Scarring alopecias may respond well to treatment are the patient will experience a halting of their hair loss and symptoms (if symptoms are present).
In some cases, relatively “inactive” scarring alopecias may become “active” again and cause further symptoms and hair loss. We call such unexpected reactivation a “flare.”
Reasons for a Flare of Scarring Alopecia
Here we review considerations that must be given for any patient with scarring alopecia who experiences a flare. When I work with doctors or give lectures, I frequently use the teaching tool or mnemonic "I'M WORSE" to review causes of a flare. Each letters stands for considerations that must be evaluated.
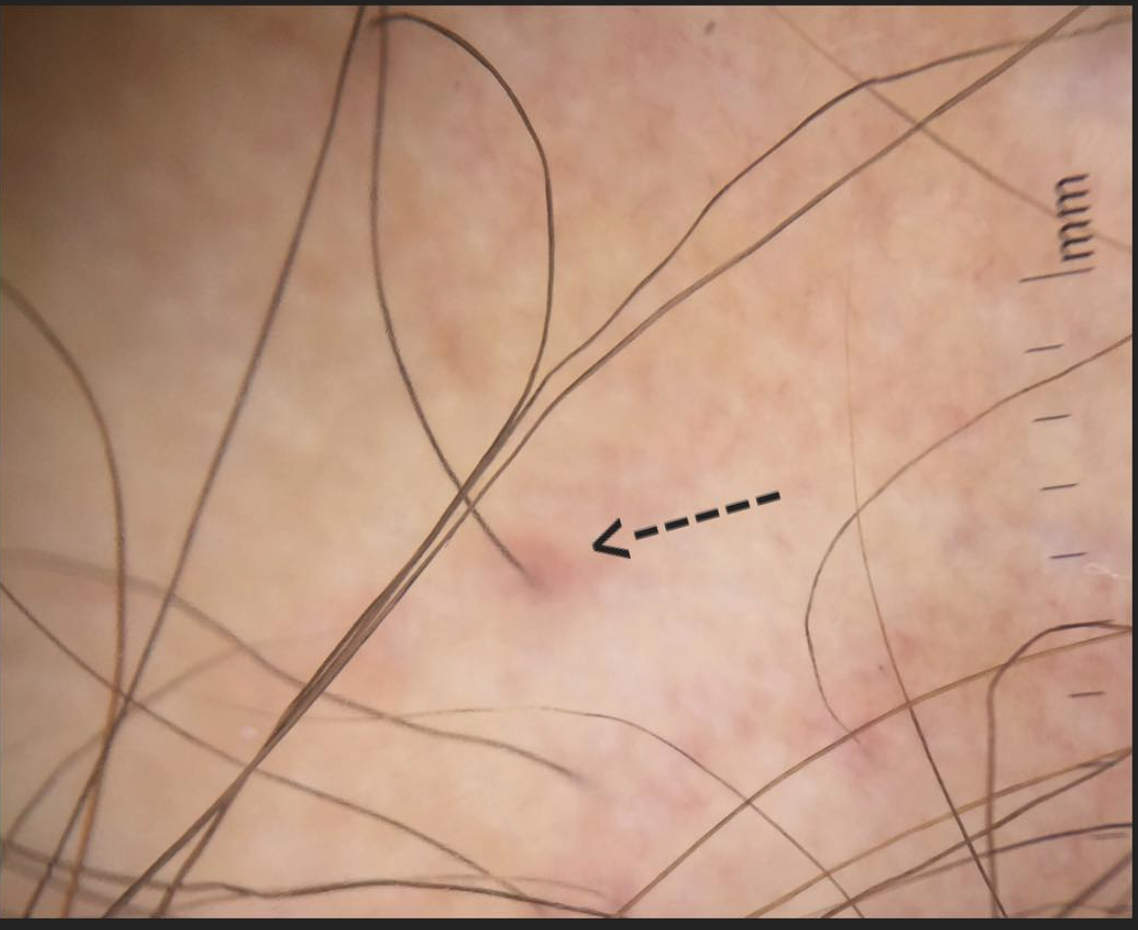
I = Injury to the Scalp
Scalp injury can worsen many scarring alopecias and trigger a 'flare' in patients who had otherwise quiet disease. There can be many potential sources of such injury including a direct blow (i.e. something strikes the scalp), a massive sunburn or scalp surgery. In the latter category, a hair transplant is an example of a surgical procedure that can potentially trigger a flare in a patient with a scarring alopecia. For this reason, a hair transplant is never an option for patients with scarring alopecia that is not completed quiet.
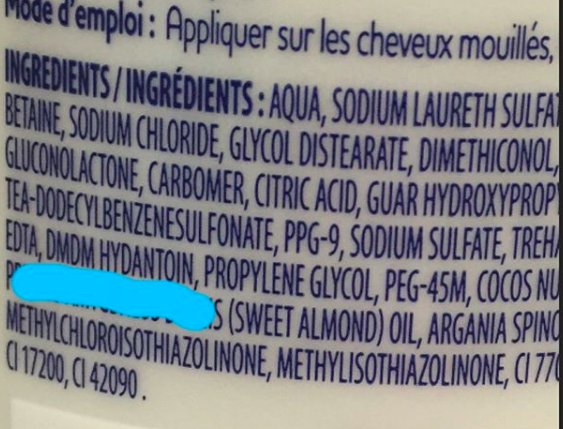
M = Medications are making it Worse
In some patients who are experiencing “flares” of their scarring alopecia, it is sometimes the medication itself that is causing things to worsen. Occasionally patients prescribed steroids injections, steroid shampoos, hydroxychloroquine, methotrexate, minoxidil, or retinoids find their hair loss has worsened on account of a specific drug or topical product.
This is a challenging category to evaluate but does need careful consideration. Occasionally for example a patient with relatively stable disease who adds minoxidil in hopes to stimulate more hair growth finds that minoxidil triggers worsening shedding and dryness that seems to flare things overall. Similarly, there are some patients who find that steroid injections similarly trigger a flare.
W = Wrong Medication or Dose
It is not common for medication dosing errors to be the main reason for a flare. Nevertheless it needs to be considered. A patient who changes their dose after getting a prescription refill could find that this change triggers a flare. For topical medications that are compounded, one must consider that the method use to compound the drug may changed.
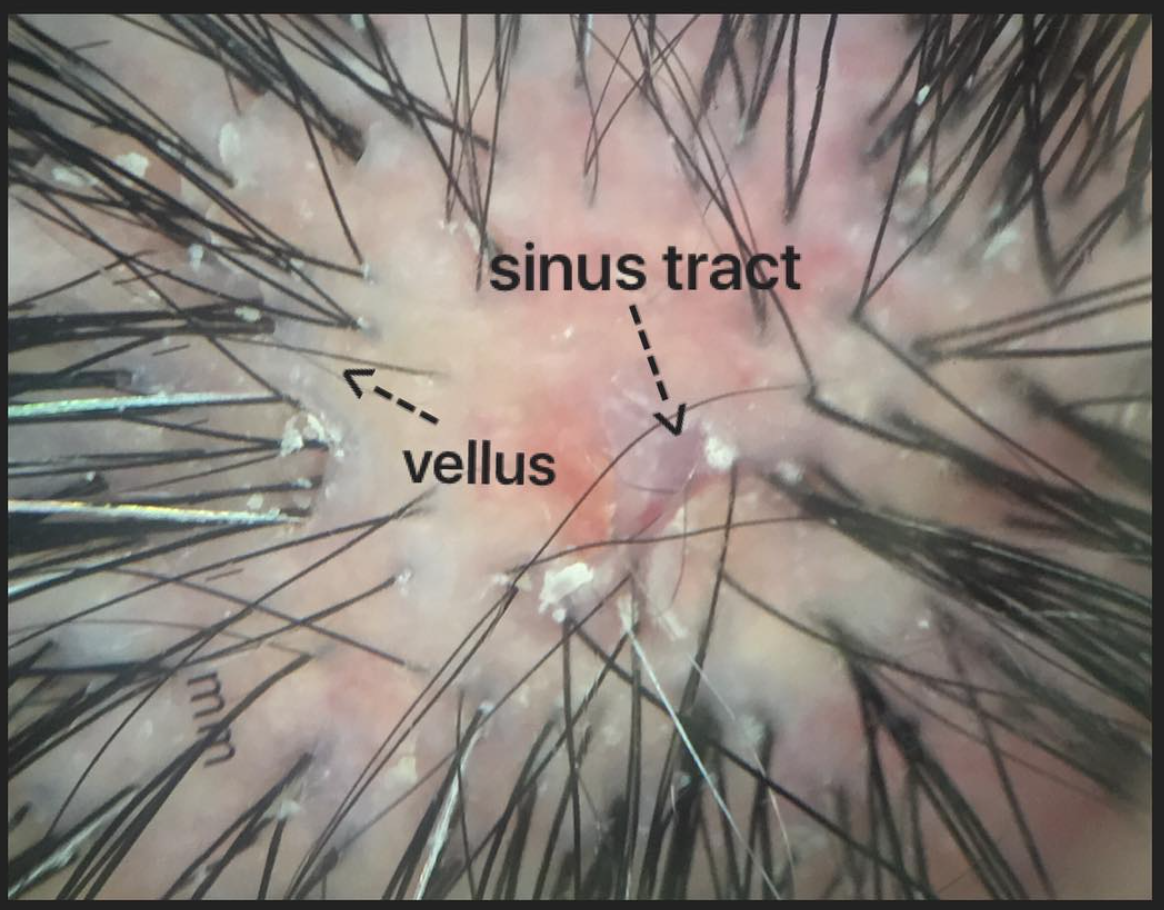
O = Other Condition Developed or Worsened
For a scarring alopecia may be perceived to have worsened, one must keep in mind that it could actually be a completely separate medical issue that has triggered the worsening rather than the scarring alopecia itself. A example would be the development of iron deficiency in a patient with lichen planopilaris that triggered a worsening of hair loss. The key treatment in this scenario is to treat the iron deficiency rather than more aggressively treat the scarring alopecia. Similarly, in a patient with stable LPP who develops hyperthyroidism (and hair loss from the thyroid disease) the perception to the patient is likely to be that their scarring alopecia is worse. In reality, their scarring alopecia may be stable but they have a second condition that has developed and it too is causing hair loss.
Seborrheic dermatitis and S. aureus related infections can rarely make scarring alopecia worse as well. Seborrheic dermatitis is very common in scarring alopecia so one should always consider this entity.
R = Rejection of Prescribed Medications (Medication Compliance/Adherence)
For a patient whose scarring alopecia is flaring, one needs to consider the possibility that the patient is not using the medication in the manner that was intended. An example could be a patient who was supposed to use doxycycline for 6 months but stopped it after two months. In such situations it is important to inquire about the exact reason the medication was stopped prematurely. In some cases, it may due to side effects that prompted stopping the medication or other factors such as cost. We know that a very large proportion of patients do not take their medications in the manner prescribed. So a physician should never assume adherence to the treatment protocol
S= Stressful life events
For patients with scarring alopecia, stress is a potential trigger of a “flare” of scarring alopecia. Many patients with scarring alopecias such as lichen planopilaris, pseudopelade, frontal fibrosing alopecia, folliculitis decalvans notice that the scalp can become considerably more itchy around times of intense stress. This may be stress related to work or family, personal relationships, finances or other issues. All have the potential to trigger a flare.
E= Enigma (NO clear reason)
The last category is the most common. Most of the time, the exact cause of a patient's “flare” is not known. The disease just wants to get worse. We see this sort of phenomenon in nearly every immune based disease known to humans. Despite all factors being reviewed, it just does not seem clear why a patient who was stable for so many months is now experiencing worsening of their disease (i.e. a flare). There is much about the immune system in the present day and age that we simply do not understand. The immune system can become active for reasons we do not understand. In this situation, additional treatment is needed to halt inflammation.