Diphencyprone (DPCP) For Patients with Breast Cancer
I’ve selected this question below for this week’s question of the week. It allows us to discuss some of the finer aspects of using a treatment for alopecia areata that some are unfamiliar with - diphencyprone .
Here is the question….
Question
I am a late 60s year old woman and I have had Alopecia Areata verging on Totalis, for 20 years. I have tried cortisone injections, minoxidil, simvastatin, etc., with varying results. Finally I used DPCP starting summer 2018 and had a good response by early Spring 2019. I even had 2 haircuts! But by mid summer 2019, some new bald patches appeared. I was diagnosed with breast cancer in the Fall of 2019, at which point DPCP was stopped. Hair shedding continued for the next 2-3 months. I had 2 surgeries to remove the cancer in the last few months of 2019, then radiation for 4 weeks in early 2020. I noticed diffuse patchy hair regrowth in January and now have approximately 70% regrowth coming in.
Question 1:
With the removal of the tumor, and associated immune stimulation, could this affect the beginning of hair regrowth?
Question 2:
I there a known link between DCPC use and my breast cancer?
Question 3:
Should I continue using DCPC in the future?
Answer
Thanks for the great question. First, I hope you are doing well after your surgery and treatments. As far as alopecia areata and breast cancer goes, we don’t have a lot of good evidence to link the removal of the breast cancer and the ability of the hair to grow back. It is certainly possible. Of course, the “how likely” this is probably depends a bit on the patient’s cancer exact histological type, size, etc. A small tumor is going to stimulate the immune system differently than a large tumor. A localized tumor is going to stimulate the immune system differently than a cancer that has spread.
We don’t have any evidence that diphenycprone enters the blood to any significant degree and we we don’t have evidence that there is no known link to DPCP and breast cancer.
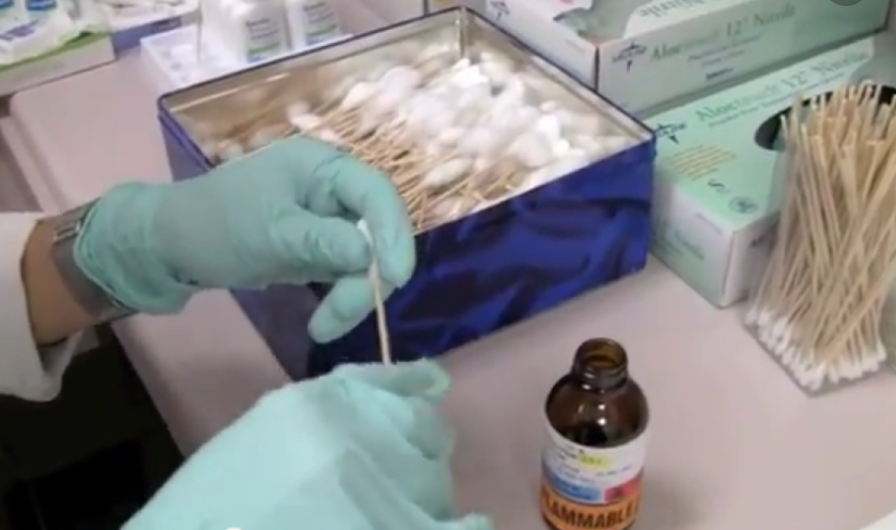
See previous article : Does DPCP Get absorbed ?
DPCP is not an immunosupressing medication and has its advantages for patients with alopecia areata with a previous diagnosis of cancer. It also has advantages for patients with alopecia areata with a previous diagnosis of cancer who are going through a pandemic due to COVID 19. You’ll clearly want to speak to your dermatologist about all the facts as I don’t have all the facts in front of me with the information given in this question. But it’s quite likely that returning to DPCP is an excellent option.
Thank you again for the great question.
References
[1] Can one apply DPCP at home?