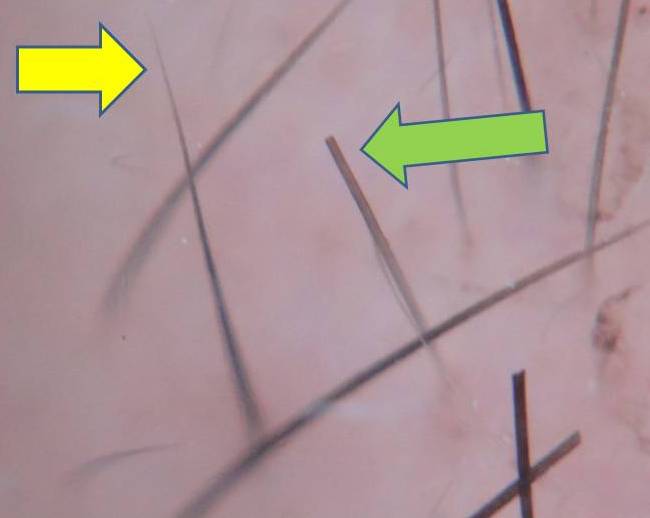
There are over 100 reasons to lose hair. Sometimes the reason a person is losing hair (i.e. the diagnosis) is obvious as soon as I meet the patient. Othertimes, a small scalp biopsy is needed in order to examine the hairs under the microscope before reaching the final diagnosis.
A previous blog of mine reviewed how a scalp biopsy is performed. The procedure takes about 15 minutes and is performed using local numbing medicines. An important question patients ask is:
Should I be applying an antibiotic cream or ointment from the drug stores to my stitches after the procedure in order to help prevent infection?
The answer is straightforward for the vast majority of scalp biopsies I do: No.
Antibiotic creams or ointments are usually not required for patients undergoing a scalp biopsy. Numerous studies have shown that about 1 to 2 % of patients undergoing simple skin surgeries willl develop an infection. But more importantly, the risk is not reduced if patients use an antiobiotic cream or ointment. In fact, the unnecessary use of a topical antibiotic might increase the risk of developing an allergy to one of the ingredients (like neomycin or bacitracin).
Fortunately, the message is catching on among physicians that we don't need to use topical antibiotics for most procedures. A recent study showed that between 1993 and 2007 there were about 212 million routine skin surgery procedures in the USA. Topical antibiotics were used in about 6 % of those procedures. Fortunately, the researchers showed that the use of topical antibiotics has decreased over time (from about 7 percent back in 1992 down to about 3 percent at the present time).
Exceptions, of course, do exist. If a patient has very poorly controlled diabetes or they are immunosuppressed the use of oral antibiotics before a procedure might be recommended. Similarly, I might consider antibiotics if a patient has certain types of problems with their heart valves or recently had a hip or knee replacement.
But more often than not, patients do not need to use antibiotic creams or ointments after their scalp biopsy. Petroleum jelly might be recommended to simply keep the area moist and speed up healing.
References
1. Levender MM et al. Use of topical antibiotics as prophylaxis in clean dermatologic procedures. Journal of te American Academy of Dermatology 2012; 66:445-51.
2. Smack DP etal. Infection and allergy incidence in ambulatory surgery patients using white petrolatum vs bacitracin ointment: a randomized controlled trial. JAMA 1996; 276:972-7
3. Campbell RM et al. Gentamycin ointment vs petrolatum for management of suricular wounds. Dermatol Surg 2005; 31;664-9.
4. Dixon AJ et al. Randomized clinical trial of the effect of applying ointment to surgical wounds before occlusive dressing. Br J Surg. 2006; 93:937-43.