Hydroxychloroquine Dosing: Electronic Medical Records Help (A bit) to Keep Prescribers on Track
Despite a Computer Algorithm 1 out of 5 Patients Still Getting Too High of Hydroxychloroquine Doses
Hydroxychloroquine is widely used in hair loss clinics to treat certain types of lymphocytic scarring and non scarring alopecia. I use hydroxychlorquine to treat discoid lupus, systemic lupus, lichen planopilaris, frontal fibrosing alopecia (and rarely mild cases of dermatomyositis). Hydroxychloroquine has the chance of causing a retinopathy - or damage to the retina. The chance of this is around 1 % in the first five years of use and 2 % after 10 years of use.
In 2016, the American Academy of Ophthalmology (AAO) published updated guidelines for ophthalmic-safe hydroxychloroquine dosing, recommending the daily maximum dose to be 5 mg/kg of actual body weight (ABW). By respecting these dosing guidelines, the chance of retinopathy remains at 2 % after 10 years of use.
See “Hydroxychloroquine and Retinal Safety: New Guidelines”
Despite the 2016 AAO Guidelines, Many Patients Still OverDosed
A 2021 study suggested that there was still a very significant proportion (27%) of outpatient hydroxychloroquine prescriptions that are above the dosing recommendation given by the AAO guidelines.
Chen et al, 2022
A study by Chen and colleagues from the Cleveland Clinic and Case Western University examined the potential benefits of a clinical decision support tool attached to an electronic medical record that sends warnings when dosing of hydroxychloroquine is above 5 mg per kg or 400 mg. Authors studied whether the new warning system helped reduced the chances of patients being given too high of doses. They compared ‘preintervention’ data with ‘post intervention’ data.
Over 7000 patients were studied. Mean daily dose decreased from 340 mg pre-intervention to 324 mg postintervention (P < .001). 0.8% (50/6,539) of prescriptions in the preintervention group exceeded 400 mg. This dropped to 0.22% (17/7,417) prescriptions in the post intervention group. (P < .001).
Overall, the prevalence of excessive dosing (defined as >5 mg/kg/ day ABW) among all prescriptions decreased from 27.4% pre-CDS to 21.1% post-CDS (representing a 29% reduction; P < .001).
In multivariate analysis, patients with low body weight were 76 times more likely to be given an excessively high dose. In addition, non rheumatologists were 1.6 times more likely to give an excessively high dose compared to a rheumatologist.
Conclusion
Using a computer reminder tool, overdosing of hydroxychloroquine decreased by 29% (from 27.4% to 21.1%) in a large US healthcare system. The overall prevalence of outpatient prescriptions exceeding 400 mg daily also decreased fourfold from 0.8% to 0.2% postintervention. Risk factors of excessive dosing after the intervention included low weight and nonrheumatologist prescriber.
It’s still concerning that despite fancy computer interventions, one in five patients are still receiving too high of doses. More efforts are needed to reduce the chances of hydroxychlorquine overdosing in our population.
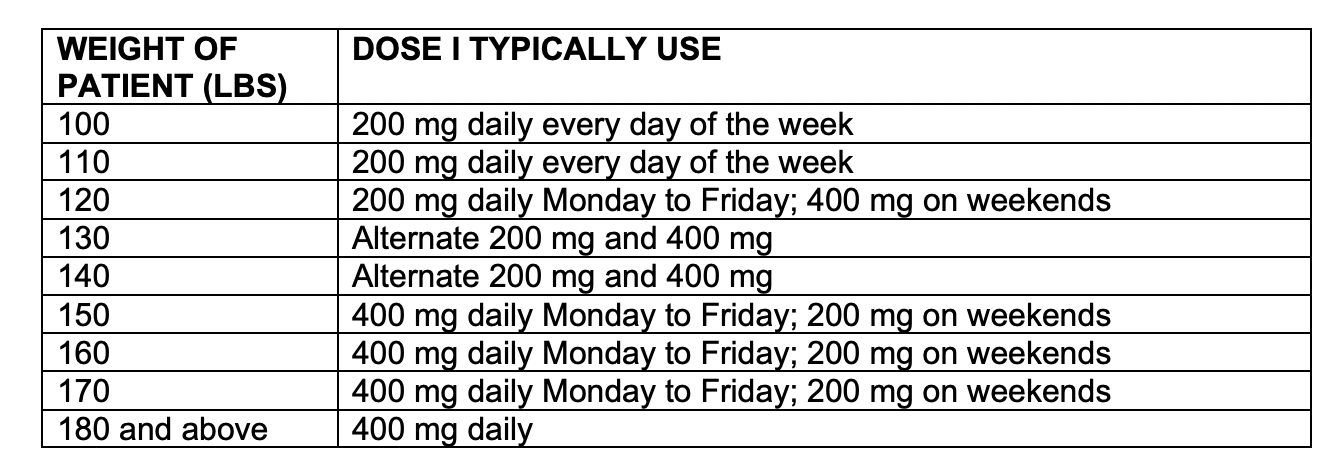
Below is a helpful table that we use in our clinic every time we see a patient on hydroxychloroquine. Unless someone is over 180 pounds, I’m not going to prescribe 400 mg dosing.
REFERENCE
Chen R et al. Impact of an Electronic Decision Support Tool to Improve Ophthalmic Safety in Hydroxychloroquine Prescribing Practices Ophthalmic Surg Lasers Imaging Retina. 2022 Jun;53(6):310-316.
Marmor MF, Kellner U, Lai TYY, Melles RB, Mieler WF; American Academy of Ophthalmology. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 revision). Ophthalmology. 2016;123(6):1386-1394. https://doi.org/10.1016/j. ophtha.2016.01.058 PMID:26992838
Chen RI, Chen AX, Greenlee TE, Conti TF, Deal C, Singh RP. Hydroxychloroquine prescription practices after 2016 American Academy of Ophthalmology recommendations. Ophthalmology. 2021;128(7):1112-1114. https://doi. org/10.1016/j.ophtha.2021.03.022 PMID:33741377
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.