Rates of Depression and Anxiety Increased in Patients with AA
Depression and Anxiety Increased in Patients with AA
It is well known that alopecia areata has a profound impact on the mental health of those with the condition. Risks of depression and anxiety are known to be increased in those with AA.
A 2012 case-control study by Chu et al. showed a higher prevalence of anxiety and depression in people with AA than matched population controls.
A 2019 study by Vallerand et identified a bi-directional positive association between major depressive disorder and AA. In other words, there was an increased risk of depression in patients with AA and an increased risk of AA in those with depression.
Macbeth A et al. 2022
Authors form the UK set out to assess the risk of depression and anxiety in adults with AA compared to the general population. The researchers also wanted to evaluate the mental health treatment burden and impact on time-off work and unemployment.
The authors used a powerful database known as the Oxford-Royal College of General Practitioners (RCGP) Research and Surveillance Centre (RSC) network database. There were 5,435 people with newly-diagnosed AA in UK primary care were identified and these were matched to 21,740 controls. Mean age was 39 and 54 % were female. This was similar in cases and controls.
Pre-existing Depression And Anxiety in Patients with AA
The study showed that patients with AA were more likely to have a pre-existing diagnosis of depression and anxiety.
Overall, depression and anxiety were more prevalent in people diagnosed with AA compared to controls (p<0.001). In those with AA, the rates were: (Recurrent depressive disorder 12.3%, Depressive Episode 19.4%, Anxiety 16.6%) compared to matched controls (RDD 8.6%, DE 14.7%, AD 12.9%).
Mental Health in First Two Years After Diagnosis
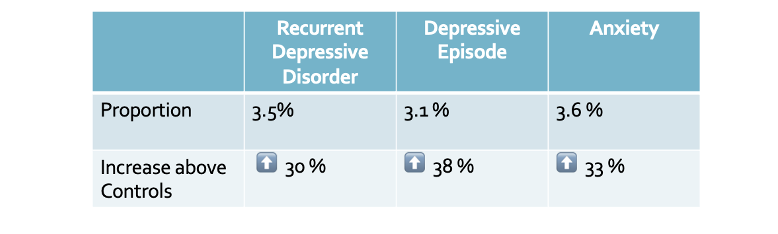
In the first two years after AA diagnosis, the authors showed that there was a 30-38 % increased risk of depression and anxiety. Specifically, the data was as follows:
a) Recurrent Depressive Disorder.
3.5% (95% CI 3.0, 4.1) of AA cases were diagnosed with new onset recurrent depressive disorder. This corresponds to an aHR 1.30 [95%CI 1.04-1.62].
b) Depressive Episode
3.1% (95% CI 2.5, 3.6) were diagnosed with depressive episode. This corresponds to an aHR of 1.38 [95%CI 1.13-1.69.
c) Anxiety Disorder
3.6% (95%CI 3.0, 4.2) were diagnosed with anxiety. This corresponds to an aHR of 1.33 [95%CI 1.09-1.63])
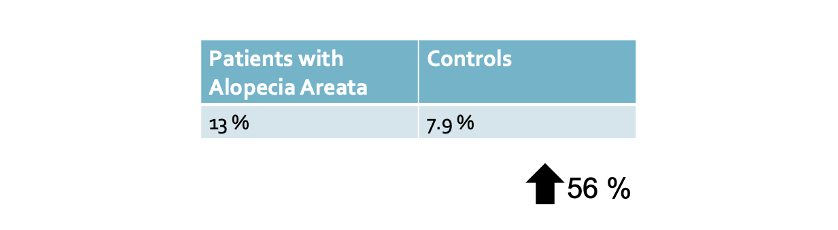
Time off work within One Year of Diagnosis in Patients with Alopecia Areata
Time-off work certificates were more frequently issued to people with AA (13.0% within a year of diagnosis) than matched controls (7.9%). This represented at 56 % increase with an aHR 1.56 (95%CI 1.43,1.71), p < 0.001.
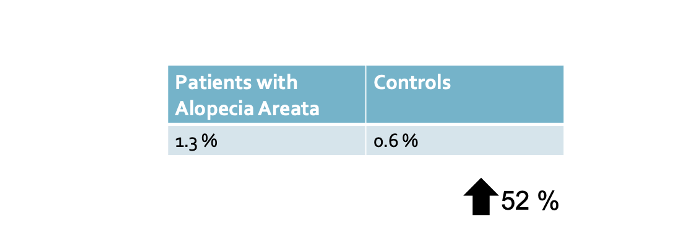
Unemployment within One Year of Diagnosis in Patients with Alopecia Areata
People with AA were more likely to have a record of unemployment in the year after diagnosis (1.3% of AA cases, 0.6% of matched controls. This represented an 82 % increased with an aHR 1.82 (95%CI 1.33, 2.49
Antidepressant Prescribing
Higher rates of antidepressant prescribing were also seen in people with AA. overall less than 10 % of those with a mental health condition were referred for non pharmacological management.
Conclusion
The overall conclusion was that people with AA have higher rates of depression and anxiety than those without AA.
The authors showed that there is a higher rate of depression and anxiety before onset of AA and a higher rate once alopecia areata develops. The authors proposed that this data supports the general notion that the risks of alopecia areata are increased in those with depression and anxiety and that depression and anxiety are increased in those with alopecia areata. We call this the ‘bidirectional association.”
These mental health issues were shown to impact in negative ways on mental health treatment burden, time-off work, and unemployment.
The authors proposed that evidence-based mental health treatment programs are needed for people with AA.
Further Questions For Study in the Future
There are many unanswered questions that will fuel further research:
1) Does treatment of alopecia areata reduce incidence of depression and anxiety?
2) Is pharmacological approaches better or worse than non pharmacological approaches or are both the ideal?
3) which groups of patients with AA benefit most from non pharmacological and pharmacological approaches?
4) Do any medications worsen depression and anxiety in AA?
5) What are the barriers for mental health professionals to recognize the burden of AA?
REFERENCE
Macbeth A et al. The associated burden of mental health conditions in alopecia areata: A population-based study in UK primary care. Br J Dermatol . 2022 Feb 14.
Chu SY et al. Psychiatric comorbidities in patients with alopecia areata in Taiwan: a case-control study. Br J Dermatol. 2012 Mar;166(3):525-31.
Vallerand IA et al. Assessment of a Bidirectional Association Between Major Depressive Disorder and Alopecia Areata. JAMA Dermatol. 2019 Apr 1;155(4):475-479.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.