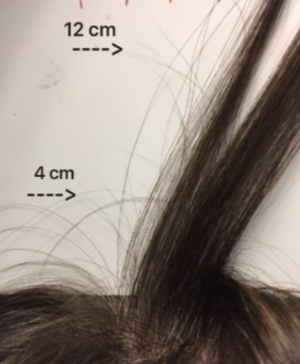
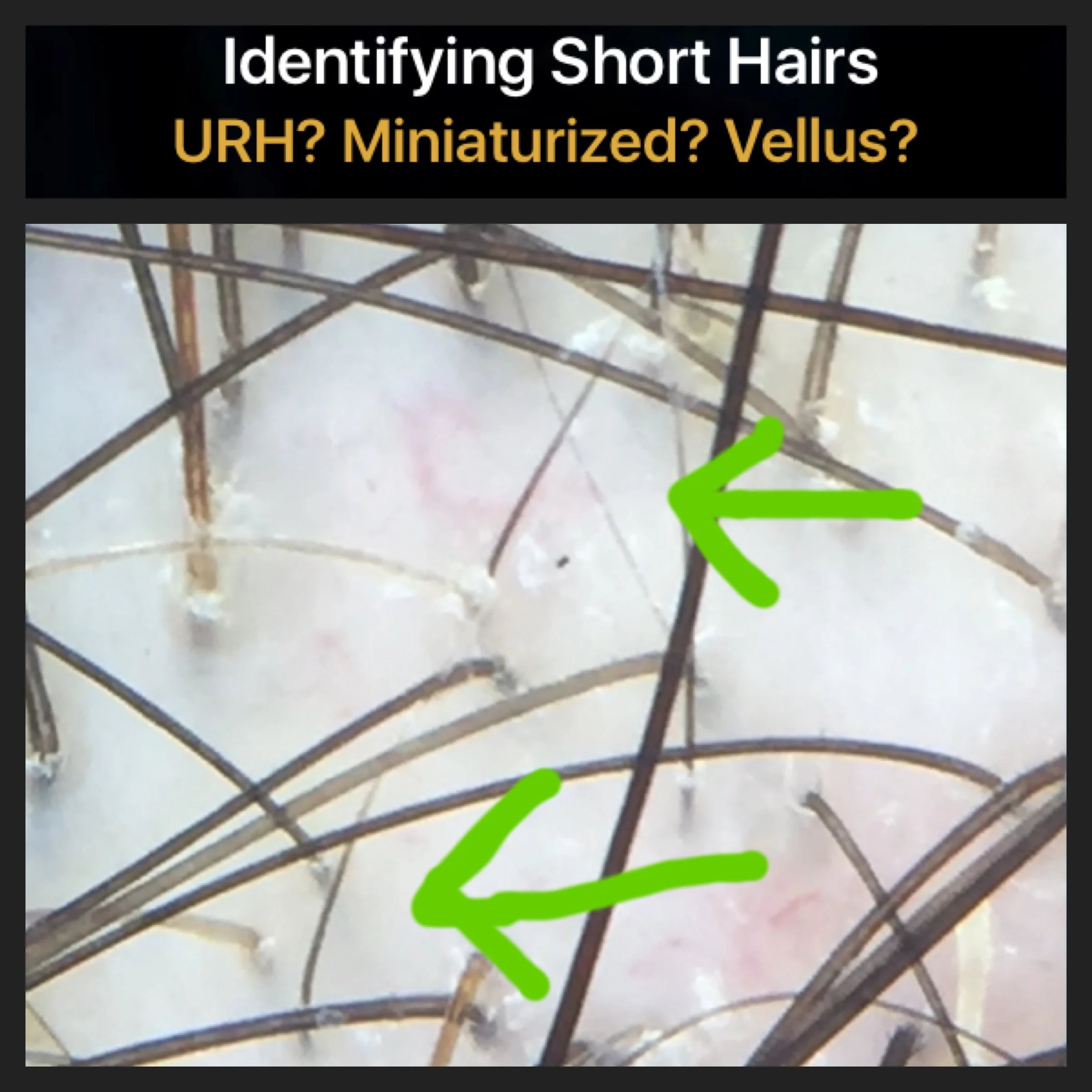
A careful review of one's story (called the medical history) and up close examination of the eyelashes is needed to determine the cause. One must also examine the eyebrow and scalp hair at the same time as there is no other way to confidently come to the diagnosis.
Causes of eyelash loss include
1. Inflammatory and Autoimmune Conditions. Inflammation of the hair follicle can cause it to fall out. Alopecia areata, frontal fibrosing alopecia, Scleroderma/ en coupe de sabre and lupus are all potential causes. A variety of true dermatological conditions can also cause lash loss including various eczemas, seborrheic dermatitis and psoriasis. In such cases it is scratching and rubbing that often leads to lash loss.
2. Trichotillomania. 3-5 % of the world will purposefully pull out one or more of their hair follicles somewhere on the body during their lifetime. When repeated, the diagnosis of trichotillomania needs to be considered. Plucking of the lashes is quite common and may even be one sided.
3. Endocrine disorders. Isolated eyelash loss is uncommon in patients presenting with endocrine disorders. However, one needs to consider thyroid, parathyroid and pituitary disorders.
4. Infections. Infections with fungus, bacteria, viruses all have the potential to cause lash loss. Isolated lash loss is uncommon but can be seen with conditions such as leprosy and syphilis.
5. Drugs. There are many drugs now implicated in lash loss ranging from cancer drugs to antidepressants (escitalopram) to diabetes medications (sitagliptin and metformin) to methylphenidate. Other drugs include blood thinners, cholesterol meds, propranolol, valproic acid. Even cocaine vapour can cause lash loss.
6. Infiltrative Conditions. Eyelashes can fall out when cells enter the hair loss that normally don't reside there. Lymphomas are a good example. Eyelash loss can also occur with a variety of local tumors including basal cell carcinoma, squamous cell carcinomas, sebaceous carcinomas and many others.
7. Nutritional Issues. Poor diets and specific deficiencies can all cause lash loss. This ranges from severe illness with marasmus, to deficiencies of protein, zinc and iron.
8. Congenital and genetic conditions. Many many genetic syndromes are associated with less than normal eyelash density. Well over 50 conditions fall in this category from KID syndrome, Rothmund Thompson syndrome, Incontinentia Pigmenti, Keratosis follicularis spinulosa decalvans, Progeria, Bloom syndrome, Menke's syndrome, Monilethrix to Trichothiodystrophy. Many many others are on this list as well.
Conclusion
There are many causes of eyelash loss. Not every cause of eyelash loss responds to Latisse.