Adrenal Suppression: A Primer for the Hair Specialist
What is “adrenal suppression”?
Adrenal suppression is a condition characterized by the inability of the adrenal glands to produce adequate amounts of cortisol – a hormone which is critical during periods of physiological stress. Cortisol has many important roles in the body. It helps keep blood pressure up (at normal levels) and helps keep blood sugars up (at normal levels) and help the patient feel energized and awake. It’s easy to imagine that when the adrenal gland is not able to make enough cortisol, the patient is more likely to have low blood pressure, low blood pressure and feel very weak and fatigued.
Adrenal suppression is important to identify because patients with adrenal suppression need to be prescribed additional medications (so called “stress steroids”) dosing during times of illness or during times of surgery in order to mimic the body’s normal elevation in cortisol levels during physiological stress. The failure to prescribe additional stress steroids during times of stress or illness can lead to the patient with adrenal suppression to become quite ill.
Adrenal suppression has significant morbidity and mortality and so needs to be recognized and treated quickly and appropriately.
Why does “adrenal suppression” occur?
Exogenous corticosteroids taken by the patient inhibit the release of CRH and ACTH from the pituitary gland. This in turn reduces the amount of cortisol that the adrenal gland is instructed to manufacture. ACTH is an important hormone that tells the adrenal gland to make cortisol. With less ACTH, there is less cortisol produced.
What are the signs and symptoms of adrenal suppression?
The symptoms of adrenal suppression can be very non-specific. Therefore, it sometimes takes an astute clinician or patient or family member to question the possibility of adrenal suppression.
A patient with adrenal suppression may be completely asymptomatic. However the following symptoms may be seen
1. Weakness, fatigue
2. Malaise
3. Nausea, vomiting, diarrhea
4. Morning headaches
5. Abdominal pain
6. Muscle pain (myalgias)
7. Arthralgias
8. Psychiatric symptoms
9. In children, poor weight gain and poor growth can be seen.
What is an ‘adrenal crisis’?
An ‘adrenal crisis’ is a state whereby the body needs more cortisol than the adrenal glands can supply at that particular time. A patient with adrenal suppression is at risk to develop adrenal crisis during times of illness, fever, infection, surgery or trauma. Without additional cortisol prescribed to the patient, the patient with an adrenal crisis can become quite ill. An adrenal crisis is a medical emergency and needs immediate attention.
Low blood pressure and low blood sugars are often seen and seizures may also develop.
Patients with adrenal suppression may not have any problems until the time they have some kind of illness or experience some kind of body stress – such as an upper respiratory tract infection or gastrointestinal illness. That may be the first time they feel unwell and the first time they present for medical attention.
What factors increase the risk that a patient will develop adrenal suppression when using oral, inhaled, injectable or topical steroids?
Increased dose of steroids and longer duration of using steroids increase the risk that a patient will develop adrenal suppression.
How long after stopping or reducing steroids does it take for the adrenal glands to fully “wake up”?
It can take several weeks and in some cases it can take one year or more for the adrenal glands to function normally. Generally speaking, patients who have been on oral steroids for 4-6 weeks can usually expect any adrenal suppression to resolve in 2-8 weeks. Those patients who have been on steroids longer may have prolonged adrenal suppression and will need to be prescribed steroids to help them transition as the adrenal gland tries to manufacture steroids once again.
Who should be suspected or having adrenal suppression from use of steroids?
1. Children receiving more than 2 weeks of oral steroids and adults receiving more than 2-3 weeks.
2. Patients with multiple courses of oral steroid through the year even if less than 2 weeks each time.
3. Patients with symptoms of adrenal suppression such as weakness, fatigue, nausea, vomiting, diarrhea, abdominal pain, headaches, muscle pains, joint aches (arthralgias), psychiatric symptoms, low blood pressure, low blood sugars. Children with poor weight gain and poor growth should also be screened in addition to having any of the above symptoms and signs.
What blood tests are ordered for patients with suspected adrenal insufficiency from adrenal suppression?
The following blood tests are typically ordered to assess for glucocorticoid induced adrenal suppression (and glucocorticoid induced Cushing syndrome which often goes along with it)
1. Cholesterol
2. Fasting blood glucose (or random glucose)
3. Hemoglobin A1c
4. Sodium and potassium (high potassium and low sodium in primary adrenal insufficiency are due to combined glucocorticoid and mineralocorticoid deficiency. These are not seen in glucocorticoid adrenal suppression)
5. 8 am to 10 am “AM cortisol”
o A morning cortisol test is a useful first step by the primary care physician or the dermatologist
o The steroid dose may be withheld 24 hour before the dose is given
o If levels are less than 85 nmol/L it is quite likely that the patient has adrenal suppression. If levels are above 85 nmol/L, it’s still possible that the patient has adrenal suppression. In other words this cut off level of 85 nmol/L is not very sensitive. If a patient has a morning cortisol level above 85 and one really suspects that adrenal suppression is a possible diagnosis, one needs to do a cosyntropin stimulation test (see point 7 below)
o A morning cortisol above 250 nmol/L is not likely to be associated with adrenal suppression and a level above 350 nmol/L really suggests the adrenal axis is functioning normally again.
o A level between 100-275 nmol/L could represent adrenal suppression. Many patients with these AM cortisol values are often recommended to take stress dosing of steroids. Many are referred to an endocrinologist for proper cosyntropin testing
6. Endocrine tests (by the endocrinologist)
o An ACTH (cosyntropin) stimulation test by the endocrinologist can help determine if their truly is any adrenal suppression. ACTH is the key hormone to stimulate the adrenal gland to make cortisol. If one administers ACTH and finds the adrenal gland does not pump out cortisol, it’s a sign of ongoing adrenal suppression. The cosyntropin test involves administration of cosyntropin to the patient and then measurement of cortisol levels at 15 minutes and 30 minutes after injection (and initially). A level greater than 500 nmol/L is considered normal and a sign there is no adrenal suppression.
How is adrenal suppression treated?
Anyone with confirmed adrenal suppression needs to appreciate the potential seriousness of this situation. Patients with adrenal suppression can feel well and so may not fully understand that seriousness of their situation. Patients should ideally carry a medicalert bracelet to advise others of their adrenal suppression. All patients with adrenal suppression need to understand that if they feel unwell, or have fever from any reason, or develop an infection, or have high stress, or undergo surgery, or experience a trauma they will need to be prescribed ‘stress doses’ of steroids on an urgent basis. The patient needs to understand this may need to be administered in a hospital or acute care setting (although sometimes a patient may administer these stress doses themselves). This is essential and may be lifesaving.
To re-iterate again:
All patients with confirmed adrenal suppression should ideally consult with an endocrinologist as soon as possible. The endocrinologist can advise if daily doses of steroid are needed and how best to taper the steroids. The endocrinologist can advise how to take medications in the event of developing an illness, fever and advise on the needed steps in the case of deteriorating health. Anyone with a complex history or signs of adrenal crisis needs immediate attention.
One should seek medical attention immediately if unwell and ideally go to the emergency department. Emergency consultation with an endocrinologist is essential if there are any signs of adrenal crisis or fever or illness
1. During an adrenal crisis, hydrocortisone (SoluCortef) will be given by IV or intramuscular and repeated every 6 hours. An endocrinologist will guide how long this is to be done.
2. During surgery, hydrocortisone will be given by IV before the surgery starts and then every 6 hours after surgery. An endocrinologist will guide how long this is to be done.
3. During an illness or fever, hydrocortisone (or equivalent steroid) will be given at 20 mg/m2/day in a divided manner 2-3 times per day.
4. During times of vomiting, hydrocortisone (or equivalent steroid) will be given at 30 mg/m2/day in a divided manner 2-3 times per day
A MedicAlert bracelet should be worn by all patients with adrenal suppression.
Family members should be told about the adrenal suppression and be advised to help the patient seek medical attention if there are concerns in the patient’s health and to advise emergency medical teams about the diagnosis of adrenal suppression. The endocrinologist will likely provide helpful information about what steps to take in the event of semi-urgent and urgent situations.
Sometimes, patients will be taught how to inject hydrocortisone intramuscularly in the event of being far from a hospital centre (such as those patients who are traveling away from home, camping etc)
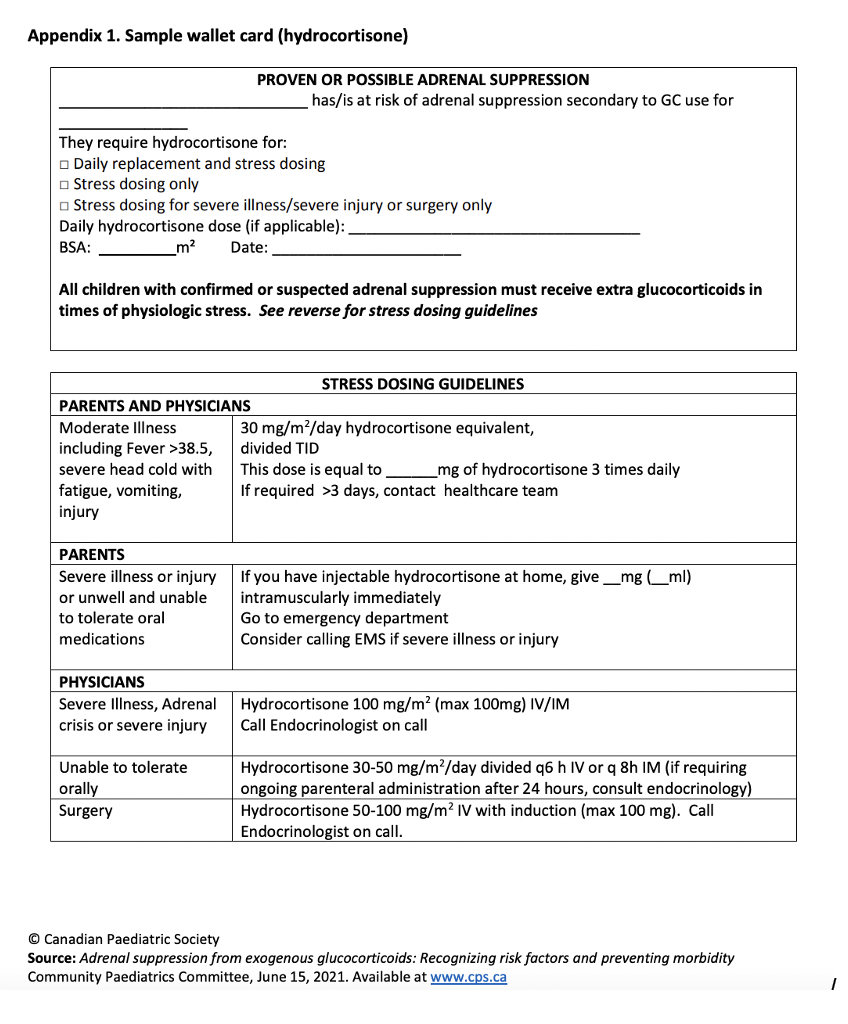
All patients with adrenal suppression should carry a medical information “wallet card” with them if instructed to do so by their endocrinologist. The Canadian Pediatric Society (CPS) has given an example of such card and it is shown on page 6 below.
Tapering Steroids in Patients on Steroids for Hair Loss
If patients have been on steroids for more than 3 weeks, it is important to taper steroids slowly rather than stop them abruptly. Such tapering is not generally needed if patients have been on them less than 3 weeks.
The speed of tapering depends somewhat on how long the patient has been on the steroid. A patient who has been on steroids more than 3 months should have a much slower and cautious taper than someone who has been on 6 weeks.
The first goal is to slowly get the patient down to what is considered a ‘physiological dose’ for them (5-7 mg prednisone for and adult and 1-5 mg for a child and adolescent). Tapering is typically done much more slowly once getting to this ‘physiological level’ and dosing can be done every other day rather than daily or with smaller decrements. For children, we may taper even more slowly. For example,
40 mg daily for 2 weeks
20 mg daily for 2 weeks
10 mg daily for 1 week
5 mg daily for 1 week
2.5 mg (one half of a pill) daily for 1 week & 1.25 (one quarter of a pill) daily for 2 weeks
An AM cortisol is generally checked 4 weeks after stopping steroids. An AM cortisol level above 250-300 suggest the adrenal gland is functioning well again.
What to do if a patient becomes ill or has stress while taking oral steroids and tapering oral steroids?
Patients who meet any of the following 10 criteria may need to be prescribed “stress doses” of steroids: 1) throat infection 2) ear infection) 3) nausea 4) vomiting 5) diarrhea 6) fever more than 38.5 C 7) lethargy/extreme fatigue 8) need stitches 9) have a broken bone or 10) need anesthetics of any kind…...
Here is how we typically prescribe stress steroids in this case:
a) If the patient is taking more than 10 mg prednisone at the time they become ill, he or she should take the medicine in divided doses. For example, if their dose is 30 mg daily, the patient should take 15 mg twice daily in the event they become ill.
b) If the patient is taking 10 mg prednisone at the time they become ill, he or she should take 5 mg twice daily.
c) If the patient is taking less than 10 mg prednisone at the time they become ill, he or she should take 5 mg twice daily.
d) If the patient has stopped prednisone at the time they become ill, but the patient has not yet gone to the lab to see if the adrenal gland is fully functioning again, he or she should immediately get back on 5 mg twice daily.
REFERENCE
Adrenal suppression from exogenous glucocorticoids: Recognizing risk factors and preventing morbidity Alexandra Ahmet, Anne Rowan-Legg, Larry Pancer; Canadian Paediatric Society, Canadian Pediatric Endocrine Group, Community Paediatrics Committee Paediatr Child Health 2021 26(4): 242–247
M. Cecilia Lansang, MD, MPH and Leighanne Kramer Hustak, DNP, BC-FNP, CDE. Glucocorticoid-induced diabetes and adrenal suppression: How to detect and manage them. Cleveland Clinic Journal of Medicine November 2011, 78 (11) 748-756; DOI:
‘WALLET CARD’ FOR PATIENTS WITH ADRENAL SUPPRESSION
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.