Distinguishing Alopecia Areata from AGA when "Peribulbar" Infiltrates are Lacking
How Can we Differentiate Alopecia Areata from Androgenetic Alopecia When Peribulbar Infiltrates are Lacking?
Alopecia areata is an autoimmune hair loss conditions that may cause hair loss from any hair bearing site. Biopsies are not generally needed to diagnose alopecia areata, but may be helpful in challenging cases.
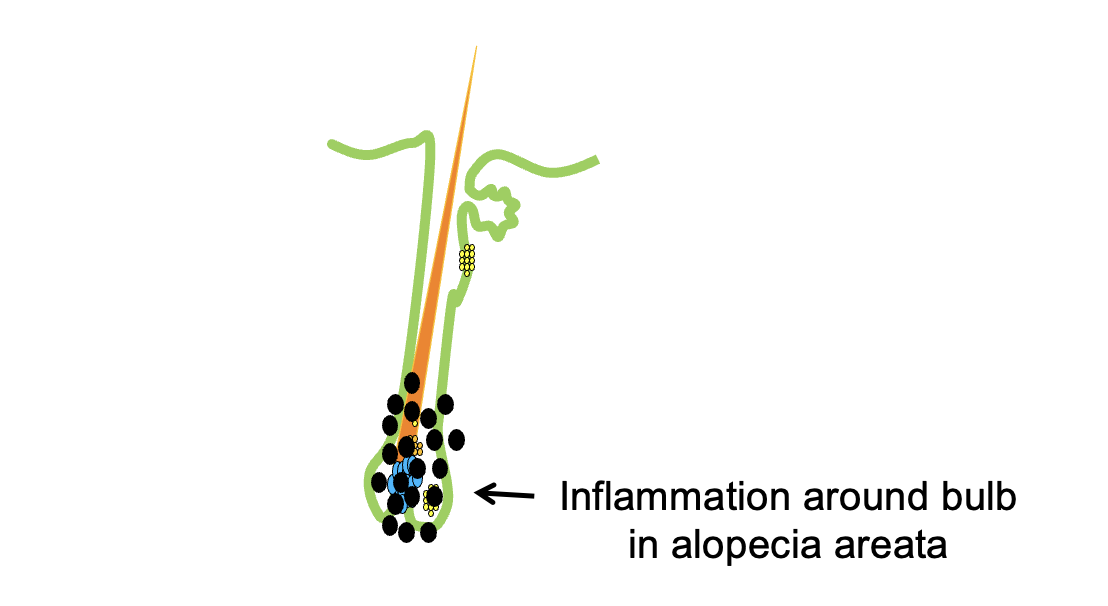
The classic histology that everyone learns about in diagnosing alopecia areata is inflammation around the bulb. This is called peribulbar inflammation. A schematic diagram of the peribulbar inflammation is shown below:
So how can we diagnose alopecia areata when peribulbar inflammation is not seen? Well other findings can be helpful to differentiate alopecia alopecia (AA) from androgenetic alopecia (AGA).
Plante et al 2023
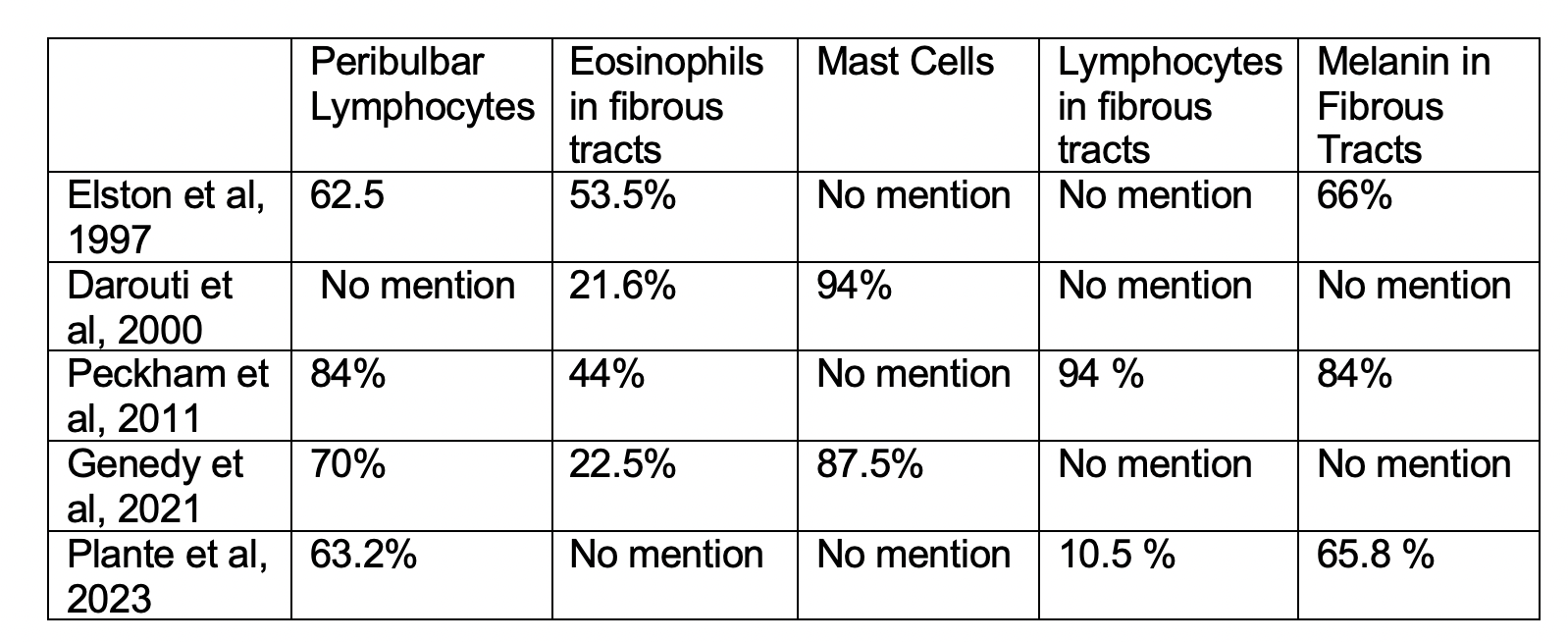
Authors of a new study set out to determine which histopathologic features are most useful for differentiating AA from AGA To do so, the authors performed a retrospective review of AA and AGA scalp biopsy specimens from 2014 to 2019 at a tertiary referral center. There were 96 cases analyzed. 38 were AA biopsies and 58 were AGA biopsies. Peribulbar infiltrates were identified in 63.2% of AA cases. A catagen/telogen shift (meaning more than 20 % of hairs in catagen or telogen) was observed more frequently in AA than PHL (65.5% AA vs. 17.2% AGA; p ≤ 0.0001). Lymphocytes and melanin were more common in fibrous tracts in AA than AGA. Specifically, lymphocytes were present in 10.5% AA vs. 1.7% AGA p = 0.058). Melanin was present in fibrous tracts in 65.8% AA vs. 8.6%; AGA p ≤ 0.0001). Apoptotic bodies within vellus hairs were more frequently identified in AA than AGA (84.2% vs. 63.8%; p = 0.030). Small dystrophic follicles were also more common in AA than AGA (42.1% vs. 1.7%; p < 0.0001).
Conclusions and Comment
All in all, the authors point out that there are several important features to be aware of than the “classic“ peribulbar infiltrates. These include a catagen/telogen shift, melanin in fibrous tracts, and small dystrophic follicles. Much to my surprise, the authors did not report mast cell and eosinophil information in this study. We’ll come to the importance of that in just a moment. But all in all the authors feel that this information on melanin, catagen shift, dystrophic follicles is useful when we need to distinguish AA from PHL in specimens without peribulbar infiltrates.
MAST CELLS AND EOSINOPHILS IN AA: THE EVOLVING STORY
I’m a little disappointed that this study did not include mention of mast cells or eosinophils. It’s kind of like getting together with friends to talk about their visit to the summer state fair and none of your friends talk about the food that was available at the fair. There’s just some things that we expect in the story.
The role of mast cells and eosinophils in alopecia areata has been the subject of research for 40-50 years. I would like to highlight some key papers.
Elston et al 1997
In their 1997 report, Elston et al found eosinophils in 38 of 71 (53.5%) of biopsy specimens of alopecia areata (AA). The authors concluded that the presence of eosinophils in the fibrous tracts and near hair bulbs is a helpful diagnostic feature that distinguishes AA from other mimicking conditions such as androgenetic alopecia, trichotillomania and syphilitic alopecia.
In this Elston et al study, a peribulbar lymphoid infiltrate was present in 62 % of cases but absent in 27 of the 71 (38%) cases. But eosinophils were still present in 48% of cases where peribulbar lymphocytes were absent. Miniaturized hairs were present in 77% and melanin in fibrous tracts were present in 66%. 48 % had multiple catagen hairs.
This paper was important to understand how to diagnose non-classic AA biopsies that lack peribulbar infiltrates.
Darouti et al 2000
Darouti and colleagues were not as excited about eosinophils as Elston and colleagues. In a letter in JAAD in response to the 1997 Elston paper, Darouti et al showed that eosinophils were detectable in only 11 of 51 (21.6%) AA biopsies. The authors did not report the proportion of cases showing peribulbar inflammation. Instead the authors found a surprisingly high number of biopsies containing mast cells. Mast cells were detected within the fibrous tracts and around hair bulbs in 48 slides (94% of the cases). The authors felt that mast cells rather than eosinophils were a more important diagnostic finding.
Peckham et al, 2011
In 2011, Dr Elston and his team were back again looking at other features in alopecia areata biopsies besides peribulbar lymphocytes. Here, they examined 109 cases. In contrast to their 1997 study showing 62% of cases having a peribulbar infiltrate, here a peribulbar lymphocytic infiltrate was present in 84% of specimens. Eosinophils in fibrous tracts in 44%, lymphocytes in fibrous tracts in 94%, melanin within fibrous tracts in 84%, pigment casts within follicular canals in 44%, catagen follicles in 93%, and miniaturized follicles in 90%, Dystrophic miniaturized follicles were rare (4%). The authors concluded that the finding of eosinophils, melanin and lymphocytes in fibrous tracts are particularly helpful when a peribulbar lymphocytic infiltrate is lacking.
Bertolini et al, 2014
Bertolin and colleagues set out to explore the role of MCs in AA pathogenesis, focusing on MC interactions with CD8+ T-cells. Their data showed that perifollicular MCs are significantly increased in human AA lesions compared to healthy or non-lesional control skin. The authors further showed data to suggest that MC may present autoantigens to CD8+ T-cells and/or co-stimulatory signals. They suggested that MCs becomes skewed towards pro-inflammatory activities and this facilitates cross-talk with CD8+ T-cells in this disease. Together this may contribute to triggering HF-IP collapse in AA.
Nasiri et al, 2020
Nasiri et al set out to compare mast cell density in patients with alopecia areata, androgenetic alopecia and controls. There were 20 patients in each group. Significantly higher perifollicular and perivascular mast cell counts were seen in both AGA and AA groups as compared to the healthy control group (P<0.001 for both). AA patients had more frequent perivascular mast cells than the AGA group but it barely met statistical significance (P=0.042). Among patients aged <40 years, perifollicular and perivascular mast cell counts were not significantly different among three groups; however, subjects over 40 years of age in both groups had significantly more perifollicular and perivascular mast cells than healthy participants. There was a significant positive correlation between disease severity and mast cell counts in both perifollicular and perivascular areas in AA patients (P=0.001 for both).
Genedy et al, 2021
Authors set out to study the cellular infiltrate in AA at different disease stages and in relation to disease activity.
The authors reviewed biopsies from 40 subjects with AA. A significant relation was found between the course of AA and the terminal: vellus ratio. Peribulbar lymphocytic infiltration was seen in 70% of cases. Mast cells were observed in 87.5% of cases, including fibrous tract and around the arrector pili muscles. Eosinophils were detected in the scalp biopsy of 22.5% of cases. The authors showed that the course and activity of AA were significantly related to the peribulbar lymphocytic cell infiltration but not to mast cells and eosinophils.
The authors concluded that peribulbar lymphocytic infiltrate is the classical finding of AA, it is absent in the chronic phase. Mast cells are commonly found in the scalp biopsy of AA and proposed that this may explain why antihistamines help.
Final Summary
All in all, I liked this Plante et al study. It’s a nice reminder of the need to really fine tune skills to diagnose non classic AA. AA can be histologically confused for AGA, TTM and even syphilis too. I would have hoped there was a mention of eosinophils and mast cells.
As reviewed above, several studies over the years have examined the histological features of AA – especially those features other than the classic peribulbar infiltrates. As you can see, the data that has accumulated is a bit inconsistent. Some studies showing a large proportion of biopsies have eosinophils and some showing few.
All in all several features are important to differentiate AA from AGA and TTM.
Eosinophils in fibrous tracts may be helpful. The precise role for mast cells is not clear given how common they are in AGA.
The miniaturized hairs of alopecia areata may appear dystrophic or distorted when compared with the miniaturized hairs of AGA. Androgenic alopecia lacks pigment incontinence and lacks peribulbar lymphoid and lacks eosinophils in fibrous tracks.
TTM histology shows empty anagen follicles, multiple catagen hairs, and pigment casts in the follicular infundibulum. Eosinophils in fibrous tracts are not seen in TTM. Empty anagen follicles are not a feature of AA.
MAIN REFERENCE
Plante J et al. A comparative study of histopathologic features in alopecia areata and pattern hair loss.J Cutan Pathol. 2023 Jan 6.
ADDITIONAL REFERENCES
Bertolini M et al. Abnormal interactions between perifollicular mast cells and CD8+ T-cells may contribute to the pathogenesis of alopecia areata. PLoS One. 2014 May 15;9(5):e94260.
Darouti et al. Eosinophils in fibrous tracts and near hair bulbs: A helpful diagnostic feature of alopecia areata. J Am Acad Dermatol. 2000 Feb;42(2 Pt 1):305-7.Elston DM et al . Eosinophils in fibrous tracts and near hair bulbs: a helpful diagnostic feature of alopecia areata.J Am Acad Dermatol. 1997 Jul;37(1):101-6.
Genedy R et al. Lesson to Learn From Cellular infiltrate in Scalp Biopsy of Alopecia Areata.Am J Dermatopathol. 2021 Dec 1;43(12):e158-e164.
Nasiri et al. Infiltration of Mast Cells in Scalp Biopsies of Patients with Alopecia Areata or Androgenic Alopecia Versus Healthy Individuals: A Case Control Study. Galen Med J. 2020 Dec 29;9:e1962.
Peckham SJ et al. Histologic features of alopecia areata other than peribulbar lymphocytic infiltrates. J Am Acad Dermatol. 2011 Sep;65(3):615-620.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.