The LPP - FD Overlap Syndrome (LPP-FD Phenotypic Spectrum)
What is the LPP- FD Phenotypic Spectrum ?
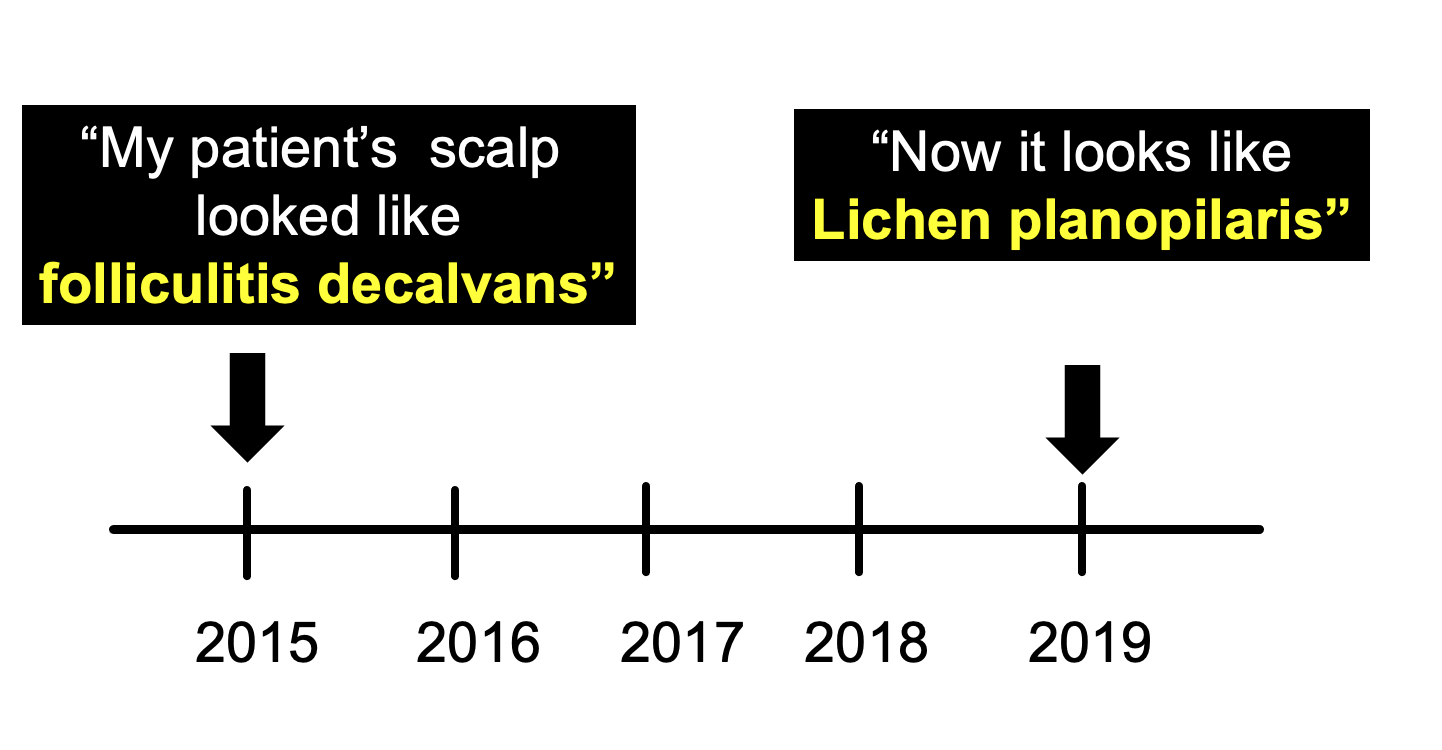
The LPP FD Phenotypic Spectrum (LPPFDPS) is a very interesting phenomenon. I refer to it as the LPP FD Overlap Syndrome because it helps to better remember that this is a hair loss condition with overlapping features of both folliculitis decalvans and lichen planopilaris. Typical, the patient’s hair loss starts out more looking like folliculitis decalvans and then starts resembling lichen planopilaris over time.
When this situation is encountered, many clinicians scratch their own head in confusion wondering if they made the right diagnosis. Does my patient have FD or LPP? Did I make a mistake in the diagnosis ?
This is the LPP FD phenotypic spectrum in action!
Two Key Studies from 2020: The Yip et al and Egger et al Studies
The LPP-FD Overlap syndrome has sheen recognized for quite a few years by hair loss experts. Surprisingly, there were few studies to document the phenomenon and do describe more about it. That all changed inn 2020 when a study by Yip et al and then Egger et al provided the world with more information
Study 1: Yip et al, 2020
Yip, Barret and Harries reported in the journal Clinical and Experimental Dermatology 13 patient who had clinical features of both FD & LPP - either sequentially or over time. The patients in their study often started out with having folliculitis decalvans (with tufting and pustules) and then changed over time to have more of a lichen planopilaris like phenotype (with perifollicular scaling and erythema). There were times were the pathology of the scalp show true folliculitis decalvans features (with a mixed infiltrated and time where the biopsy showed more of a LPP like histology.
Study 2: Egger et al, 2020
Egger described seven patients who had concomitant features of both FD and LPP. These patients had a recalcitrant course and patients were unresponsive to topical and systemic immunomodulatory and anti-inflammatory treatments.
There were several features that these patients had inn common inlcuding
1) clinical evidence of polytrichia on scalp exam (fusing of follicles together)
2) histology showing the compounding of follicles.
3) positive bacterial cultures in 50 % of patients
4) improvement in clinical course with administration of antimicrobials
Summary and Conclusion : What’s it all mean ?
It’s easy to feel confused when you first encounter the LPP FD Overlap syndrome (“phenotypic spectrum). One need not be confused. There are situations where patients with folliculitis decalvans have scalp that look like LPP ! That’s all there is to it.
Nobody knows why that it is - only that it is.
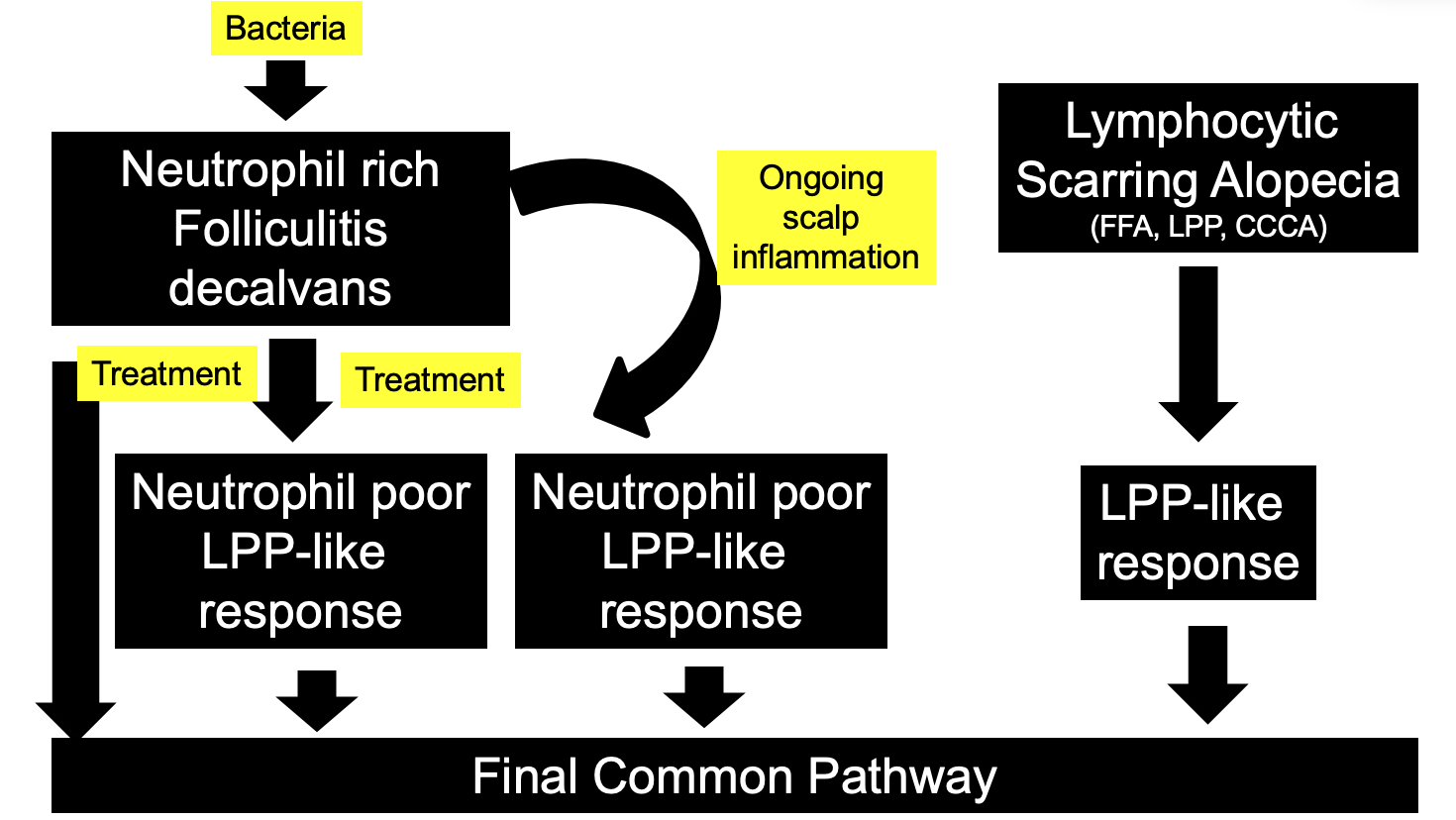
It may be that when bacteria are in the scalp, patents who are predisposed to folliculitis decavlans develop certain changes in the scalp that resemble FD. When the bacteria go away, and immune system may still be programmed to damage hairs - and the mechanism it elects to take is sometimes an LPP-like damage pathway. Similarly it could be that once the scalp starts getting damaged in FD, lots of inflammatory signals get sent out in the scalp - and some of these signals cause an LPP like change.
Sometimes when inflammation goes away, the scalp is just left with scar tissue and resembles what every other scarring alopecia looks like when inflammation goes away.
The problem with modern hair science is that we think of LPP as one disease. It’s not quite like that. It’s a reaction pattern. Biopsies of LPP looks the same as biopsies of frontal fibrosing alopecia and biopsies of frontal fibrosing alopecia look the same as biopsies of central centrifugal cicatricial alopecia. Why is this? Well, the hair follicle only knows how to create a limited number of changes when things go wrong. These are all different diseases but the hair still undergoes similar changes when the inflammation is present.
With certain inflammation in the scalp, the hair follicle undergoes a FD like change. When the inflammation is just a little bit different, it takes on a LPP-like change. Eventually, long standing folliculitis decalvans and long standing LPP can look similar.
There are several important concepts to keep in mind when thinking about this LPP FD phenotypic spectrum:
1) Don’t be confused if your FD patients start looking like they have LPP
2) Don ‘t be confused if your LPP patients start looking like they have FD
3) If your LPP patients are not responding to treatment ask yourself if they might have FD
4) If your FD patients are not responding to treatment, consider LPP like transition
There are four features which I refer to as the “four P’s of LPP” which might give a hint that the LPP patient in front of the doctor might have folliculitis decalvans or an LPPFDPS rather than a true LPP:
P - Pustules and crusts (the patient has pustules and crusts on the scalp!)
P - Polytrichia (the patient has compound follicles!)
P - Purpura and bleeding (the patient has evidence of bleeding!)
P- Plasma cells on biopsy (the patient’s biopsy has plasma cells)
Reference
Folliculitis decalvans and lichen planopilaris phenotypic spectrum: a case series of biphasic clinical presentation and theories on pathogenesis.Yip L, Barrett TH, Harries MJ.Clin Exp Dermatol. 2020 Jan;45(1):63-72.
Folliculitis Decalvans and Lichen Planopilaris Phenotypic Spectrum-A Series of 7 New Cases With Focus on Histopathology.Egger A, Stojadinovic O, Miteva M.Am J Dermatopathol. 2020 Mar;42(3):173-177.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.