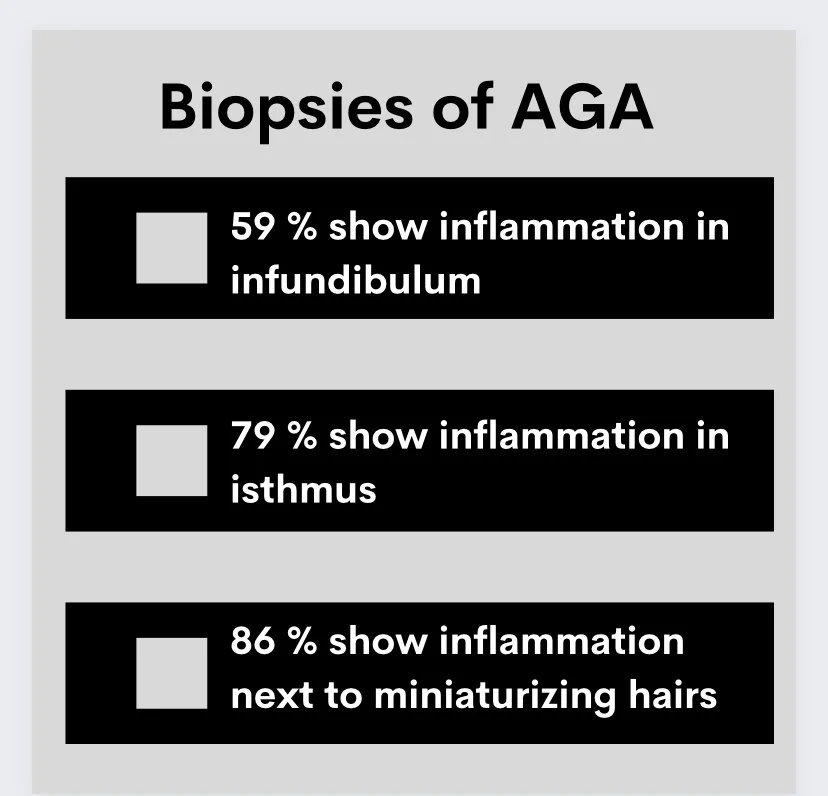
87.9 % of AGA biopsies have perifollicular inflammation; 79.3 % in isthmus region
Perifollicular Inflammation is Part of Androgenetic Alopecia
I was interested to read a report in the Journal of the American Academy of Dermatology about the patterns of inflammation in androgenetic alopecia.
It comes as a surprise to many the inflammation is so much a part of what biopsies of androgenetic alopecia look like. I’ve written about this topic quite a few times now
ARTICLE 1: Perifollicular inflammation in AGA
ARTICLE 2: AGA Under the Microscope
Inflammation is well known to occur in the isthmus and infundibulum of hair follicles. Inflammation is very much a part of AGA. The legendary dermatologist Dr David Whiting (1931-2018) first showed that 40% of biopsies from patients with AGA showed perifollicular inflammation. Ramos in 2016 showed that inflammation is more common around miniaturizing hairs. It has been postulated that the progressive fibrosis of the perifollicular sheath might begin with T-cell infiltration of follicular stem cell epithelium and that the perifollicular fibrosis actually impairs hair growth. In 2009, El-Domyati showed the perifollicular inflammation was present early in the condition long before perifollicular fibrosis started to be seen. Over time, as perifollicular fibrosis became more commonly seen as perifollicular inflammation started to decrease.
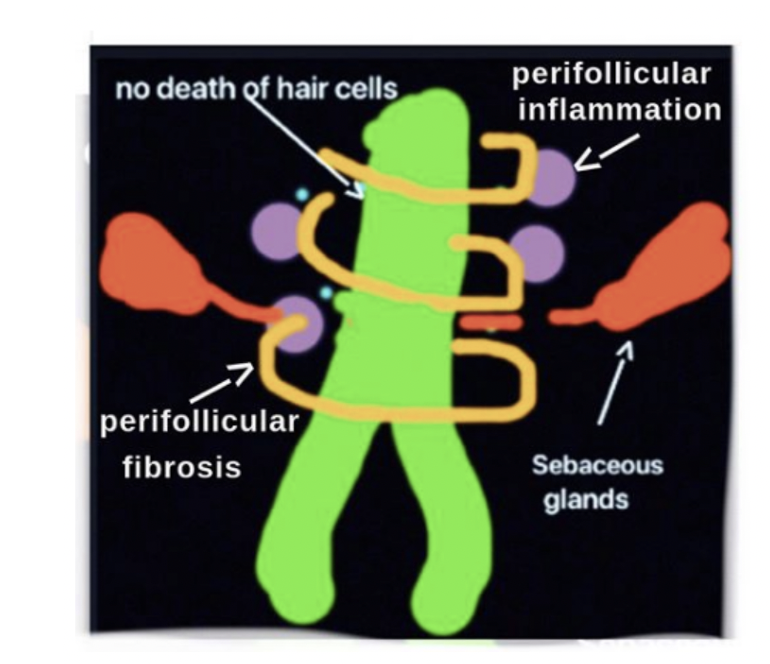
Cartoon showing key features of androgenetic alopecia: miniaturization of hairs (green), perifollicular fibrosis, perifollicular inflammation in the ismthus and lack of lichenoid inflammation and cell death and preservation of sebaceous glands
Plante et al, 2022
A new study examines patterns of inflammation in the hair follicle in androgenetic alopecia and compares those patterns to what is seen in alopecia areata.
Plante and colleagues performed a retrospective review of biopsies of androgenetic alopecia and alopecia areata over a 6 year period at their institution. There were 58 AGA and 38 AA biopsy samples.
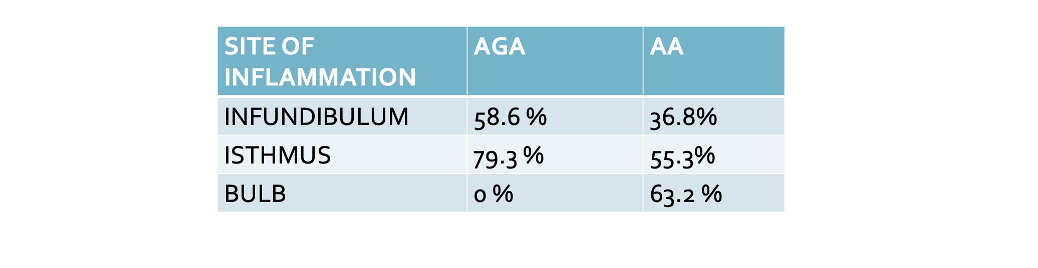
Perifollicular lymphocytic infiltrates were present in most specimens (87.9% AGA, 81.6% AA), with no significant difference in incidence.
(1) AGA specimens were more likely than alopecia specimens to exhibit inflammation in the infundibulum (58.6 % vs 36.8 %).
(2) AGA specimens were more likely than alopecia specimens to exhibit inflammation in the isthmus (79.3 % vs 55.3 %).
(3) Not surprisingly, biopsies from AGA were less likely to demonstrate peribulbar infiltrates (0.0% vs 63.2%).
Inflammatory infiltrates in the isthmus were moderate in 10 AGA (17.2%) and 5 AA (13.2%) samples and severe in 4 AGA (6.9%) and 1 AA (2.6 %) of samples.
Follicular miniaturization was present in many specimens, and inflammation adjacent to miniaturized follicles was observed in 86.2% of AGA cases and 78.9% of AA cases.
CONCLUSION
Most cases of AGA have perifollicular inflammation and most have inflammation at the level of the isthmus. One quarter of AGA biopsies have moderate to severe inflammation!
AGA is more likely than alopecia areata to have inflammation in the isthmus and infundibulum and these may be relevant to the pathogenesis of AGA. In fact, the authors showed the most miniaturizing hairs were surrounded by inflammation.
Inflammation probably drives the development of fibrosis and the process of miniaturization. Prior studies have shown the inflammation occurs before significant fibrosis develops. Prior studies have also shown an association between the extent of inflammation and the extent of miniaturization. So it seems that inflammation starts and drives fibrosis and miniaturization.
I liked this study because it really reminds us all to remember that AGA is an inflammatory non-scarring alopecia. Most biopsies have inflammation and one quarter even have moderate to severe inflammation.
If you look at a slide and see inflammation and perifollicular fibrosis, it’s easy for the inexperienced pathologist to get tricked into calling it scarring alopecia (like lichen planopilaris).
If interested see, article below for further discussion of this topic
ARTICLE 3: AGA or LPP: Who is right?
REFERENCES
Plante J. Perifollicular inflammation and follicular spongiosis in androgenetic alopecia. J Am Acad Dermatol 2022 Feb;86(2):437-438.
Ramos PM, Brianezi G, Martins AC, da Silva MG, Marques ME, Miot HA. Apoptosis in follicles of individuals with female pattern hair loss is associated with perifollicular microinflammation. Int J Cosmet Sci. 2016;38(6):651-654. https://doi.org/ 10.1111/ics.12341
Merlotto MR, Ramos PM, Miot HA. Pattern hair loss: assess- ment of microinflammation in miniaturized and terminal hair follicles through horizontal histologic sections. J Am Acad Dermatol. 2020;83(2):e145-e146. https://doi.org/10.1016/j. jaad.2020.03.119
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.