New Study Describes Varied Presentations and Disease Associations with Acne Keloidalis Nuchae
Acne Keloidalis Nuchae: New Study Highlights Complexity of Disease
Acne keloidalis is a chronic scarring alopecia characterized by the development of papules, nodules, plaques and/or tumorous masses – typically starting in the lower occipital area of the scalp. The cause is not clear although trauma to the scalp is thought to play a role including close shaving, friction, heat and humidity.
Authors of a new study set out to perform a retrospective and multicentre international review of 79 patients with a confirmed diagnosis of AKN. Patients were from Spain, Australia and Italy.
Patients Characteristics & Predisposing Factors
The study included 79 patients (75 men and 4 women) with a median age at diagnosis of 35 years were included. 42% were Caucasian, 8% middle eastern, 20 % African, 12 % African American, 14% south American and 5 % Asian.
In terms of predisposing factors, 38% had straight hair, 25% have wavy hair and 38% had curly hair. In terms of prior triggers, prior use of a razor to the back of the scalp was noted in 41% of patients. 17% previously used a helmet.
Disease associations
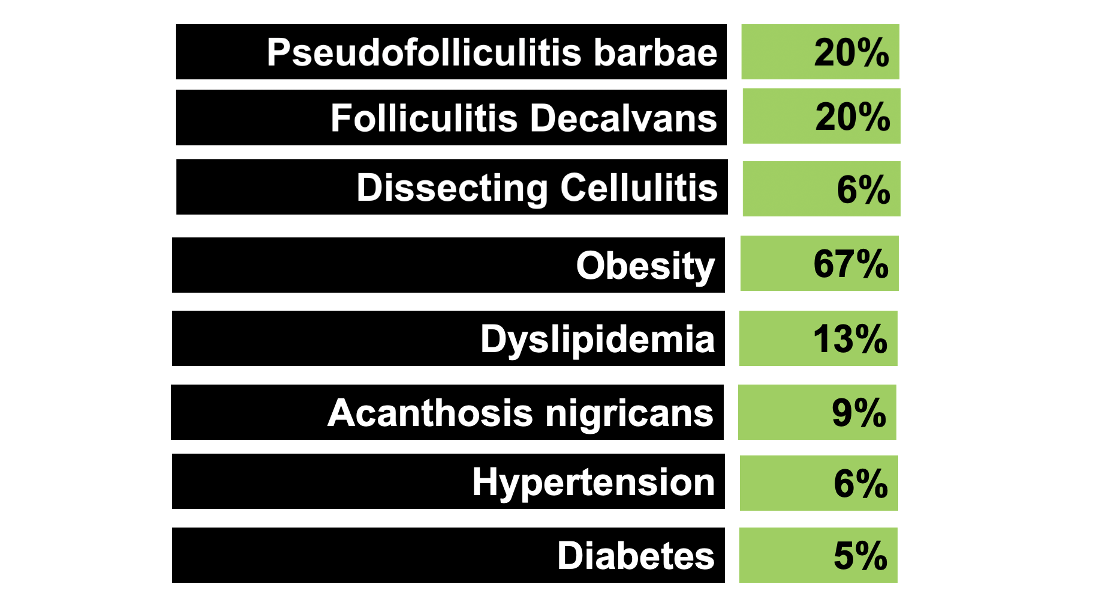
18% were obese, 6% had high blood pressure, 13 % had high cholesterol, 5% had diabetes, 9% had acanthosis nigricans. 12% had keloids in other areas of the body (with median number being 3). 20 % had pseudofolliculitis barbae, 12 % hidradenitis, 14% acne conglobate, 1 % pilonidal sinus, 6% dissecting cellulitis, 20 % folliculitis decalvans.
Severity
In terms of severity, 59% of patients had discrete papules and nodules, 18 % had merged papules and nodules, 12 % had plaques and 12 % tumerous mass. In terms of severity according to height of involvement in the occipital region (Umar classification). 41 % were less than 3 cm, 33 % were 3-6.5 cm, 26 % were more than 6.5 cm and none were widespread .
Straight hair was associated with less than 3 cm distribution of the lesions and wavy hair was associated with 3–6.5 cm distribution.
Treatments
The authors described an incredibly large array of treatments that were used in attempt to treat the AKN. Intralesional steroids was the most performed treatment modality followed by oral retinoids and oral and topical antibiotics.
19% of patients had no improvement with treatment but a high proportion of patients did have improvement. 26% had mild improvement, 18% had moderate improvement and 37% had significant or complete improvement.
Patients with a less than 3 cm distribution of the lesions or with discrete papules and nodules had a greater probability of important or complete improvement after treatment in comparison to the more than 6 cm distribution of the lesions group and the patients with merged papules and nodules.
Discussion
I liked this study as it draws attention to an scarring alopecia that is still very much a challenge to treat. Its exact pathogenesis is also not clear.
There are limitations to this study. These include lack of a control group and also the lack of matching the grade of improvement with the therapeutic modality.
But what I liked about this study is its focus on the complex disease associations that exist in AKN. It’s clear that features of the metabolic syndrome are very prevalent in AKN. In this study, a high proportion have overweight/obesity (66.7%) and dyslipidemia (13%), hypertension (6%) and diabetes (5%)
This study supports that general notion that metabolic syndrome is increased in AKN and this is therefore an important call to action for the patient.
A large study by Kridin et al in 2020 of 2677 patients with AKN and 13,190 controls also drew attention to the issue of metabolic syndrome. The prevalence of the MS was 3 times greater in patients with AKN than in control subjects (16.1% vs. 6.6). Obesity demonstrated the strongest association with AKN (OR 3.00; 95% CI 2.75-3.28), followed by type 2 diabetes mellitus (OR 2.47; 95% CI 2.20-2.77), hypertension (OR 1.82; 95% CI 1.63-2.05), and dyslipidemia (OR 1.60; 95% CI 1.46-1.75).
A 2017 study by East Innis et al found that the presence of any component disease of the metabolic syndrome (OR = 14, P = 0.008) and specifically hypertension (OR = 6.75, P = 0.036) were significantly associated with the extension of the lesions beyond the nape and occipital scalp.
Other follicular and scarring alopecias as common too. It’s well known that PFB is common in AKN and this study confirmed that 1 in 5 patients with AKN had PFB. But other scarring alopecias are common including folliculitis decalvans (20% and dissecting cellulitis (6%). So we should not be confused if we are diagnosing 2 conditions in our patients.
Components of the follicular occlusion tetrad (hidradenitis, acne conglobata, dissecting cellulitis, pilonidal cysts) are found in a significant proportion of AKN patients. Patients may not always tell us about these as they feel they are not related – so we must ask. These issues can be debilitating.
The study also reminds us that treatments are helpful for some patients with AKN. While It’s true that 1 in 5 patients had no improvement, nearly one third had complete improvement. This information is important as patients often ask me if it’s worth treating or not.
REFERENCE
Lobato-Berezo A et al. Acne keloidalis nuchae: An international multicentric review of 79 patients. J Eur Acad Dermatol Venereol. 2023 Nov 1.
Kridin K et al. Acne Keloidalis Nuchae and the Metabolic Syndrome: A Population-Based Study. Am J Clin Dermatol. 2020 Oct;21(5):733-739.
East-Innis ADC et al. Acne keloidalis nuchae: risk factors and associated disorders - a retrospective study. Int J Dermatol. 2017 Aug;56(8):828-832.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.