Behçet’s Disease: A Brief Primer For the Hair Practitioner
Behçet disease (BD): A Rare But Important Disease for the Hair Loss Practitioner to Know About
Introduction
Behcet’s disease is not a disease we talk about often in the world of hair medicine. However, it’s important for hair loss practitioners to be aware of this condition. The condition itself, does not typically cause hair loss. However, the medications used to treat Behcet’s very rarely cause hair loss. Patients with Behcet’s disease have ulcers in the mouth or genital ulcers quite commonly but also sometimes have a phenomenon known as “pathergy.” This means that trauma can induce skin lesions. Therefore, hair transplantation, microneedling, PRP procedures, laser hair removal are usually not going to be very good options for the patient with Behçet disease (BD). We discussed an interesting case of pathergy developing after laser hair removal several years ago. (To review this, please click on the link below)
Introduction
Behçet disease (BD) is an inflammatory vasculopathy that can affect multiple organ systems in the body. It is a variable vessel vasculitis and can affect both veins and arteries of all sizes (sometimes leading to thrombosis).
The syndrome was was characterized by Turkish dermatologist Hulusi Behçet in 1937. He recognized a triad of symptoms in his patients – namely recurrent aphthous stomatitis, relapsing uveitis, and genital ulceration. The disease frequently starts in second and third decades of a person’s life and has a remitting–relapsing course.
How common is Behçet’s Disease?
Behçet’s disease is not common. However, some parts of the world have many more patients with BD than other parts of the world. Prevalence ranges from 5 per 100,000 people in North America to 80 per 100,000 in Iran to up to 420 per 100,000 people in Turkey. In general, Turkey has the highest prevalence of BD, followed by Iran, Saudi Arabia, Iraq, Israel, northern China, and Korea. The disease is more prevalent in countries around the Mediterranean basin and East Asia such as Japan, Korea and China (the so called ‘ancient silk road’).
What are the symptoms of Behçet’s Disease?
It is important to recognize that Behcet’s can appear very different in different people. Some patients can have a more eye symptoms related Behcet’s (occular Behcet’s), some can have an intestinal Behcet’s and others can have a nervous system predominant form (neuro Behcet’s).
The most common symptoms, however, are oral ulcers, followed by genital ulcers, skin lesions (like papulopustular lesions or erythema nodosum or pseudofolliculitis), uveitis and arthritis. However, a range of systemic manifestations can occur including neurological issues, gastrointestinal issues and a range of vascular issues.
Oral ulcers occur in up to 97-99% of patients, genital ulcers in up to 85% of patients, skin lesions in up to 85 %. About 50% of patients have uveitis and a similar proportion have arthritis.
Symptoms of Behçet’s differ in different parts of the world. In North America, more women than men are affected, In the silk road countries, more men than women are affected. In North America, pathergy affects 30 % and a greater proportion of patient have milder disease. In silk road countries, pathergy is found in 50 % or more of patients and many have a more severe disease with greater likelihood of systemic involvement.
What is the cause of Behçet’s disease?
The cause of Behcet’s is unknown although there appears to be genetic an environmental factors that contribute. There is a strong correlation with human leukocyte antigens, specifically HLA-B51, especially in patients living in the prior silk road zones. HLA-B51 positivity appears somewhat less common in North America.
Pathergy: What does the term mean?
Pathergy refers to the development of a papulopustular skin lesion at the site of trauma. Overall, it is seen in 50% of patients with Bechet’s disease but the chances of a patient having a positive test depends on where in the world they live and their genetic background. For example, this ranges from 9 % in India to 71 % in China.
Pathergy is a different term than the Koebner phenomenon - although both are seen after injury. In pathergy, there is infiltration of mononuclear cells at the site of trauma and a red bump or pustule forms. In the Koebner phenomenon, trauma induces a specific disease and what is seen at the site of the trauma is a specific disease not necessarily a pustules. For example, trauma might induced lichen planus, psoriasis, or vitiligo in a patient with these conditions.
Testing for Pathergy
One can test for pathergy using a 20 gauge needle. This is entered into the skin at a 30 degree angle (generally on the forearm). 5-6 areas of the skin are poked and then left for observation over the next 24-48 hours. A positive result is defined a presence of an erythematous papule ≥2 mm or a pustule after 24–48 hours.
Positive pathergy result: A 20 gauge needle is used to introduce trauma to the skin. the area is then observed for 24-48 hours to see if a pustule forms
Positive pathergy results happen in several conditions – and not exclusively in Behçet’s disease.
Pathergy can also be seen Sweet’s syndrome, Crohn’s disease, pyoderma gangrenosum, A20 haploinsufficiency, and a few others (inflammatory bowel disease, eosinophilic pustular folliculitis, chronic myeloid leukemia treated with IFN-alpha, and spondyloarthropathies).
Why does pathergy occur?
It’s not clear why pathergy occurs. There appears to be damage to keratinoctyes due to trauma or a microbe that triggers inflammation. There is a release of pro-inflammatory cytokines (IL-6, TNF-alpha, IL1B) that leads to inflammation. This reaction may occur in other organ systems other than the skin (for example eye inflammation after eye surgery or synovitis after arthrocentesis, for example).
Pathergy is not always present in a given patient. It has a relapsing remitting course. In addition, the overall incidence may be decreasing in the past decade. Despite these limitations, testing for pathergy remains an important part of evaluating Behcet’s disease (see criteria below).
How does one diagnose Behçet’s disease?
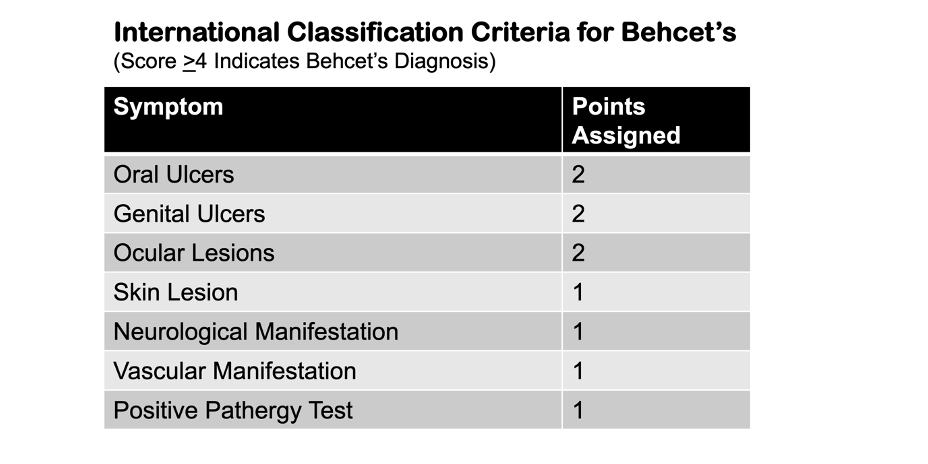
There are no pathognomonic lab tests to diagnose BD. However, over the years, researchers have put forth clinical criteria. These criteria have changed over time. The International Criteria for Behçet Disease (ICBD) developed from the collaboration of experts from 27 countries to address the challenges in diagnosing Behçet’s disease.
The ICBD criteria are highly sensitive and specific. However, there are still differences in clinical manifestations of the disease among ethnicities and countries. A score of 4 or more indicates a diagnosis of Behçet’s disease.
Treatment of Behcet’s Disease
Behcet’s is treated with a variety of immunosuppressants. The exact treatment will depend on what organ exactly is involved. Treatments include oral steroids, azathioprine, colchicine, TNF inhibitors, cyclosporine, methotrexate, sulfasalzine. Apremilast has recently been shown to be helpful for treating oral ulcers in Behcet’s
References
Alibaz-Oner F and Direskeneli H. Advances in the Treatment of Behcet’s Disease. Curr Rheumatol Rep. 2021; 23(6): 47.
Hatemi G, Melikoglu M, Tunc R, Korkmaz C, Turgut Ozturk B, Mat C, Merkel PA, Calamia KT, Liu Z, Pineda L, Stevens RM, Yazici H, Yazici Y. Apremilast for Behçet’s syndrome--a phase 2, placebo-controlled study. N Engl J Med. 2015;372(16):1510–1518. doi: 10.1056/NEJMoa1408684.
Sakane T, Takeno M, Suzuki N et al.. Behçet's disease. N Engl J Med 1999;341:1284–91. 10.1056/NEJM199910213411707
Yurdakul S, Hamuryudan V, Yazici H. Behçet syndrome. Curr Opin Rheumatol 2004;16:38–42. 10.1097/00002281-200401000-00008
Yazici H, Fresko I, Yurdakul S. Behçet's syndrome: disease manifestations, management, and advances in treatment. Nat Clin Pract Rheumatol 2007;3:148–55. 10.1038/ncprheum0436
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.