Are patients with seborrheic dermatitis at risk for osteoporosis?
New Study Links Seborrheic Dermatitis With increased risk of Osteoporosis
Osteoporosis is a systemic bone-resorbing disease that causes bone fragility and subsequent risk of fracture. The WHO 1996 definition of osteoporosis includes four key components: 1) low bone mass, 2) microarchitectural detioration, 3) increase in fragility as a result of these and 4) increased susceptibility to fracture.
in addition, osteoporosis has been defined based on bone mineral density (BMD) assessment. According to the WHO criteria, osteoporosis is defined as a BMD that lies 2.5 standard deviations or more below the average value for young healthy women (i.e. a T-score of < − 2.5 SD).
Risk Factors for Osteoporosis
Risk factors for osteoporosis are divided into two categories: modifiable and non-modifiable. Modifiable risk factors include low body weight, smoking, alcohol consumption, lack of exercise, deficiency of dietary calcium, and long-term glucocorticoid use. The non-modifiable group includes gender, age, race, and genetic characteristics.
In a recent meta-analysis by Salari et al, the prevalence of osteoporosis in the world was 18.3%, which was calculated based on reports of the prevalence of osteoporosis from 86 studies across five continents.The sample size of the study was 103,334,579 people in the age range of 15–105 years. Subgroup analyses showed that for women the prevalence was 23.1 % and for men it was 11.7 %.
Seborrheic Dermatitis (SD)
Seborrheic dermatitis is an inflammatory skin condition that affects about 5 % of the world. It is thought to be multifactorial in nature with Malassezia yeast playing an important role in the condition. Changes in skin microbiome, as well as environmental factors play a key role too. All of the factors have yet to be fully worked out. The most common sites of SD, known as “seborrheic areas,” are the anterior chest, axilla, back, groin, central area of the face, and scalp. The incidence of SD is highest in infants, adolescents, and adults aged 30–60 years.
Risk Factors for Seborrheic Dermatitis
There are many well known risk factors for SD. Many of the seborrheic dermatitis risk factors are shown in the image below. They include
a) Row 1, top, left to right: neurological conditions like Parkinson’s and tardive dyskinesia, stress, being male, HIV, winter months.
b) Row 2, middle, left to tight: depression, sleep deprivation, humidity, Western diets, excess alcohol.
c) Row 3, bottom, left to right: darker skin types, altitude, some medications, lymphoma and immunosuppressive states).
Although the the prevalence of SD is approximately 5% in adults, the prevalence is known to be even higher in immunocompromised individuals (including HIV/AIDS) and in those with neurologic disease (such as Parkinson’s disease and multiple sclerosis).
Is SD a risk factor for osteoporosis?
Authors from Taiwan were interested to study whether patients with SD have an increased risk for osteoporosis. They stated that this interest came about given that osteoporosis and SD share a similar pathobiology, namely inflammation and hormonal imbalance, The authors there set out to investigate whether the existence of SD increases osteoporosis risk using a large database known as the Taiwan National Health Insurance Research Database. The authors compared the risk of osteoporosis in patients with SD to the risk of osteoporosis in patients without SD.
The study group include 7831 patients aged 18–50 years with SD. The control group included 31 324 patients without SD. Patients were matched by age, gender, Charlson Comorbidity Index, and index date at a ratio of 1:4 during 1996–2010.
Key Results
Compared to the non-SD group, the SD group had a higher prevalence of diabetes mellitus, hyperlipidemia, high blood pressure, chronic liver disease, hyperthyroidism, depression, stroke, dementia, and psoriasis.
Overall, the authors showed that 0.98% of patients with SD had osteoporosis. This was 0.66% in the non SD group. Compared to the non-SD group, this translated to a 5.95-fold higher osteoporosis risk in patients with SD compared to patients without SD (after adjustment for variables). (2.42 vs 0.44 per 1000 person-years, respectively) after adjustment for age, gender, CCI, and comorbidities
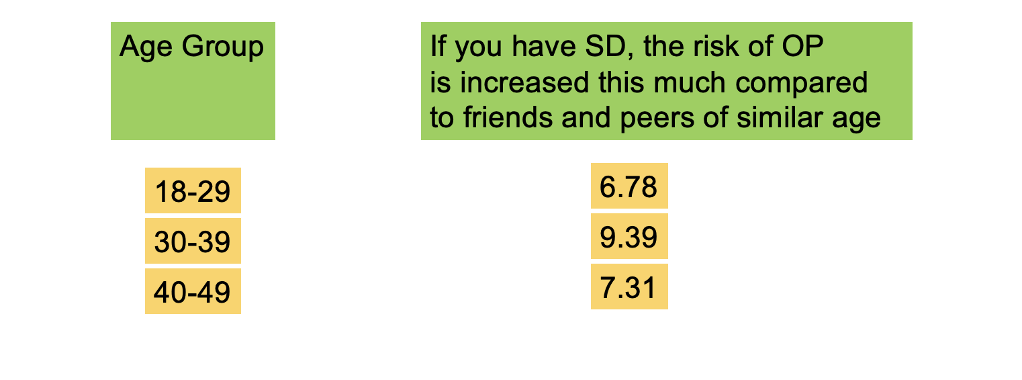
Although all patients with SD had an increased risk of OP, the impact of SD on osteoporosis risk was found to be the largest in the female and young age groups. In other words, although older patients with SD were more likely to have OP than younger patients with SD, and older patients with SD were more likely to have OP than older patients without SD, younger patients with SD were more likely to have SD compared to patients without SD in the same age group.
Additionally, the SD group tended to develop osteoporosis more rapidly (2.2 years after enrolment) compared to the control group (8.9 years after enrolment).
In addition, the authors found that the presence of hyperlipidemia, hyperthyroidism, and epilepsy synergistically increased osteoporosis incidence in the SD group.
Females with SD Have Higher Risk for OP than Males with SD
In gender-specific analyses of SD patients, the osteoporosis risk in SD patients was higher in females compared to males (adjusted HR = 7.36, 95% CI = 5.15–10.52 for females; adjusted HR = 3.80, 95% CI = 1.95–7.38 for males).
Which patients with SD are most likely to have OP?
Among patients diagnosed with SD, the risk factors for osteoporosis included advanced age, female, high CCI, hy- perlipidemia, hyperthyroidism, and epilepsy.
Conclusion
This first large cohort study demonstrated an association between SD and osteoporosis. There is a 5.95-fold higher risk of osteoporosis in those with SD compared to controls after adjustment for comorbidity.
The reasons are not clear and this study did not set out to identify the actual reasons. SD is an inflammatory systemic disorder associated with altered the skin microbiome. In this study, SD patients had a high prevalence of depression, hypertension, hyperlipidemia, and diabetes mellitus. Therefore the authors wonder whether seborrheic dermatitis may contribute to osteoporosis risk by increasing the risks of metabolic syndrome. However, these complex associations need further study and hopefully this study will fuel further such studies
One limitation is that the database could not control for all risk factors in the analysis. The database lacked detailed data for osteoporosis risk factors such as genetic factors, family history, sun exposure, diet/exercise habits, tobacco and alcohol consumption, and body mass index.
In conclusion, this study is the first cohort study to demonstrate that SD patients have an increased risk of osteoporosis, especially when the patient with SD has hyperlipidemia, hyperthyroidism or epilepsy.
It was particularly interesting to note the influence of SD on osteoporosis risk was largest in young age groups. Young patients sill have a much lower risk for OP overall but SD bumps this risk up quite a bit.
REFERENCE
Ying-Yi Lu et al. Impact of seborrheic dermatitis on osteoporosis risk: A population-based cohort study. J Dermatol. 2022 Sep 12.
Salari N et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021 Oct 17;16(1):609. doi: 10.1186/s13018-021-02772-0.PMID: 34657598
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.