What's really better? Vertical or horizontal sectioning for scalp biopsies?
Vertical and Horizontal Sectioning Seems Similar for Diagnosing Scarring Alopecias. Horizontal Has Advantages for Non-Scarring
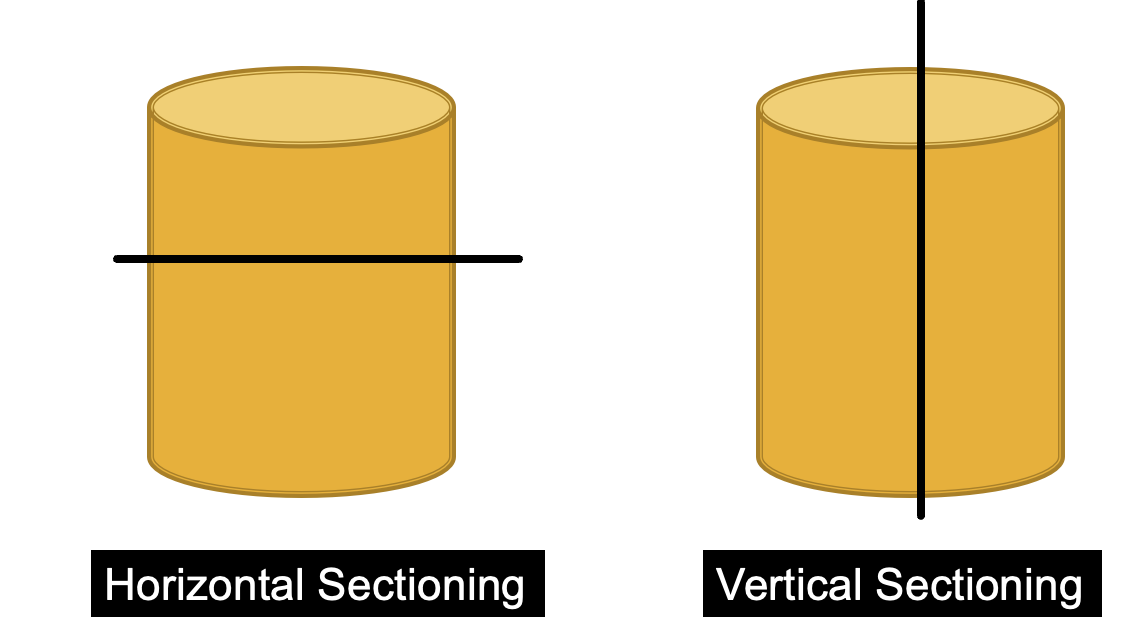
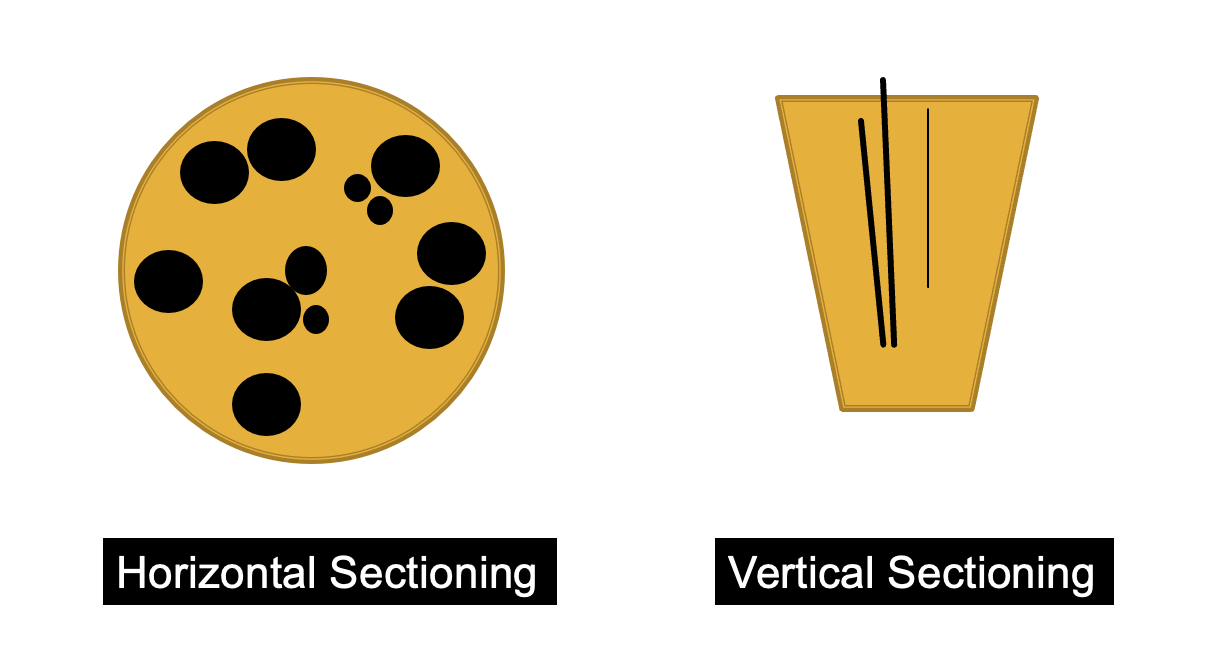
There are two common ways that scalp biospies can be processed in the pathology lab. One is with horizontal secctions and one is with vertical sections. There has been considerable debate over the years regarding which technique is superior and in which situations one might be better than another.
A nice study from New Delhi compared the benefits of horizontal and vertical sections in accurately diagnosing scarring and non-scarring alopecia. The author’s study included 78 patients with alopecia – including 43 with non scarring alopecia and 35 with scarring alopecia. The mean age was 27.7 years; the male: female ratio was 1.4:1, and the mean duration of hair loss was 4.4 years.
The 43 cases of non-scarring alopecia were divided as follows: alopecia areata: 25; androgenetic alopecia: 16; chronic telogen effluvium and trichotillomania: 1 each.
The 35 cases of cicatricial alopecia were divided as follows: lichen planopilaris: 15; pseudopelade of Brocq: 12; discoid lupus erythematosus: 4; folliculitis decalvans: 3; linear morphea: 1.
Two Dermatopathologists evaluated the slides.
Results
All in all the authors found that the diagnostic accuracy of horizontal (transverse) sections was significantly more than vertical sections for alopecia areata (97.7% and 86%, P = 0.05) and androgenetic alopecia (97.7% and 81.4%, P = 0.01). The results were similar with both techniques for lichen planopilaris (vertical section = 100%; transverse section = 97.1%, P = 0.30) and pseudopelade of Brocq (vertical section = 100%; transverse section=97.1%, P = 0.30).
The authors found that greater detail could be ascertained from horizontal sections. For example, catagen and telogen hairs, miniaturization were found significantly more often in biopsied performed using transverse sections than vertical sections.
The authors found that 20 % of alopecia areata could not be diagnosed on vertical sections. Similarly, in androgenetic alopecia, miniaturisation was missed in 44 % of cases on vertical sections and in just 6 % in horizontal sections.
Overall the authors proposed that horizontal and vertical sections were equally helpful for scarring alopecia whereas horizontal sections were more helpful for diagnosing non scarring alopecia.
Discussion
This is a nice study. The debate about horizontal and vertical sections continues in our field. Some centers use vertical sections because they don’t know how to prepare horizontal sections and the pathology lab simply does not have the skills to prepare them. Some centers use vertical sections because the pathologist is more comfortable reading vertical sections and has not been trained in reading horizontal sections.
In 2016, a meta-analysis by Du et al published in the European Journal of Dermatology did not find a statistically significant difference in the accuracy of horizontal and vertical sections. For evaluating non-scarring alopecia, there were eight studies examining the use of horizontal sections and eight examining the use of vertical section. The pooled diagnostic rates were 0.81 (95% CI: 0.70-0.92) and 0.76 (95% CI: 0.60-0.93). For the diagnosis of scarring alopecia, there were three studies examining the use of horizontal sections and five examining the use of vertical sectioning. The pooled diagnostic rates were 0.86 (95% CI: 0.66-1) and 0.90 (95% CI: 0.82-0.98). Overall, the authors concluded that based on published studies, no significant difference existed between horizontal and vertical sectioning techniques in the diagnosis of alopecia.
There are many factors that are relevant when I send my biopsy off to the lab. The first is the pre-test probability of various diagnoses. What do I think the diagnosis is before sending it in the pathologist? The second is how good of a biopsy was it? Did I take if from a location on the scalp that really has the features that I’m wondering about.
The third is the skill of the dermatopathologist. Does he or she enjoy reading pathology of hair and gives good report?
For scarring alopecia, it’s clear in my mind that excellent evaluations can come from both. It does seem that horizontal sections really help in challenging cases and early diagnoses. In alopecia areata, the horizontal sections can capture other findings that just “peribulbar inflammation” that we wait to see in the vertical sections. They can capture the shift in catagen hairs and the miniaturization. In AGA, the horizontal sections can beautifully capture the T:V ratios that sometimes just can be seen in vertical sections.
We probably still have some debate left in us about the utility of horizontal and vertical sections. Some centres take a single biopsy and perform both types of cuts on a single biopsy. This is called a Hovert technique and was described in 2011 by Nguyen and colleagues.
REFERENCE
Yadav et al. Vertical versus transverse sectioning in histopathological diagnosis of alopecia: A comparative study. Indian J Dermatol Venereol Leprol. 2022 Sep 17;1-4.
Du et al. Diagnostic value of horizontal versus vertical sections for scarring and non-scarring alopecia: a systematic review and meta-analysis. Eur J Dermatol . 2016 Aug 1;26(4):361-9. doi: 10.1684/ejd.2016.2797.
Nguyen J et al. The HoVert technique: A novel method for the sectioning of alopecia biopsies. J Cutan Pathol. 2011;38:401–6.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.