Doc, Should I start a JAK Inhibitor for my Alopecia Areata?
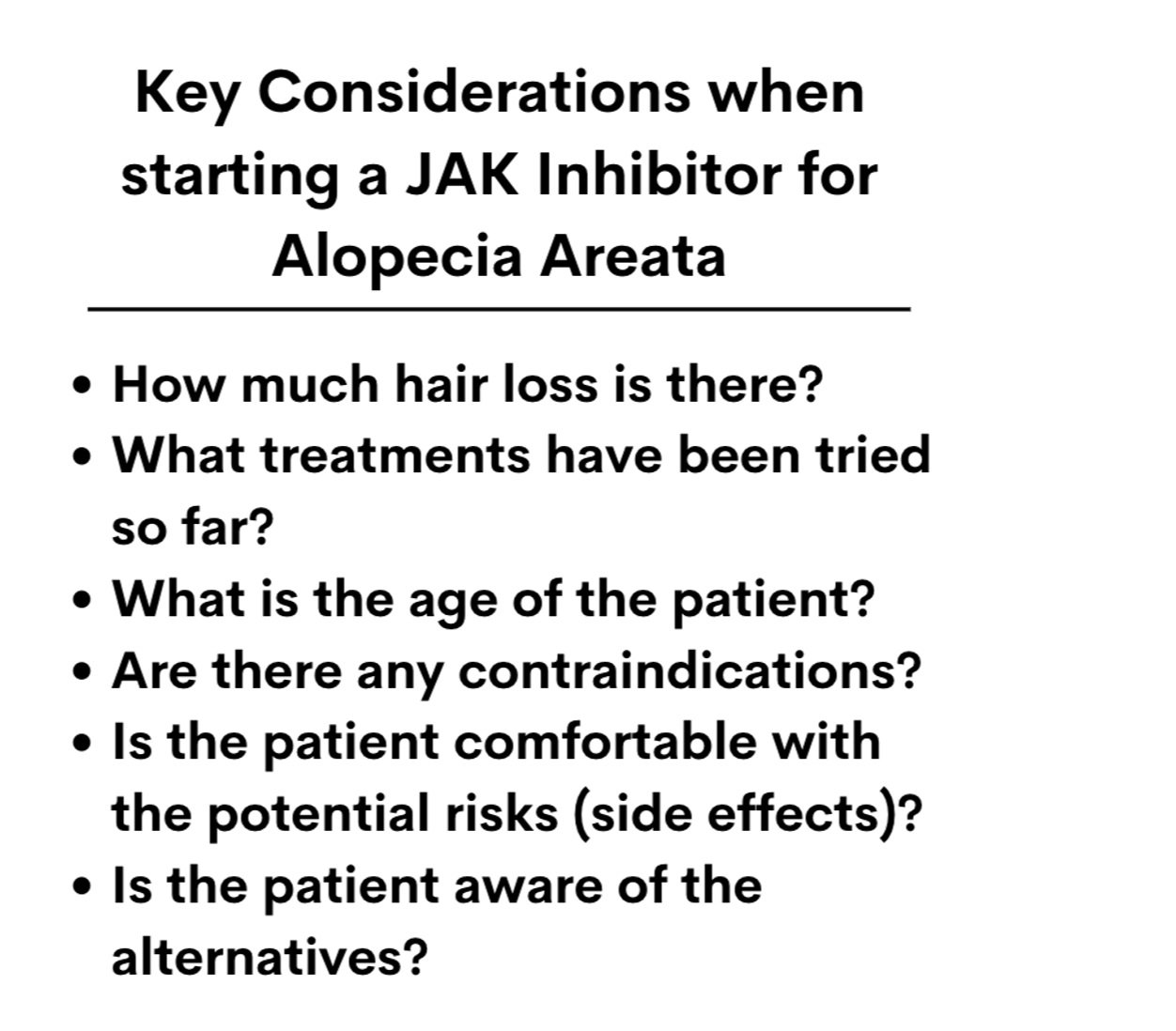
Key Questions to Answer Before Starting A JAK Inhibitor for Alopecia Areata
JAK Inhibitors are rising to the top of the list as treatment options for adult patients with severe alopecia areata. I’m often asked by patients “Should I start a JAK inhibitor, doc?” Let’s take a look at some key issues that each patient needs to answer either themselves - or with the help of their doctor - before starting a JAK Inhibitor like baricitinib, tofacitinib, ruxolitinib, upadacitinib or abrocitinib.
QUESTION 1. How much hair loss is there?
There is no strict cut off for how much hair loss a person really needs to have in order to start a JAK inhibitor. We will come back to that important point in a moment. But a person with 29 % scalp hair loss who also has eyebrow and eyelash hair loss and who has not had success with other treatments for their alopecia areata can certainly consider a JAK inhibitor.
However, if one lives in the United States, and hopes that his or her insurance company will cover the high cost of the drug - one will probably need to have at least 50 % hair loss. That’s the cut off to define severe alopecia areata. The drug baricitinib was FDA approved June 13, 2022 for adults with severe alopecia areata. The company studied adults with severe alopecia - and not any other group. So that’s the cut off that the FDA approved - and that’s the cut off that insurance companies are likely to approve.
Is someone with 49 % hair loss considered a patient with a potential FDA approved indication for the drug? Well, no. Not technically. You can see the silliness of the cut offs and how long we have to go to develop consistently sound criteria for who should be considered a candidate for these drugs. But these are the rules. Let’s review this one more time - baricitinib is FDA approved for severe alopecia areata in adults (50 % or more scalp hair loss).
Can someone with alopecia areata use baricitinib with 33 % hair loss? That’s possible, yes - assuming that the patient understands all the risks and benefits and has no contraindications to the drug and understands all the alternatives and assuming the prescribing doctor feels that’s a good option. Otherwise, the answer is no. In this case, the person with 33 % hair loss is said to be using the drug ‘off label.’ They are not using it in the way it was FDA approved. We use many, many treatments in clinic off label so this is really nothing new to a hair specialist.
The reason these cut-offs exist is simple: Many patients with less than 50% scalp hair loss may do just as well, if not better, with other treatments. Does a patient with 10 % hair loss need to start a JAK inhibitor? Probably not. A solid plan with steroid injections and topical steroids and topical minoxidil will probably help regrow hair just as good as a JAK inhibitor. It’s also a safer and cheaper plan.
QUESTION 2. What is the age of the patient?
JAK inhibitors have been studied in adults and children with alopecia areata. Most of the data pertains to adults but there is accumulating data in children and adolescents too. In fact, current studies suggest that JAK inhibitors are just as effective in children and adolescents with alopecia areata as they are in adults with alopecia areata. We must not forget that JAK inhibitors are not approved in patients with alopecia areata under the age of 18. And so any doctor who wishes to prescribe a JAK inhibitor to a patient with alopecia areata under the age of 18 is prescribing that drug ‘off-label.’
That’s not to say JAK inhibitors are not approved in pediatric patients. The JAK inhibitors upadacitinib and abrocitinib are now both FDA approved for adolescents 12-18 with severe atopic dermatitis (eczema). So, there’s reason to believe that the drugs have good short term safety in pediatric patients.
But JAK inhibitors are not formally approved for alopecia areata in pediatric patietns with alopecia areata.
Clinical trials are on the way. In fact, the FDA is currently reviewing data on the JAK inhibitor ritlecitinib for patients age 12 and over. So we may see approvals for pediatric patients in the near future.
JAK inhibitors are also not recommended for those over 65. The BRAVE AA trials that led to the FDA approval of baricitinib studied males 18-60 and females 18-70. The average age was around 37 years. Patients above 60 are not well studied and in fact several groups warn against using JAK inhibitors in older patients.
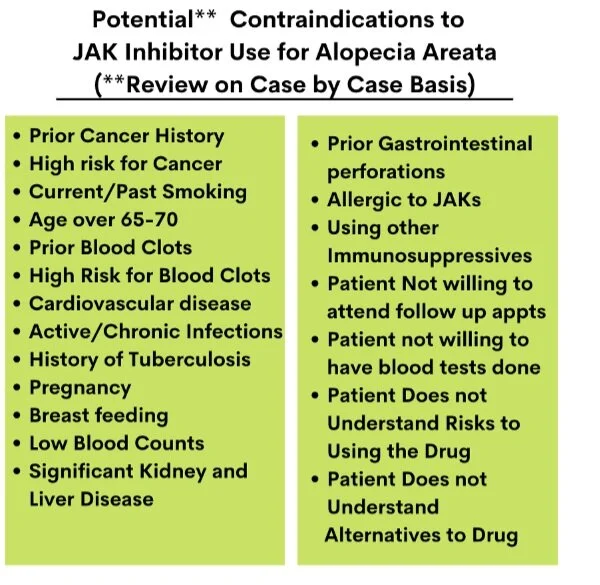
QUESTION 3. Are there any contraindications?
Not everyone with alopecia areata should use a JAK inhibitor even if they do have 50 % or more hair loss. There are many contraindications - or reasons why this might not be started. Patients with cancer, prior blood clots, prior smokers, patients with cardiovascular disease (including heart attacks and strokes) are not good candidates for JAK inhibitors. Furthermore, patients over the age of 65 are not great candidates either and this presents a relative contraindication. Patients with current infections including some chronic infections, may not be good candidates.
QUESTION 4. Is the patient comfortable with the potential risks (side effects)?
Not everyone with alopecia areata should use a JAK inhibitor even if they do have 50 % or more hair loss. Patients who are not comfortable with the potential risks of these drugs should not use these drugs. Potential risks include heart disease, strokes, cancer, death, blood clots, risk of infections, changes in blood counts, elevated cholesterol, elevated muscle enzymes and others. Fortunately, the risks for some of these issues are fairly small. In addition, we don’t even know if the risks for some issues like heart disease and strokes and cancer and blood clots even apply to patients with alopecia areata. They seem to apply to other patients - like those with rheumatoid arthritis - but we just don’t know if they apply to those with alopecia areata. Maybe they don’t. Maybe they do. Long term studies are non-existent in patients with alopecia areata. So more study is needed.
QUESTION 5. Is the patient aware of the alternatives? Does he or she prefer the alternatives?
Not everyone with alopecia areata should use a JAK inhibitor even if they do have 50 % or more hair loss. Patients who feel that the alternative options are better for them should probably strongly consider the alternative options. A given patient may feel that a trial of oral steroids is a better option for them than a trial of a JAK inhibitor. A given patient may feel that methotrexate is a better option for them than a trial of a JAK inhibitor. A given patient may feel that wearing a wig is a better option for them than a trial of a JAK inhibitor. A given patient may feel that scalp micropigmentation is a better option for them than a trial of a JAK inhibitor. A given patient may feel that not pursuing treatment is a better option for them than a trial of a JAK inhibitor. People are all different when it comes to their views and decisions.
Patients needs to understand the alternatives before starting a JAK inhibitor. That’s called informed consent. What else can be used if a JAK inhibitor is not prescribed and what are the risks and benefits and costs of those alternatives?
Conclusions
JAK inhibitors are increasingly used in the treatment of alopecia areata. It is important to be aware of the formal FDA approved indications as well as contraindications and side effects of the drug. In addition, it’s important for patients to be aware of alternative options and reflect on whether these alternatives are better options for them than the drug or not.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.