Contraindications to Hair Transplantation: When is hair transplant surgery not an option?
Hair Transplantation Contraindications and Cautions.
Hair transplantation is quite successful nowadays in the properly chosen candidate. Every year, 300,000 to 350,000 hair transplants are performed worldwide. Statistics about patient satisfaction are not widely published, but in general about 92-94 % of patients appear satisfied with their procedures. This data comes from websites such as Realself.com and RealPatientRatings.com and are surprisingly quite consistent.
What about the 6-8 % who are not satisfied with the results they get? What do we know about the 18,000-20,000 patients each year around the world who don’t quite get the result they had envisioned in their minds before they set out to have the procedure.
Here, we’ll look at a variety of factors that are relevant to hair transplantation outcomes. We’ll look at pre-transplant patient select factors and several criteria that should be considered before allowing a patient to proceed to transplant. Second, we’ll look at reasons why some patients have poorer outcomes than they were hoping for.
A. “PRE-OP” FACTORS: WHO SHOULD BE TURNED AWAY AND TOLD NOT TO HAVE A TRANSPLANT?
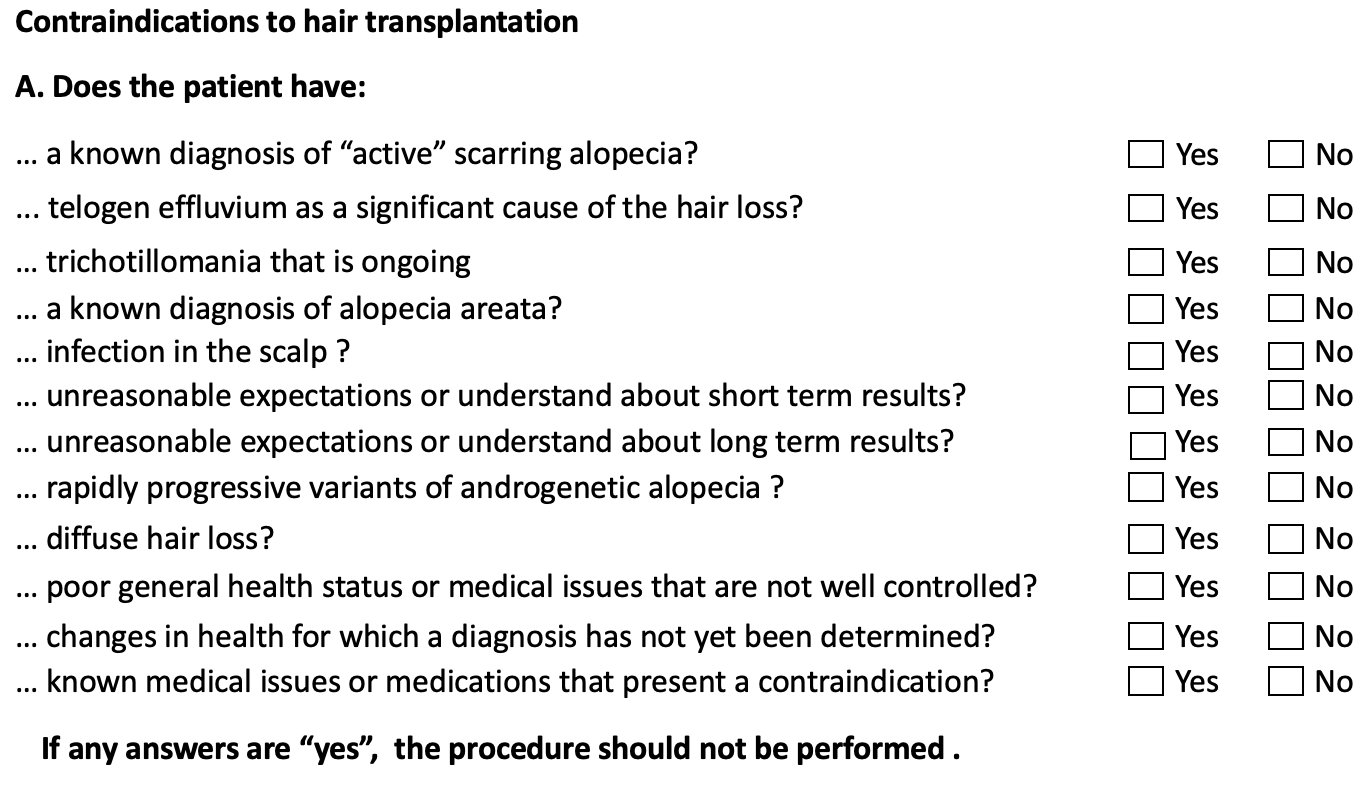
The reasons that a hair transplant surgeon should not do a hair transplant are generally quite obvious. These are reviewed in part A below. The reasons that a hair transplant surgeon should hit the pause button and investigate further before deeming the patient a good candidate for surgery are discussed in part B. These reasons are less obvious and one of the more common reasons for poor outcomes in hair transplant surgery. I will get to that in a moment, but first let’s discuss the classic contraindications to hair transplantation.
Part 1: The Contraindications to Hair Transplantation
When we use the term contraindication, I am referring to all the various reasons that make a patient a poor candidate for hair transplant surgery. These are the reasons for which a patient wanting surgery should be told he or she can not have surgery. These are the reasons that a surgery should be cancelled. The reason is quite simple: performing surgery in a patient with a contraindication to surgery may lead to poor growth and suboptimal results and in some cases may flare an underlying hair disease and lead to even worse density that before the patent went into surgery.
There are several conditions that should not be transplanted. These include active scarring alopecia, telogen effluvium, active trichotillomania, alopecia areata, and diffuse androgenetic alopecia (diffuse unpatterned alopecia areata). Hair transplants performed in patients with these issues do not work well.
Some patients also are not candidates for surgery because of their expectations. Some patients expect their density to return back to the same thickness it once was before the hair loss started. Rarely is this achieved (although in some situations, modern hair transplant techniques can make it ‘look’ pretty close to the high density it once was). Some patients only want a single surgery and don’t every want to come back to the surgeon’s office again. While this may be a reality for a patient with stable hair loss, many patients have years and years of hair thinning ahead of them and may need further surgeries in the future in order to maintain high density (maintain the same “look” over many years).
Finally some patients are just not healthy enough for surgery. A patient with uncontrolled high blood pressure is not a candidate. These patients can spike their blood pressure even higher during surgery and are at risk for bleeding. A patient with a bleeding disorder may also not be a candidate unless the bleeding disorder can be corrected during and after the surgery.
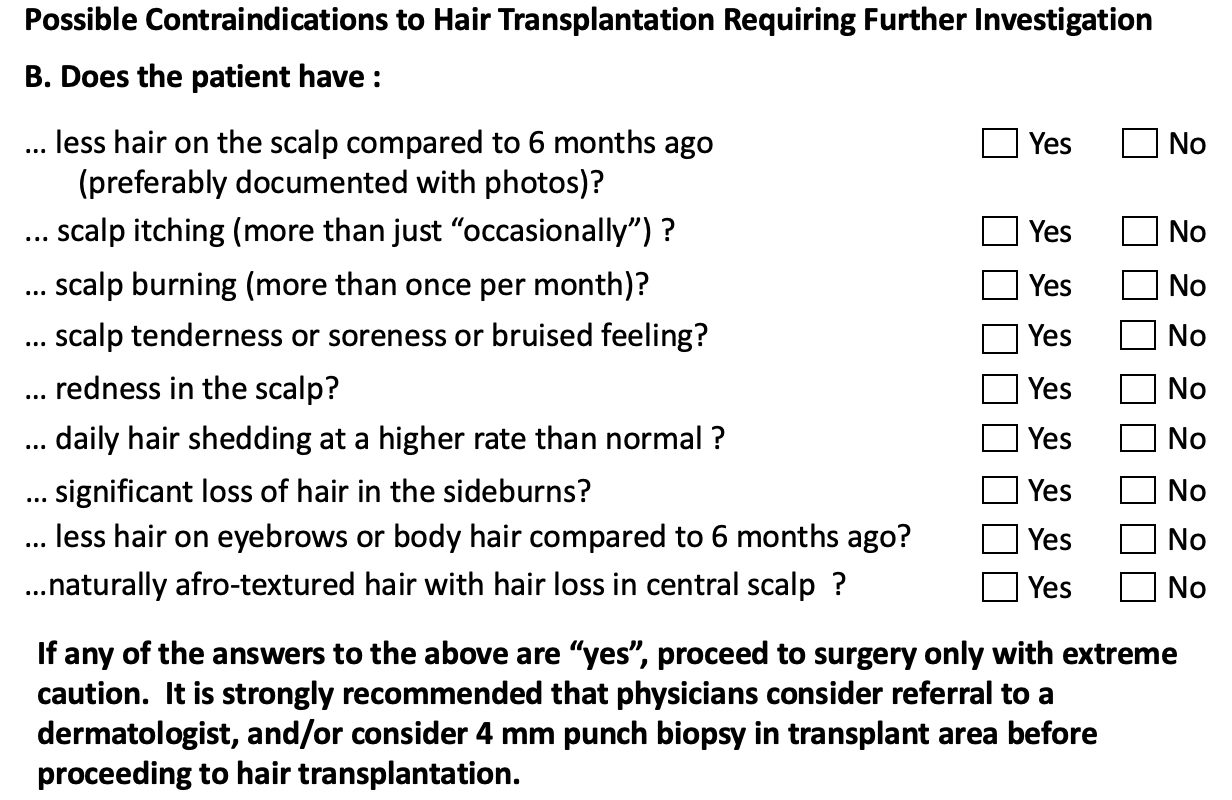
Part 2: Potential Contraindications to Hair Transplant Surgery
The next part is a discussion of a topic that is incredibly important but less often spoken about or written about in the hair transplant field. There are a series of 9 questions that can be asked of patients that can help identify patients who might have a scalp issues that presents a contraindication to hair transplantation. Some of these issues may not even be obvious when the scalp is examined.
The speed of hair loss is very important to ascertain. The ideal candidate for hair transplant surgery is a patient with relatively stable hair density. If the density is changing one week to the next, it would be obvious to many that that particular patient is not a good candidate. Even a density that changes month to month is concerning. So clearly there is some cut off for the speed of hair loss that changes a patient from ‘obviously concerning’ to ‘less concerning.’ In my opinion that cut off is 6 months: A patient who is losing hair visibly in 6 month intervals should be further evaluated. This speed of loss can certainly occur in some patients with androgenetic alopecia but it is not the typical speed.
Most patients with hair loss have itching from time to time. Patients with frequent itching, especially moderate or severe itching should be throughly evaluated to rule out an underlying scalp disorders. Most of the times the cause is seborrheic dermatitis or psoriasis, which is itself not a contraindication to surgery. However, some cases of lichen planopilaris can mimic seborrheic dermatitis almost perfectly so one must always be thinking of this possibility if a patient has daily itching of moderate to severe intensity. Patients with scalp burning and scalp tenderness should invoke greater concern than itching as these symptoms are less common in typical seborrheic dermatitis or psoriasis. Patients with scalp burning and scalp tenderness should be evaluated by a dermatologist and strongly consideration should be given to having a scalp biopsy. Even if the diagnosis turns out to be a non scarring condition, patients with scalp burning may find their burning worsens with surgery. Extreme caution must be given before proceeding to surgery.
Increased scalp redness is an important “red flag.” There is of course a gradient of scalp redness ranging from slightly red, to intense cherry red. The latter is more concerning than the former but both may be concerning. As the degree of redness in the scalp increases so should the likelihood that a scalp biopsy be performed. Most faintly red scalps will still end up being candidates for surgery after the biopsy results comes back; few cherry red scalp will be candidates for surgery after the biopsy comes back.
Increased amounts of daily hair shedding is important for the physician to appreciate. The actual number does not matter and too many physicians and patients focus on whether the number is greater than 100 or less than 100. The reality is that if a patient feels they are shedding a lot more than they once were, a detailed evaluation should be considered before proceeding to surgery. For many women, it might be that the increased shedding is still a part of the androgenetic alopecia. However, a patient with AGA who is shedding so intensively should ideally be stabilized with non surgical treatment before proceeding to surgery. Many patients with increased shedding will also have telogen effluvium. Blood tests for iron, thyroid, hemoglobin and possibly other tests are mandatory for any patient with shedding. Some patient with shedding will have lichen planopilaris as well as other scarring alopecias and some will have alopecia areata. Shedding must never be ignored.
Finally, there are a number of simple questions that can help identify the most subtle cases of frontal fibrosing alopecia and the most subtle cases of central centrifugal cicatricial alopecia (CCCA). Frontal fibrosing alopecia (FFA) is increasingly common and easily missed in the early stages. Women 40-60 years with recent loss of eyebrow density and/or body hair and women with loss of sideburn hair on both sides must be considered to have FFA until a full work up is done. Of course, not all will have FFA, but this simple rule has helped many surgeons pause surgery on a patient that they otherwise would have missed.
Finally, all female patients with afrotextured hair who are considering hair transplantation in the central scalp should have a biopsy before proceeding to surgery in order to rule out central centrifugal cicatricial alopecia. It’s a simple rule but the frequency with which CCCA will be identified is incredibly high. In my opinion, no woman with afro-textured hair should have surgery in the central scalp or crown with out first having a biopsy.
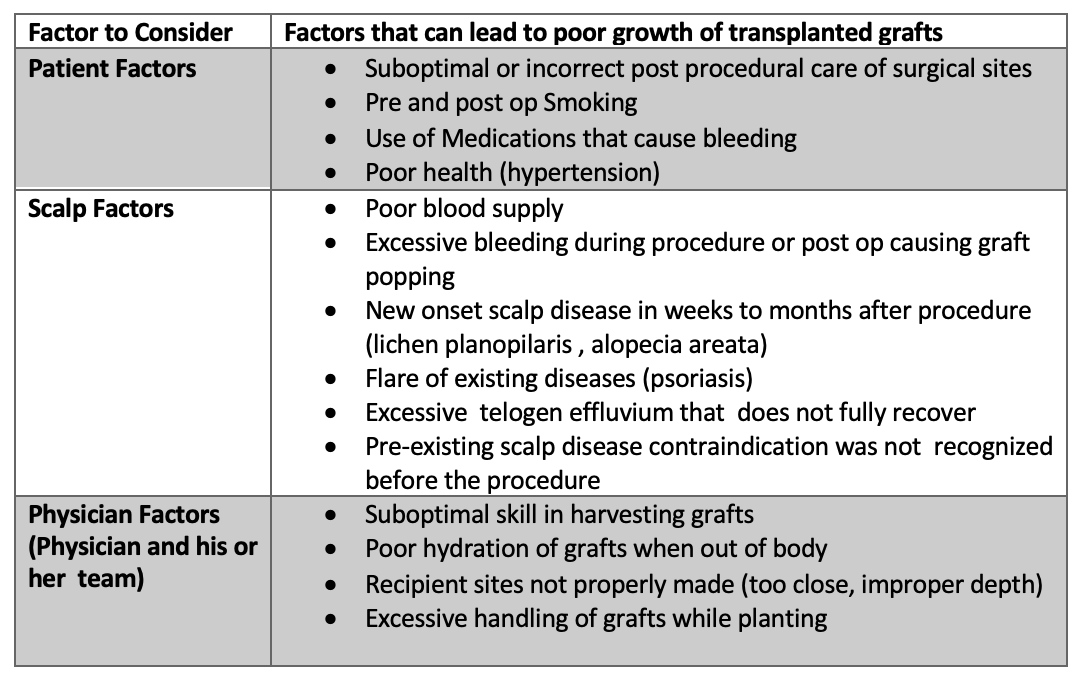
B. POST OP FACTORS: WHY DO SOME PATIENTS NOT OBTAIN THE RESULTS THEY WERE HOPING FOR ?
There are several reasons why patients don't get the results they though they would have. These can be divided into patient related reasons for poor growth, scalp related reasons for poor growth and physician related reasons. These are summarized in the table below.
a) Patient factors.
Certain things a patient might do or not do after a transplant could lead to suboptimal outcomes. A patient who mistakingly scrubs his head in the shower on day 2 or wakes up in the middle of the night to scratch the entire head is going to lose grafts. The result 9 months later will be poorer outcomes. Other factors like smoking are known to be associated with poorer graft survival. A patient with poor health, such as a patient with poorly controlled hypertension might experience an increased chance of post operative bleeding and a greater chance of experiencing graft 'popping.’
b) Scalp factors
In some cases, the health of the scalp does not permit good growth of transplanted hairs. Some scalp bleed post operatively a great deal and this causes graft popping and the dislodgement of many grafts. Some scalps, such as in the case of a hair transplant performed in a patient with inactive scarring alopecia, might not bleed enough both during and after the transplant. This is a reflection of poor blood supply and a higher likelihood of poor growth. The development of a new scarring alopecia such as lichen planopilaris post operatively may impact the survival of the grafts. Even a significant flare in a patient’s underlying psoriasis will impact the growth of the scalp hair.
c) Physician factors.
In some cases, the way the physician and/or his team performed various parts of the procedure lead to a reduced chance of the transplanted hairs surviving. In fact, there are many steps in a hair transplant procedure whereby a poorly executed step can compromise results. This includes errors in the way grafts were harvested from the donor area, and errors in how grafts are stored while out of the body and errors in how the grafts are put back into the scalp.
Summary and Conclusion
Not every patient who wants a hair transplant can have a hair transplant. Not all patients who have a hair transplant have a successful outcome. Fortunately, most do and hair transplantation remains on of the most consistently effective treatments for some hair loss conditions like androgenetic alopecia.
It is incredibly difficult sometimes for physicians to identify patients who have rare scalp disorders that should not be transplanted. There are many subtle cases of lichen planopilaris and subtle cases of frontal fibrosing alopecia or alopecia areata that are easily missed. A patient with these conditions who undergoes a hair transplant may not have a good outcome.
This article has outlined both the well known contraindications to hair transplantation as well as some of the so called “red flags” that should prompt physicians to pause and more carefully evaluate whether the patient in front of them may in fact have a hair and scalp disorder that was not previously considered.
I encourage the hair transplant physicians I train to download the following information sheet and complete it for every patient they see. Check off the boxes and put it in the patient’s chary for every patient. Many hair transplant physicians have shared with me over the last few years that the number of referrals they are making to dermatologists and the number of biopsies that are being done has now gone up considerably. Some of these biopsies are returning with diagnosis of primary scarring alopecia.
There are many reasons why 6-8 % of patients who undergo hair transpants have results they are not happy with. If we can reduce this number slightly be ensuring that no patient with a contraindicated scalp disease proceeds to surgery, we will have done something quite good for everyone.
Download Hair Transplant Contraindication and Red Flag Reminder Sheet
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.