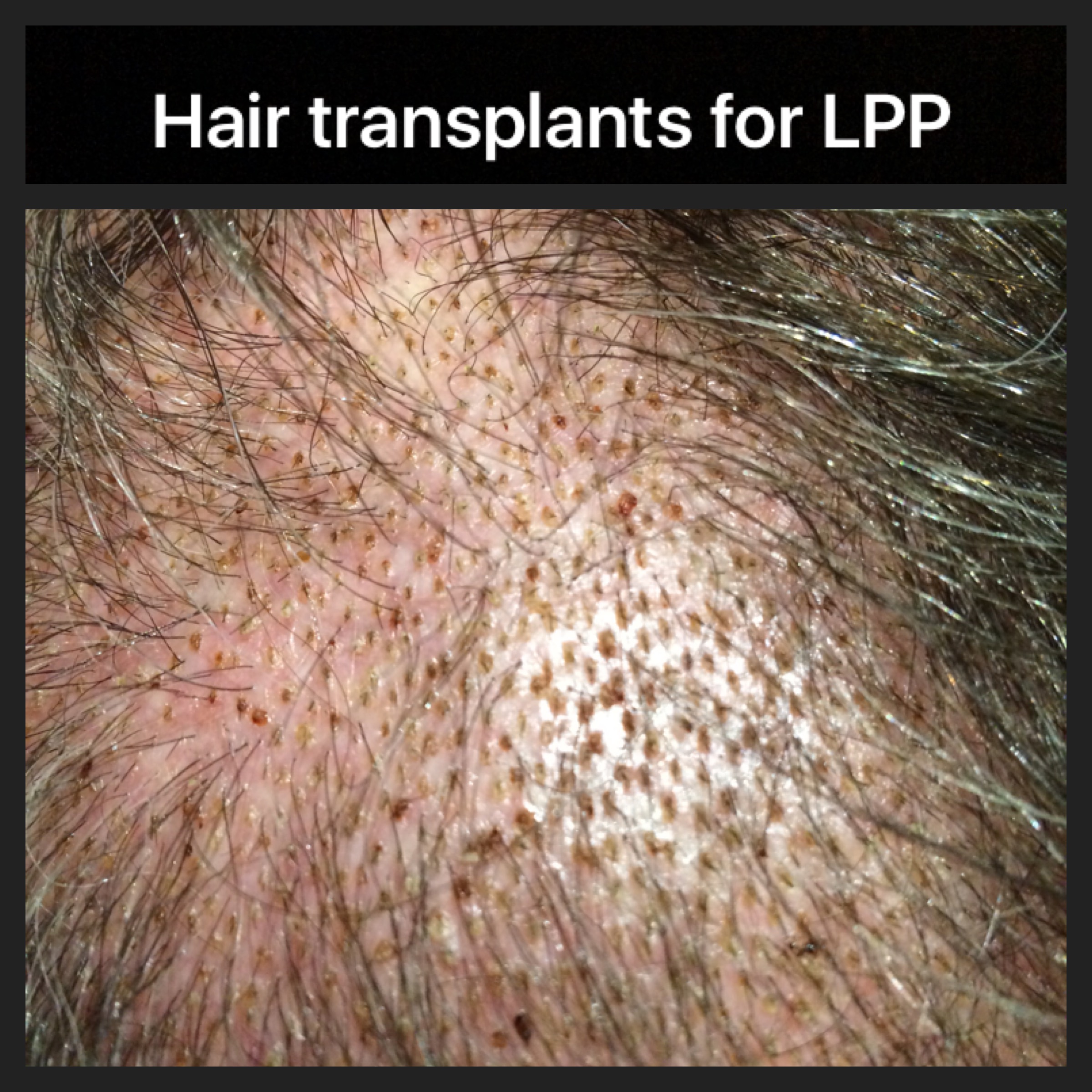
Hair transplants for Lichen planopilaris
Are hair transplants possible for LPP?
I frequently perform hair transplants for a group of conditions known as scarring alopecias. These conditions are frequently autoimmune in nature and have names like lichen planopilaris, frontal fibrosing alopecia, central centrifugal cicatricial alopecia.
When can a hair transplant be done in LPP?
A hair transplant is not possible for many patients with these conditions because the condition is "active." However, once the condition becomes "quiet" - a hair transplant can be considered.
By 'quiet', several conditions must be met. These are summarized in the LPP Hair Transplant Criteria.
Donovan LPP Hair Transplant Candidacy Criteria
In order to be a candidate for hair transplant surgery, ALL FIVE of the following criteria must be met:
1. The PATIENT should be off medications.
Ideally the patient should be off all topical, oral and injection medications to truly know that the disease is "burned out (burnt out)". However, in RARE cases, it may be possible to perform a transplant in someone using medications AND who meets criteria 2, 3 and 4 below. This should only be done on a case by case basis and in rare circumstances. It is a last resort in a well-informed patient.
2. The PATIENT must not report symptoms related to the LPP in the past 12 months, (and ideally 24 months) .
The patient must have no significant itching, burning or pain. One must always keep in mind that the absence of symptoms does not prove the disease is quiet but the presence of symptoms certainly raises suspicion the disease could be active. Even the periodic development of itching or burning from time to time could indicate the disease has triggers that cause a flare and that the patient is not a candidate for surgery. The patient who dabs a bit of clobetasol now and then on the scalp to control a bit of itching may also have disease that is not completely quiet.
3. The PHYSICIAN must make note of no clinical evidence of active LPP in the past 12 months, (and ideally 24 months).
There must be no scalp clinical evidence of active LPP such as perifollicular erythema, perifollicular scale (follicular hyperkeratosis). This assessment is best done with a patient who has not washed his or her hair for 48 hours. Some scalp redness may be persistent in patients with scarring alopecia even when the disease is quiet. Therefore scalp redness alone does not necessarily equate to a concerning finding. Perifollicular redness however is more concerning for disease activity. In addition, the pull test must be completely negative for anagen hairs and less than 4 for telogen hairs. A positive pull test for anagen hairs indicates an active scarring alopecia regardless of any other criteria.
4. Both the PATIENT and PHYSICIAN must show no evidence of ongoing hair loss over the past 12 months (and ideally 24 months).
There must be no further hair loss over a period of 24 months of monitoring off the previous hair loss treatment medications. This general includes the patient and physician's perception that there has been no further loss as well as serial photographs every 6-12 months showing no changes.
5. The patient must have sufficient donor hair for the transplant.
Not all patients with LPP maintain sufficient donor hair even if the disease has become quiet.
The Chance of Disease Reactivation Following Surgery
It is important to be aware that any patient with LPP is at risk for reactivation or a 'flare' of their LPP after surgery. The risk, I estimate based on all the patients I follow, is as follows:
LPP Reactivation Risk (Donovan, J, unpublished data)
i) A patient with active LPP before their transplant is nearly guaranteed to have a flare of his or her LPP if a hair transplant is done. (estimate 90-100 % chance of flare within 2 years post transplant)
ii) A patient with partially active LPP before their transplant is very likely to have a flare if a hair transplant is done. (estimate 70-90 % chance of flare within 2 years post transplant)
iii) A patient with medication induced inactive LPP before their transplant has a moderate chance of a flare if a hair transplant is done (estimate 50-70 % chance of flare within 2 years post transplant)
iv) A patient with inactive LPP off all medications for 1 year before their transplant has a low chance of a flare if a hair transplant is done (estimate 10-25 % chance of flare within 2 years post transplant)
v) A patient with inactive LPP off all medications for 2 years before their transplant has a low but definite chance of a flare if a hair transplant is done (estimate less than 10% chance of flare within 2 years post transplant)
What are the differences between transplants in LPP vs other types of hair loss (genetic hair loss)?
The difference between performing hair transplants for scarring alopecia and hair transplants for genetic hair loss is that the grafts are at slight risk of being lost in those with scarring alopecia. For example, in genetic hair loss we generally say the grafts are permanent. That is not the case in scarring alopecia. There is a very small albeit definite risk of reactivation of the disease that needs to be carefully monitored and followed.
Due to the small risk of reactivation in scarring alopecia, I am a big believer in keeping patients on some type of baseline treatment to keep the condition quiet.
My general principles for transplanting scarring alopecia include:
1. Considering small test sessions when appropriate.
2. Limiting the amount of epinephrine
3. Minimizing over trimming of grafts to ensure healthy proportion of stem cells get transplanted
4. Use of minoxidil in some cases pre and post op to promote blood blow
5. Adhering to densities 20-30 FU/cm2
6. Restarting topical, injection or oral immunomodulatory medications on a patient specific protocol (depending on the specific condition, how long the patient has had it, amount of hair loss, age). Although I frequently like to know a patient has been stable off medications for a prolonged period of time, I frequently restart periodic use of a corticosteroid or periodic use of low dose hydroxychloroquine depending on a number of factors. It must be noted that 10-25 % of patients with what would be considered quite 'inactive' disease will have flare so in our clinic we are quite aggressive in suppressing inflammation pre op and post op.
Further reading
Consider reading the following articles for further information
What are the clinical signs of LPP?
Conclusion
Hair transplantation for scarring alopecia is among the most challenging types of hair transplants. In the appropriate patient, it can be a very helpful means to improve density. I generally recommend that patients have inactive disease for 2 years, meaning that there has been no hair loss and no scalp symptoms over a period of 2 years.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.