COVID 19 Vaccination for Patients with Autoimmune Hair Loss
COVID 19 Vaccination in The Setting of Autoimmune Hair Loss: Exact Risks Still Waiting to be Defined
Autoimmune hair includes conditions such as alopecia areata, lichen planopilaris, frontal fibrosing alopecia, discoid lupus, and others. The most common question of the past few weeks has been “Do you recommend that I get the new COVID 19 vaccine?”
At the time of this article (Jan 13 2021), we now have two COVID 19 vaccines approved for use in Canada. These are mRNA vaccines and made by Pfizer (approved for those over 16) and Moderna (approved over 18 years), respectively. Other types of vaccines are likely on the way later in 2021 including adenoviral vaccines and protein vaccines.
The current mRNA vaccines were approximately 95 % effective in preventing COVID 19 based on comparison of rates of COVID 19 development in subjects receiving the vaccine vs those receiving the placebo. Benefits were similar in many different groups - younger vs older, men vs women, etc.
Side effects of the vaccine included issues such as pain at the injection site, headaches and fatigue. The overall incidence of “serious” side effects was fortunately quite low and overall the frequency of serious side effects was similar in placebo and treatment groups in clinical trials.
For now, we have tens of thousands of patents that have been formally studied in clinical trials. In the Pfizer trial, there were 43, 548 participants were randomized to placebo or the real vaccines. There were 8 cases of COVID 19 in those who received the COVID 19 vaccines and 162 cases in those who were assigned to placebo. The Moderna trial enrolled more than 30, 000 US participants, including 7000 aged over 65 and 5000 under 65 with high risk chronic diseases. There were 90 COVID 19 cases observed in the placebo group and five were reported in the vaccine group.
Conclusions about vaccine side effects are based on small numbers of clinical trial participants and numbers grow larger now as real world patients get followed for side effects. We don’t have hundreds of millions of patients who have received these vaccines yet. The CDC recently released data from the first 1.8 million people receiving the vaccine. The CDC indicated that safety has been good overall although there hs been 21 cases of anaphylaxis among the 1.8 million vaccinated. As the numbers grow to many millions, we will have a clearer sense of the exact magnitude of risk. However, the safety data from these two trials and the CDC monitoring data is quite impressive so far. Of course long term follow up is valuable too. There was nothing in these trials that would preclude the vast majority of people in the population from getting it. There were a small number of cases of anaphylaxis is those who had prior serious allergies. There were a small number of cases of Bell’s palsy (4 cases out of 20,000 subjects receiving the vaccine).
What do we know about vaccination for patients with autoimmune diseases?
The US Center for Disease Control CDC has made it clear that provided a person does not have allergies to an ingredient in the vaccine, it’s reasonable for patients with autoimmune disease to consider vaccination and speak further with their own doctors. Patients should be aware we don’t have any good data yet on exact risks in those with autoimmune disease but it’s likely very small compared to the massive benefits that come from reducing the risk of getting COVID and the consequences that come from having COVID (illness, death, long term disability). The Canadian guidelines make it clear: patents with autoimmune diseases should strongly consider getting vaccinated but need to be aware that good studies have yet to be formally done.
Studies are needed pertaining to vaccine related efficacy and safety for patients with autoimmune diseases. Some patients with autoimmune diseases don’t mount quite as good of protective antibodies responses to vaccines as patients who do not have immune diseases. How this relates to patients with autoimmune hair loss conditions who receive COVID 19 vaccines is not known. Likely it is a minor issue (or not an issue at all) for most types of autoimmune diseases.
Patients who are immunosuppressed who get COVID infection often have lower protective antibody titers in the bloodstream. So there is a theoretical concern that patients with autoimmune diseases who are using immunosuppressive medications may react less well to COVID 19 vaccines - although this concern applies the most to those using certain types of medications such as methotrexate and rituximab. We know from past studies that patients using the immunosuppressive drug methotrexate respond less well to some vaccines like pneumococal vaccines. Patients using methotrexate mount less antibody titers after getting the vaccine. There may be some diminishment of responses with drugs like JAK inhibitors and TNF inhibitors but it’s felt to be a whole lot less of an issue. For patients with autoimmune hair loss, it’s likely that rituxumab is the most important drug whereby a theoretical potential exists for reduced COVID vaccination responses. There is portably little risk with methotrexate but this is being studied. For now, it’s recommended that patients using immunosuppressive medications (except rituxumab) proceed with vaccination when their turn comes up provided there are no contraindications.
It’s important to understand that patients in the Pfizer and Moderna trials were not immunosuppressed patients so data is not known yet about how immunosuppressed patients respond to these vaccines. However, the trials did include older age patients (who we know have reduced immune systems), and vaccine responses were still very good in these patients. It’s likely that immunosuppressed patients will still respond to some degree after getting the vaccines.
Is there a problem with vaccination with the different drugs that patients with autoimmune hair loss conditions use ?
We have discussed the concerns about methotrexate above. Methotrexate is sometimes used in treating autoimmune hair loss conditions like alopecia areata and sometimes lichen planopilaris and frontal fibrosing alopecia and discoid lupus. For those hair loss patients using methotrexate, a discussion needs to be had with each patient about whether or not to hold the dose for a few weeks or not. Topical steroids and topical calcineurinn inhibitors won’t likely affect vaccine responses so that won’t be an issue for most. These topical drugs won’t typically need to be held for most patients before vaccination. Of course, each person should review this issue with their own doctors. Oral hydroxychloroquine (Plaquenil) and doxycycline won’t have much of an issue ether. JAK inhibitors like tofacitinib or Ruxolitinib could theoretically affect vaccination responses to a very minor degree but most past studies suggest most patients using the drugs will still mount excellent antibody titers after vaccination. The majority of hair loss patients who use JAK inhibitors won’t be asked to stop their medications before going for vaccination. Again, this will be handled on a case by case basis with each patient.
Could the COVID vaccines cause autoimmune disease?
The follow up in trials is not long enough to know this answer yet. Most experts feel the risk is very low that COVID mRNA vaccines will incite an autoimmune disease. Over time, a more exact answer will be possible.
Could the COVID 19 vaccine worsen autoimmune disease?
It’s possible there could be some minor flares of autoimmune disease activity for a few days or few weeks in some patients. This will need to be studied. It’s also possible it won’t! So stay tuned for more information as time goes by. We don’t know how common this would be or which types of diseases are more likely to be affected than others. In the rare event that a person’s autoimmune disease does flare, most experts feel that the activity will settle again with treatments or simply with time. Some autoimmune diseases may be more likely to flare after vaccination than others. That does not mean a patient should not get vaccinated, only that they will need to be more closely monitored. We’ll know more over time about whether or not autoimmune diseases have the potential to flare with COVID 19 vaccination.
Given how common autoimmune disease is in the population, it should be pointed out that there were likely some clinical trial participants among the 35,000 patients who received the vaccines in the clinical trials who actually had some background autoimmune disease. To date, we have no indication of new onset autoimmune disease among vaccine trial participants.
mRNA vaccines are not new. It’s true that they have not been approved for use before prior to these two vaccines being approved. However, mRNA vaccines have been studied for several decades, starting back in the 1990s. We do know that mRNA vaccines do cause strong type 1 ‘interferon’ responses so it’s “possible” that vaccination would worsen autoimmune diseases that are known to be mediated by the chemical interferon. Fortunately, the risk seems very low. But again - stay tuned for more information as time goes by. The diseases that are mediated by interferon would include well known conditions such as lupus and rheumatoid arthritis. In the context of hair loss, we know that interferon-mediated diseases include alopecia areata, lichen planopilaris (LPP) and frontal fibrossing alopecia (FFA). So there is a theoretical risk that these types of diseases will flare with COVID vaccination; However, if there is true risk it’s probably really really small. In case you missed that - you should read that sentence again. if there is true risk it’s probably really really small. And the benefits of getting the vaccine massively outweighs the risks for most people with these conditions.
Ongoing Studies about Vaccination in Patients with Autoimmune Disease.
There are now studies underway to determine if patients with autoimmune diseases have different responses to the vaccine. For example, a study conducted at Washington University is following patients with rheumatic disease, inflammatory bowel disease, uveitis, autoimmune dermatologic conditions, and multiple sclerosis to see how they do after being vaccinated. The study is called the “COVID-19 Vaccine Responses in Patients with Autoimmune Disease” or the COVaRiPAD Study for short. The study will examine whether patients with autoimmune disease mount high antibody titers after vaccination and whether they have more side effects or less side effects compared to patients without autoimmune diseases. I’m keenly interested in these results.
Conclusion: Should I get a COVID vaccination?
Many things in life have risk. But we must always balance the benefits and the risks when deciding on whether or not to undertake any action. Everyone needs to assess the potential small and yet unknown complete risks of vaccination and determine how this measures up to the potential life saving or disease sparing benefits of the vaccination.
A Closer Look at How People Perceive Risk and Benefit
It’s important to understand the concepts of true risk and perceived risk and true and perceived benefit. True risk is the actual risk that is attached to any action. Perceived risk is what the patient “feels” the risk is. The same applies to true and perceived benefit. The amount of perceived risk and amount of perceived benefit will influence whether a patent commits to an action or not.
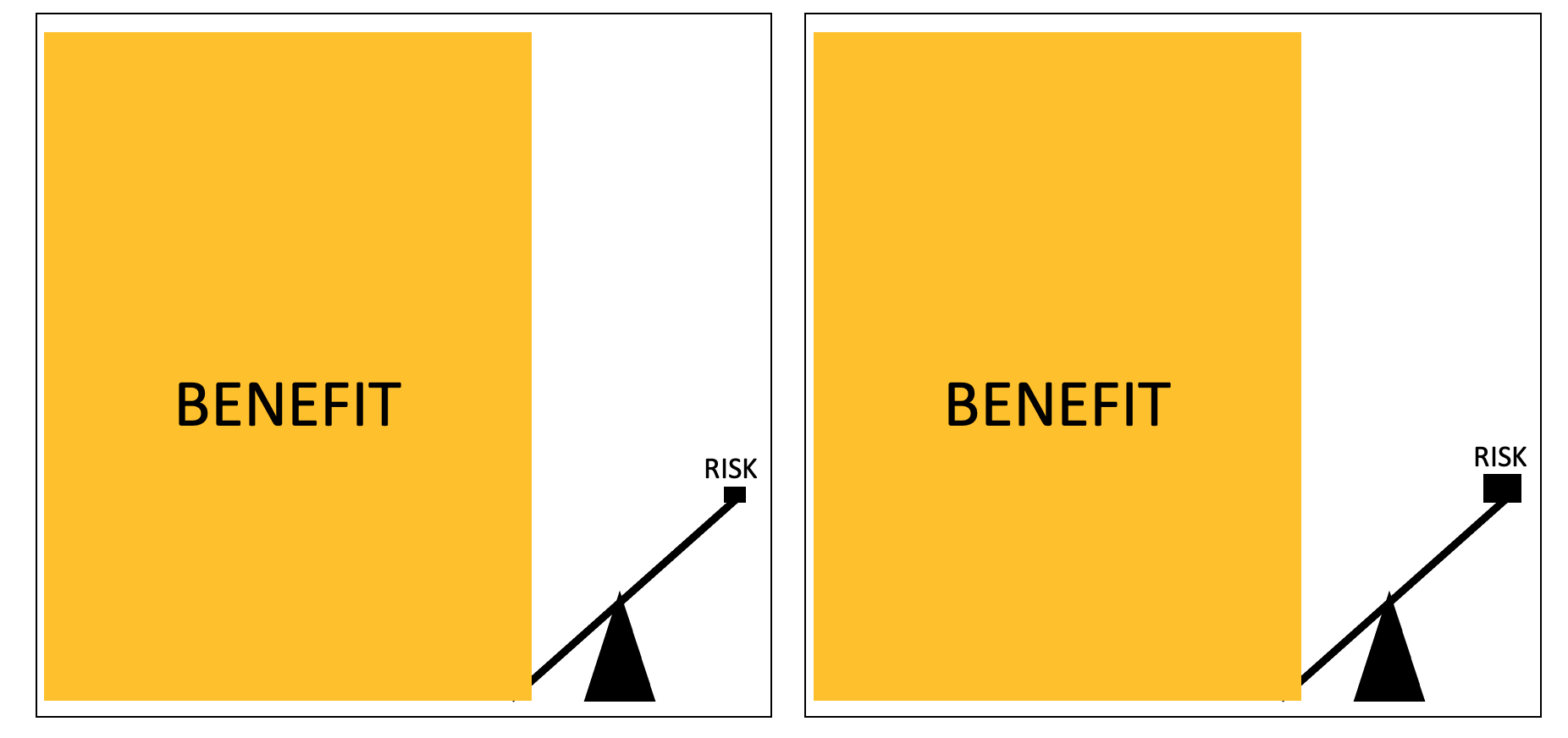
The following diagrams helps summarize our current thinking about COVID vaccinations in those with autoimmune hair loss diseases.
When it comes to assessing risk and benefit, what matters a great deal is ‘perceived’ benefit. It of course matters what the “true benefit” and true risk is but when it comes down the the patient actually rolling up their sleeve and getting the vaccine, what actually matters is how they themselves perceive risk.
Everyone has their own internal calculation of the perceived risk and perceived benefit of getting the vaccine. For some, the benefits in their mind are viewed as enormously high and the risk small. This is shown on the diagram to the right side below. These patients want to get the vaccine immediately and these are the people who rush to get the vaccine. Then there are the individuals who review the risk as small as well but they view the benefits as high - just not enormously high. These patents are excited to get the vaccine but are willing to wait their turn for when they are told they should be getting the vaccine.
Next, we have those individuals who feel the benefits are high, but have varying degrees of concerns about risks. Patients who perceive the risk is small are going to want to get the vaccine as soon as it is offered to them. These groups are shown on the left in the diagram below. Those who have higher degree of risk will want to wait until more gets it before they sign up. This is shown on the right. These patients can list off all the benefits of the vaccine but will have concerns about the risks. These people feel some uncertainty about the vaccine and feel to some degree they are guinea pigs in the overall world administration of the vaccine. They want to wait.
Benefits vs Risk for Patients with Autoimmune Disease
In an ideal ‘hypothetical’ situation, the benefits of a vaccination are very high and the risks of vaccination are very very low or zero. This is shown on the left side of the diagram below. The challenge for people with autoimmune disease is that they don’t really have data available to them yet to formulate their own internal perceive risk calculation.
In the current world, we know that the risk of vaccination for patients is not zero, but it’s still very low. For patients with autoimmune disease, we don’t know if the risk is “very, very, very low” OR “very low” relative to the massive benefits that the vaccine can bring. Experts believe it’s one of these rather than being high.
In an ideal or perfect situation, a vaccine has great benefit and no risk. In the real world, vaccines carry small risks but the risks are generally very small compared to the potential benefits. Each patient needs to assess how they perceive benefit and risks for any treatment. For the COVID mRNA vaccines, the magnitude of risk is quite low for most people with autoimmune hair loss conditions compared to the benefits of preventing or reducing disease with the vaccine. What we don’t yet know is if different autoimmune diseases have slightly different risk. Perhaps autoimmune disease 1 has a risk benefit as shown in the diagram on the left and autoimmune disease 2 has risk benefit shown in the diagram on the right. The risk overall, is still likely to be very very low. Regardless of which it is - the benefits stand out as far exceeding the risk for most people.
In an ideal or perfect situation, a vaccine has great benefit and no risk. In the real world, vaccines carry small risks but the risks are generally very small compared to the potential benefits. Each patient needs to assess how they perceive benefit and risks for any treatment. For the COVID mRNA vaccines, the magnitude of risk is quite low for most people with autoimmune hair loss conditions compared to the benefits of preventing or reducing disease with the vaccine. What we don’t yet know is if different autoimmune diseases have slightly different risk. The risk overall, is still likely to be very low.
Conclusion
When my patients ask me “should I get the vaccine?” I need to assess two things. I need to assess what I feel is the true risk-benefit in their case and then I need to assess their perceived risk benefit. The two are very different but both important. The first part is usually quite easy for most patients - the true benefit off vaccination generally massively outweighs the risks. Not that the risk is zero but that the benefits massively outweigh the risks.
But what about the perceived risk? Many patients are terrified of getting the vaccine. They intellectually understand that there is benefit, but they are scared of worsening an autoimmune disease they have worked so hard to control in the months and years leading up to the present time. For many, the perceived risk is incredibly inflated due to general fear and anxiety that the pandemic has brought with it. My job is understand their perceived risks and perceived benefits to help patients determine the right choice for them.
Further Information on the Pfizer and Moderna Vaccine
Further information is available here:
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.