Can I just buy a USB trichoscope and figure out my own diagnosis ?
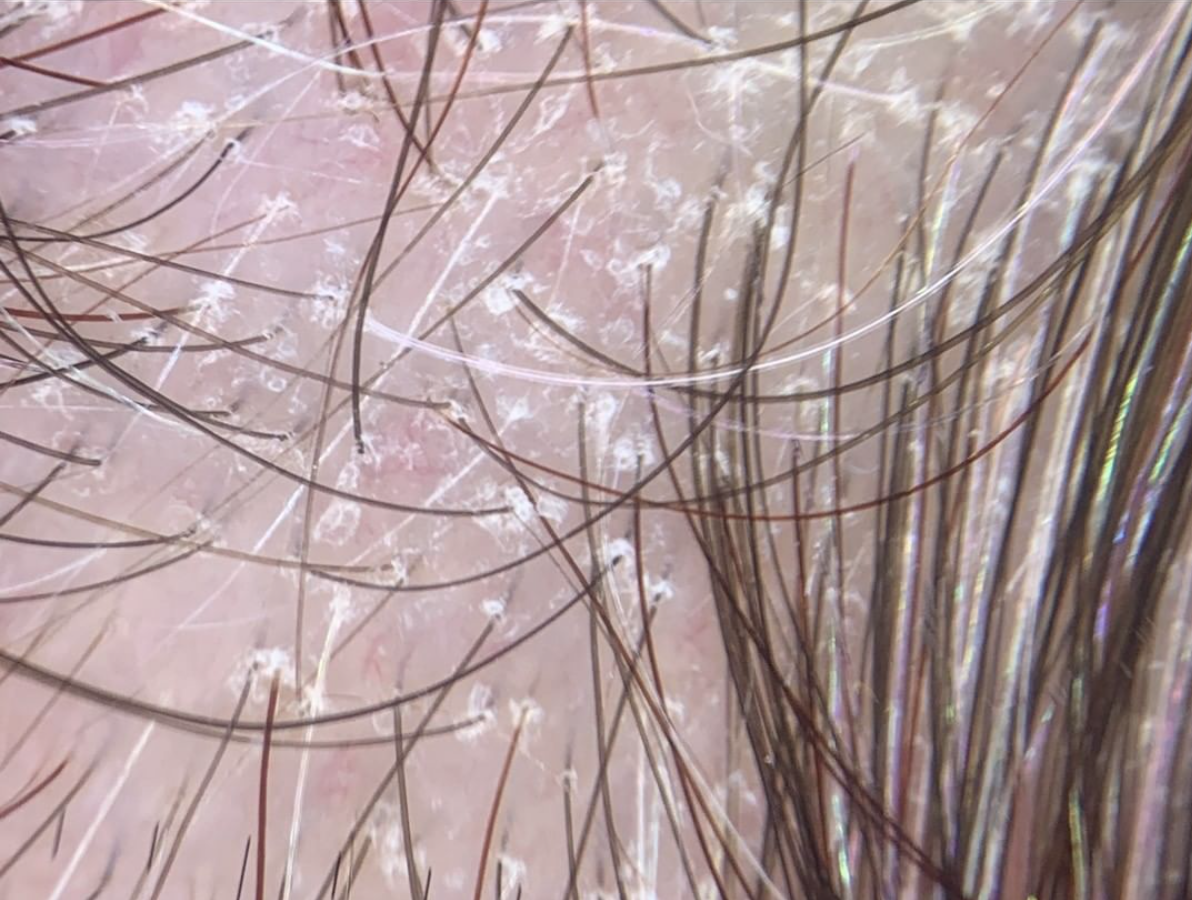
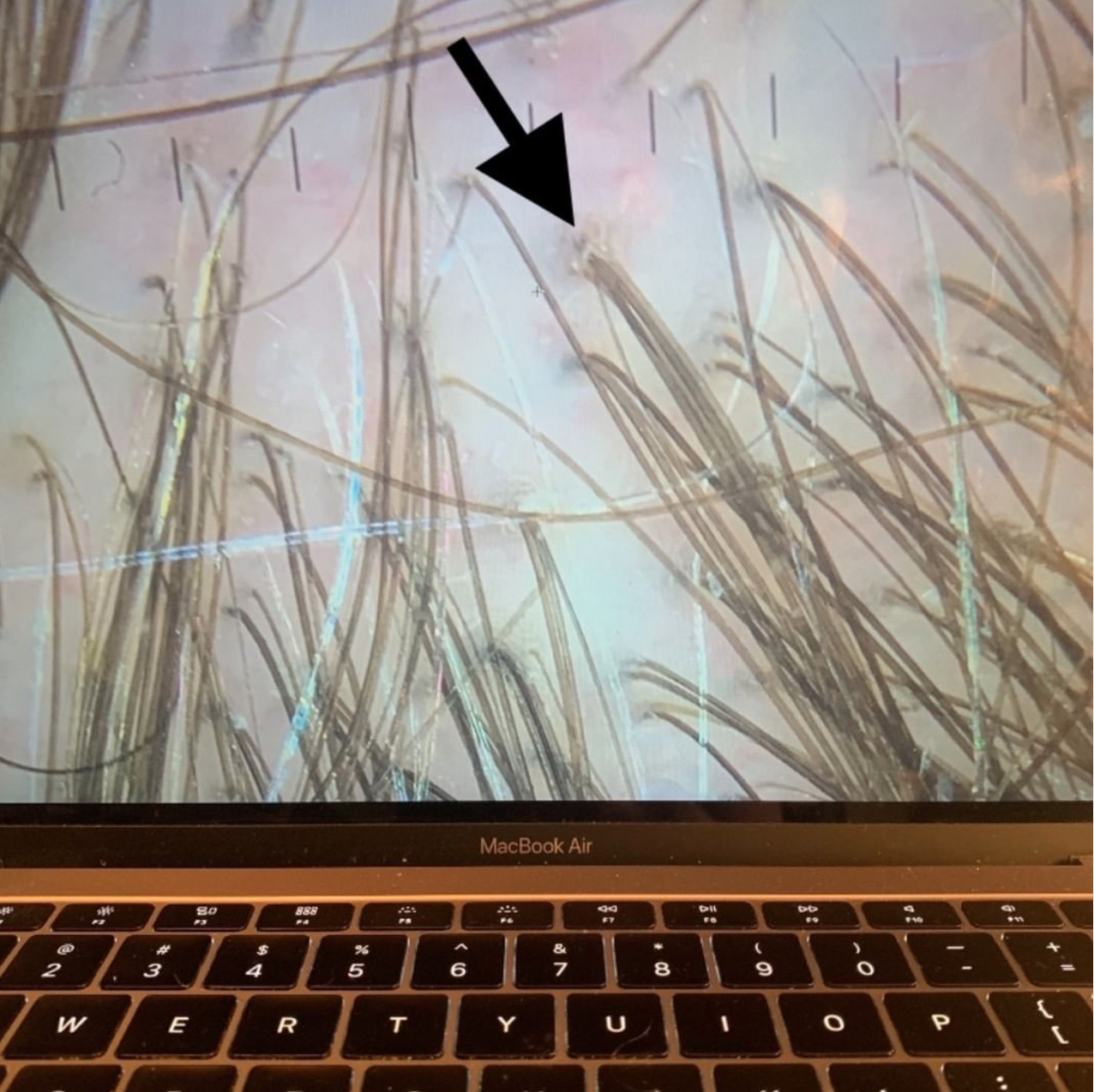
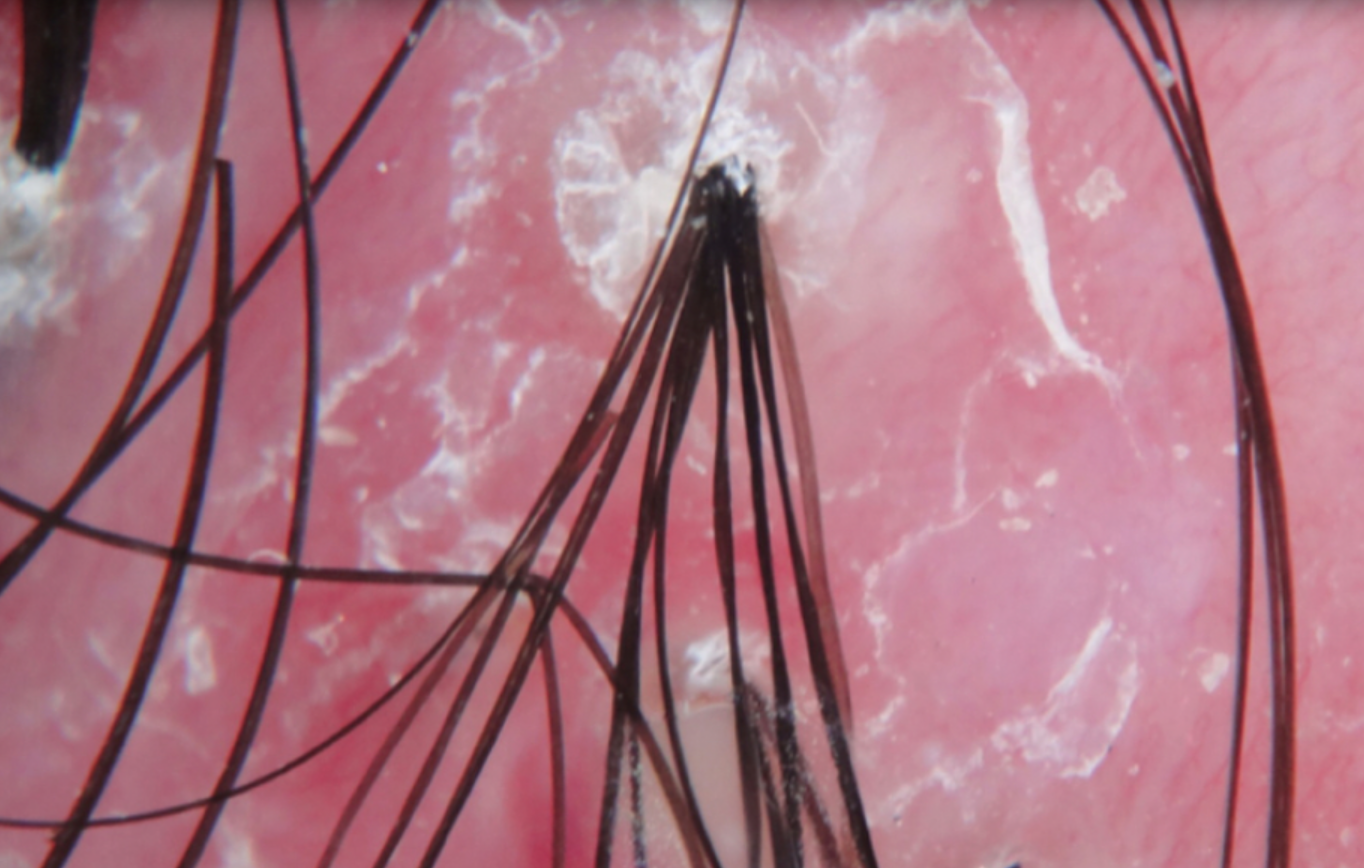
Trichoscopy is a wonderful diagnostic tool. Trichoscopy refers to the use of some sort of handheld device for viewing the scalp with higher magnification. These devices are widespread - they range in price from $ 35 for a pretty reasonable USB microscopy to $ 1,500 for a hand held device to $ 15, 000 for a video dermatoscope.
There are quite a few misconceptions that the pubic has about these devices.
1. Will trichoscopy tell me the diagnosis?
That answer is no. One can buy a USB device, plug it in and see beautiful pictures on the screen. But what does it mean? That requires an expert! It takes a few weeks to become reasonably good at trichoscopy and then a few years to become an expert. The USB trichoscope device does not give a print out that reads “you have androgenetic alopecia” or “you have telogen effluvium.”
Consider a useful analogy. If my air conditioner breaks down, I can certainly get out my tool box and open up the back of the air conditioner and see inside. But unless I known what I’m looking for, the process is not that useful and I will not know what’s wrong with the air conditioner (I can assure you based on my experience with doing this exact task).
2. If the trichoscope won't tell me the diagnosis, can’t I just email the doctor the pictures and he can tell me the diagnosis ?
I don’t like really ever answering two “no” answers in a row , but this answer is also no. We’re commonly asked this question. We have many people who ask us if they can just send in photos they have obtained with their own trichscope. These photos are not helpful UNLESS I have the entire story of the patient’s hair loss and have reviewed their blood tests and know absolutely everything about them. Then these trichoscopic images are a major bonus! It’s true that I can be pretty sure what’s going on by their photos - but not 100 % sure. Doesn't one want to be 100- % sure or at least as close to 100 % sure as possible?
The mistake people make is thinking trichoscopy is “everything.” They think to themselves that all I need to do is take pictures of my scalp of find some clinic to take trichoscopy pictures of my scalp and I’ll know what’s going on! That’s wrong, wrong wrong ….and that’s where I see people run into problems time and time again. Trichsocopy is wonderful but it’s only part of the puzzle. As an aside, some people also make the similar mistake of thinking that their blood test results are “everything.” They think to themselves that all I need to do is get to my doctor and get some blood tests and I’ll know what’s going on! That’s also not a correct approach. One needs the entire story and the chance to see the scalp in it’s entirely.
Although I’m sure I sound like a broken record, I’d like to remind the reader that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s story
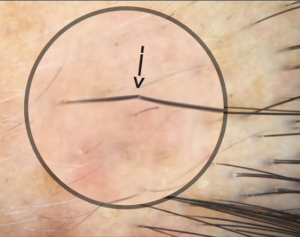
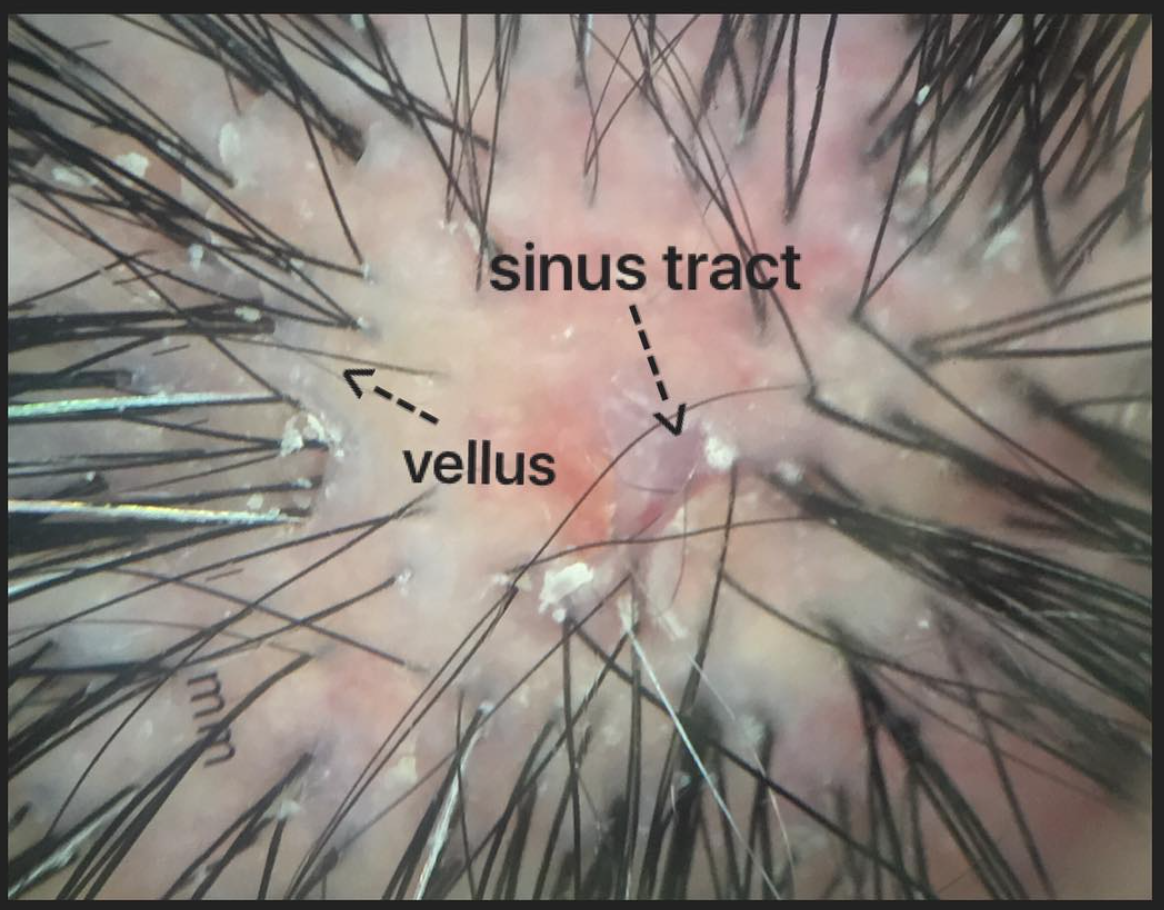
2) the findings uncovered during the process of the scalp examination (sometimes including trichoscopy, pull test, clinical exam, card test, etc)
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
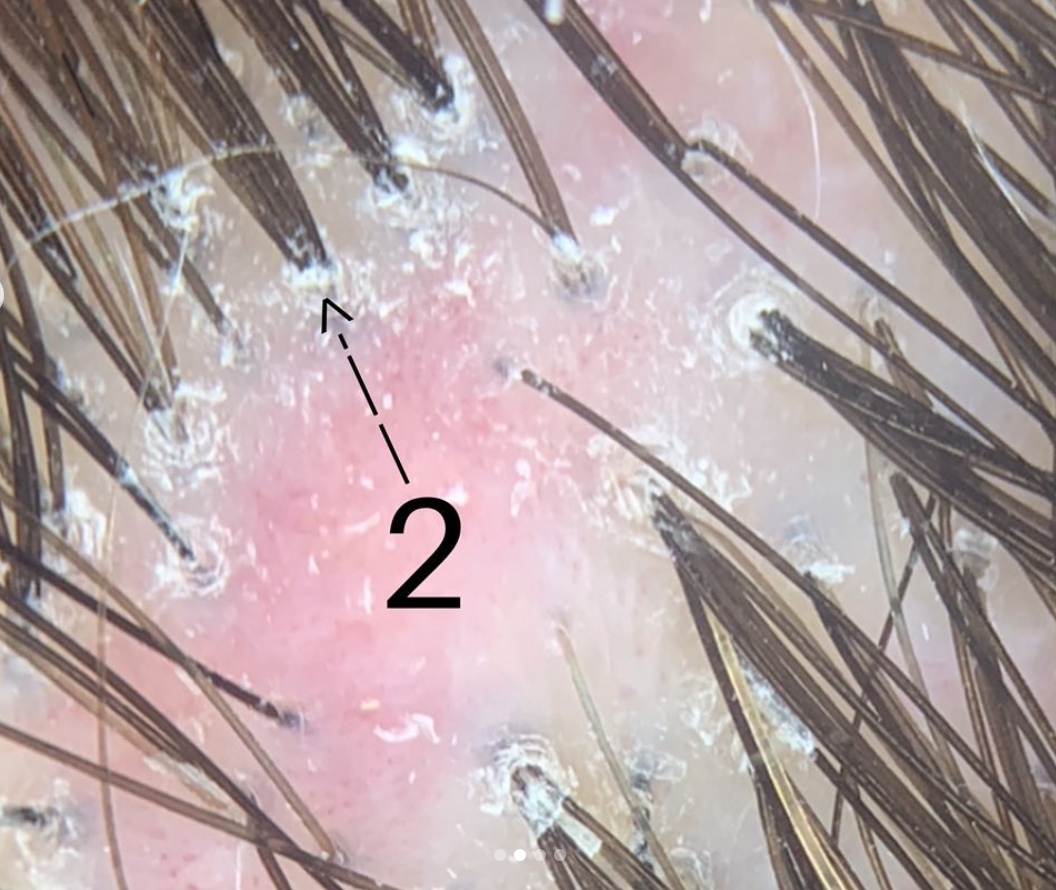
In summary, I can diagnose so many conditions with trichoscopy - but there are so many situations that I can not.
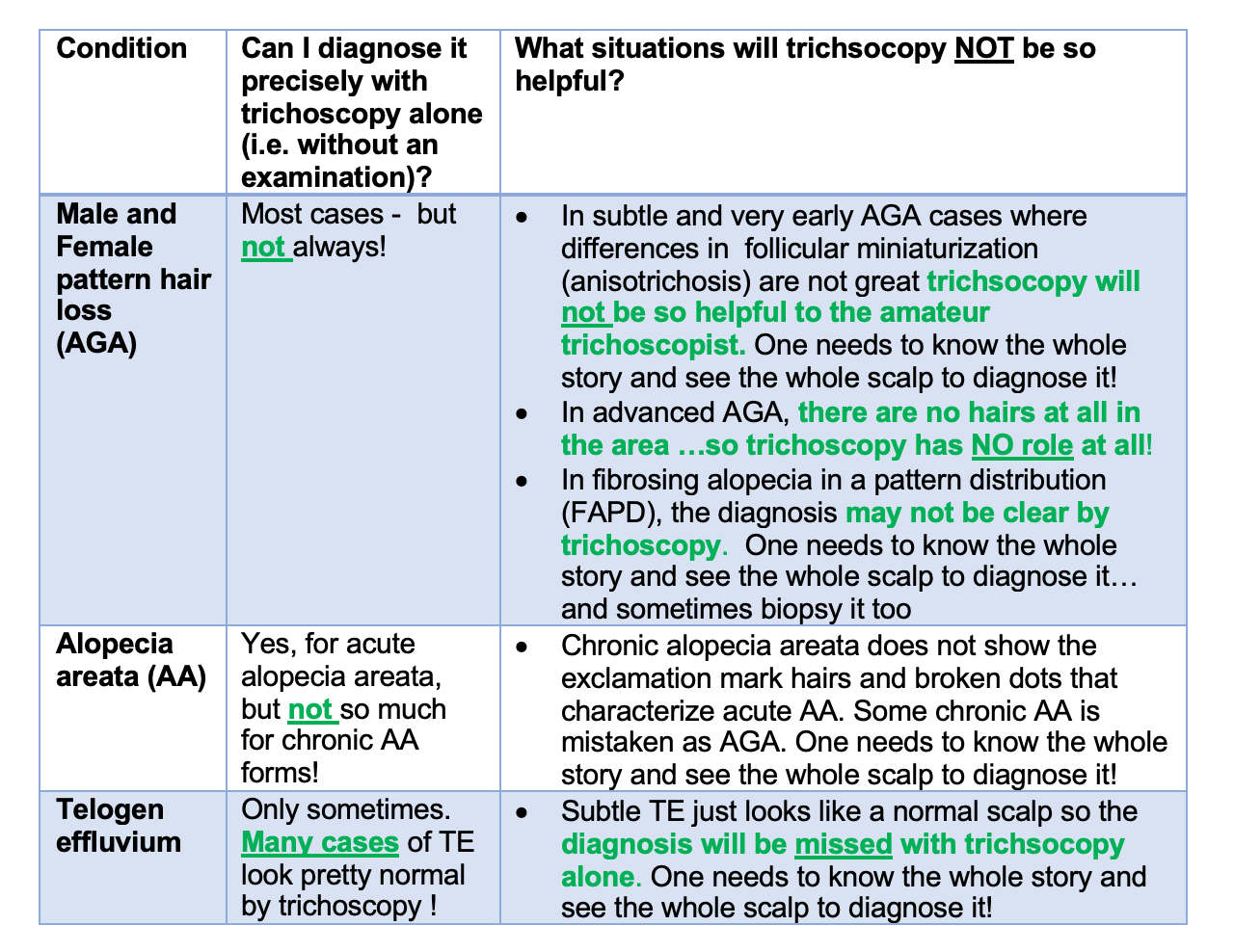
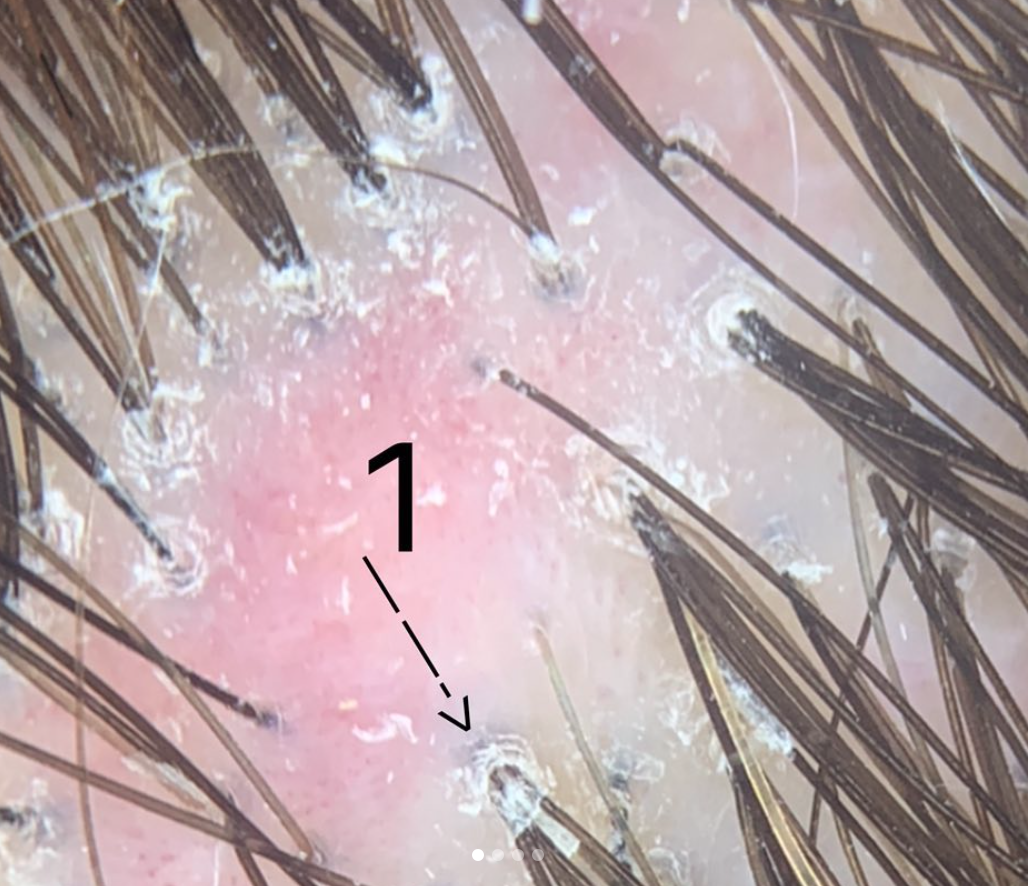
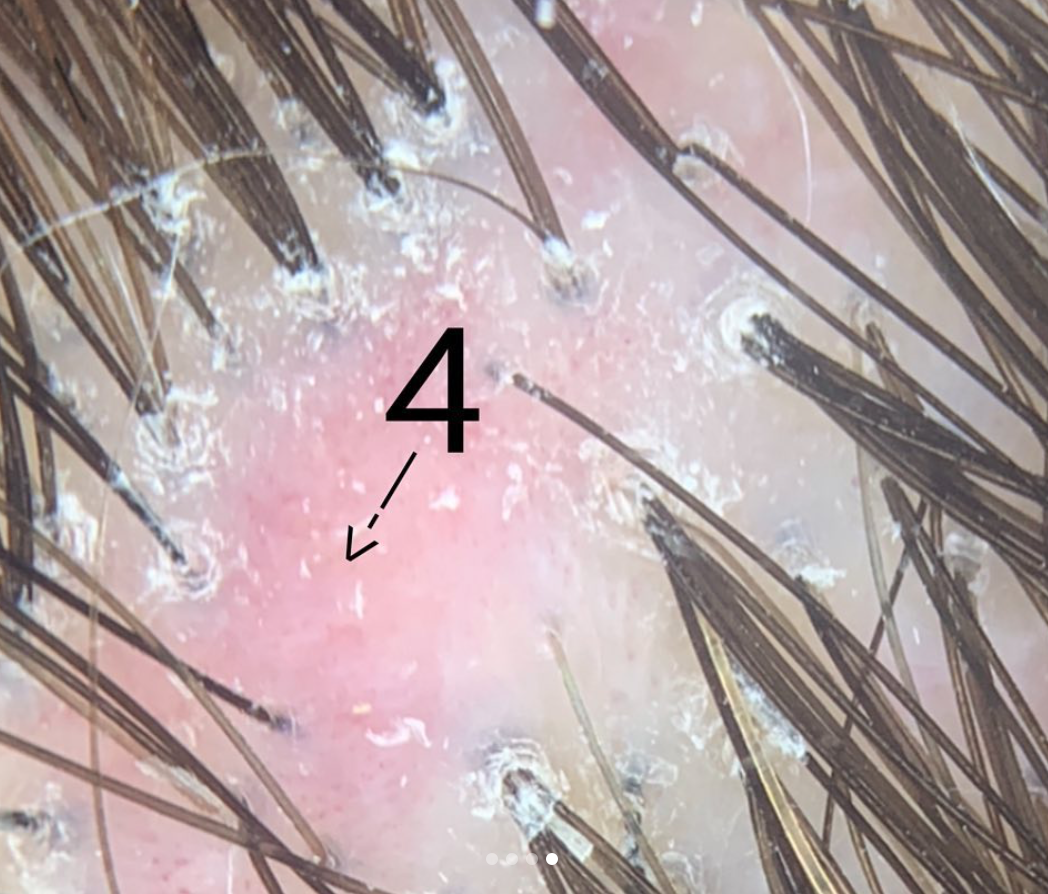
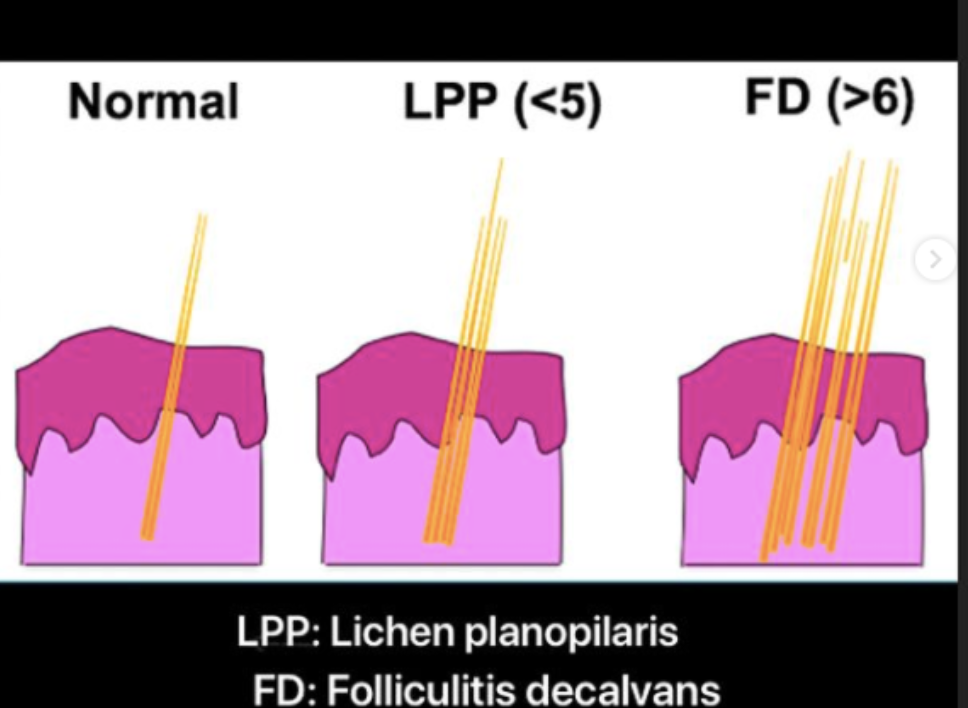
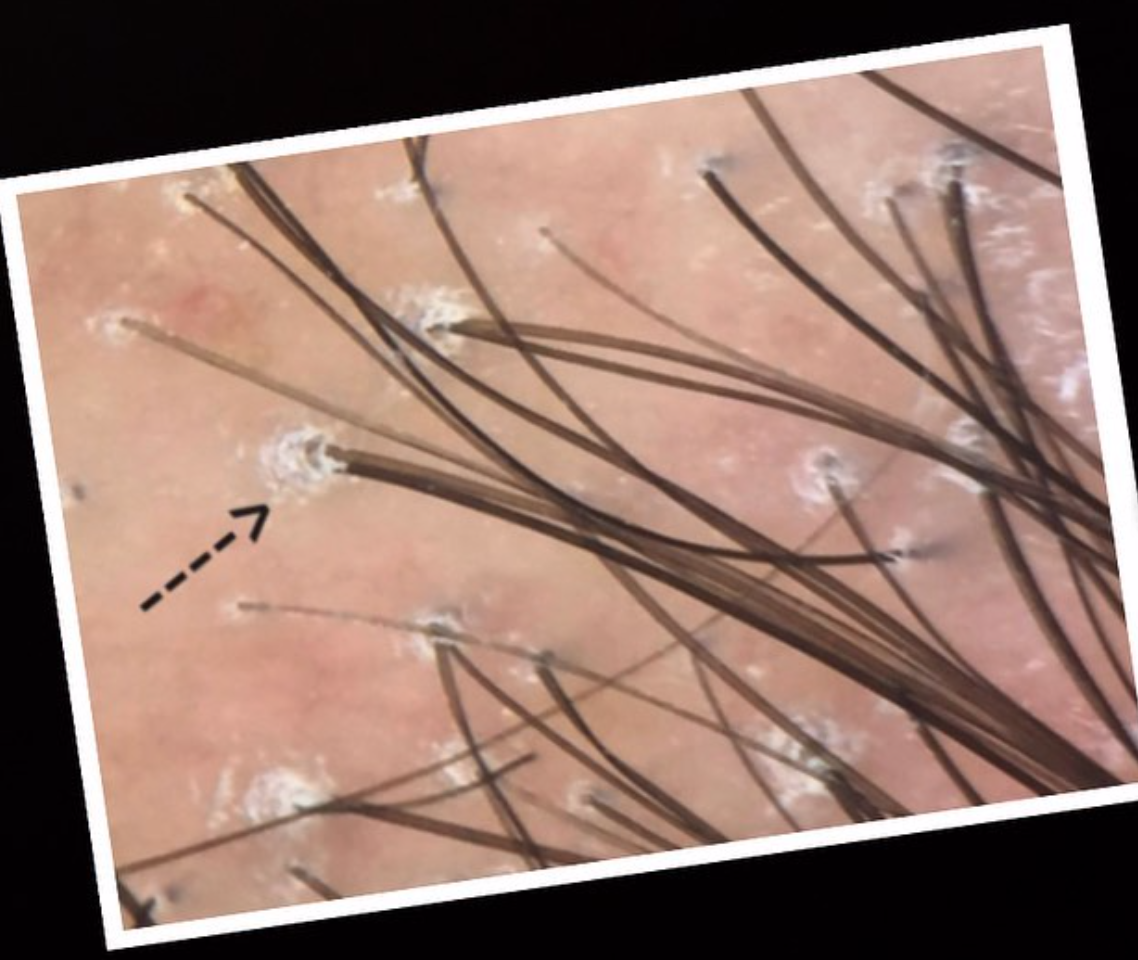
Let’s take a look at some situations where trichsocopy has it’s limitations.
EXAMPLE 1: TRICHOSCOPY IN THE NON SCARRING ALOPECIAS
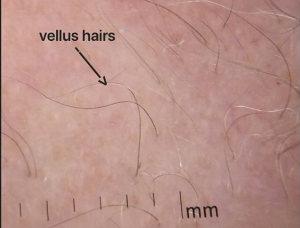
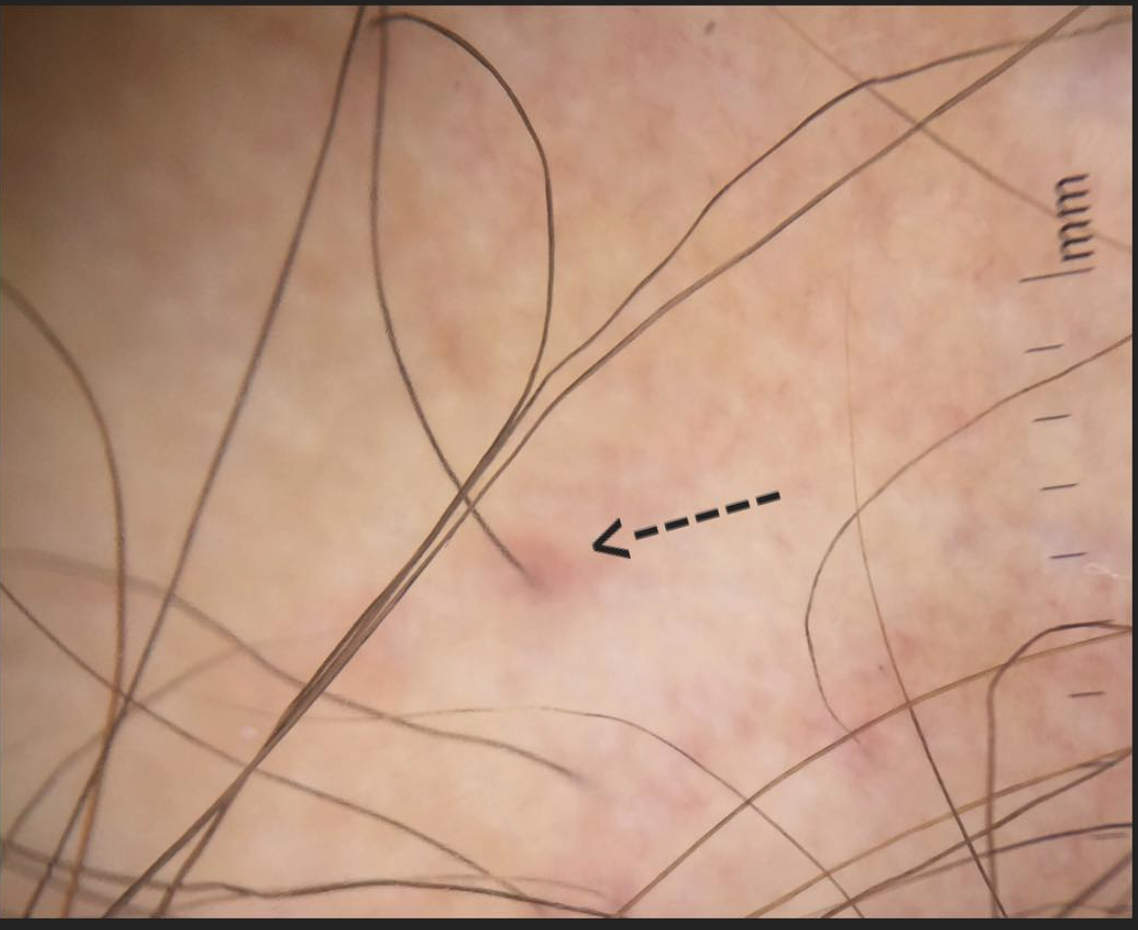
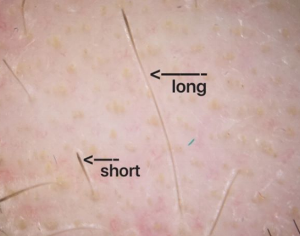
Trichoscopy is completely wonderful. It helps me tremendously in the diagnosis of many non scarring alopecia. Most cases of androgenetic alopecia can be diagnosed with trichoscopy but not all! In fact, unless one is very experienced with trichscopy, the early cases of AGA are going to be very challenging to diagnose by trichscopy because there is just not enough miniaturization that has developed yet. So, if a patient buys a trichoscope and sees that their is not much miniaturization, can they conclude they don’t have AGA? No.
Most cases of acute alopecia areata can be diagnosed with trichoscopy. This is certainly one area where trichoscopy is very helpful. But in cases of advanced AA and some cases of alopecia areata incognito, all that might be seen is miniaturization of hairs. It can be difficult to render the diagnosis from trichscopy alone. So how do we diagnose it? Listen to the patient’s story!
Telogen effluvium (TE) refers to a type of hair shedding and is one of the more common diagnoses in women. Guess what? Telogen effluvium has NO definitive specific diagnostic trichoscopic signs ! Yikes! it’s true that the presence of many upright regrowing hairs can be a tip off from trichoscopy that the diagnosis of TE might be present - but it’s not specific. If a person thinks they are going to diagnose their TE by buying a trichoscope, they are wrong.