Hair loss and Mixed Connective Tissue Disease (MCTD):
Hair loss occurs in 20-50 % of Patients with MCTD
Hair loss is often present in an autoimmune disease known as mixed connective tissue disease and we’ll examine the criteria here. MCTD is a condition that is less familiar to some hair specialists. Because hair loss is fairly common in MCTD, it’s something that hair specialists need to understand.
The group of conditions known as “connective tissue diseases” are very familiar to rheumatologists. Common connective tissue diseases include systemic lupus, scleroderma and Sjogren’s syndrome. Because these diseases typically affect multiple organ systems - other medical specialists frequently become involved in the care of patients with connective tissue disease. For example, skin diseases are extremely common in many of the connective tissue diseases and medical dermatologists are therefore generally well versed in these autoimmune conditions.
Defined, Undifferentiated and Mixed Connective Tissues Diseases : What do these terms all mean anyways?
Some connective tissue diseases have criteria for diagnosis and classification. Currently, there are specific criteria for classification for five defined autoimmune connective tissue diseases including 1) systemic lupus erythematosus (SLE), 2) scleroderma, 3) myositis, 4) rheumatoid arthritis (RA), and 5) Sjogren’s syndrome. All of these five conditions have variable presentation, meaning they don’t always present the exact same way in every patient. However, over an extended period of time, the diagnosis of a well-defined CTD is readily apparent. In other words, we can feel confident over time in saying a patient has lupus and not Sjogren’s and we can feel confident saying another person has rheumatoid arthritis and not lupus.
What is Undifferentiated Connective Tissue Disease, UCTD?
Some patients with autoimmune presentations, however, don't fit the “defined” criteria of these 5 diagnosis very well. It’s difficult to say for sure that a person has any one condition. For example, a patient may have features characteristic of autoimmune diseases such as Raynaud’s phenomenon (RP), myalgia (muscle pains) arthralgias (joint pains), or a positive anti-nuclear antibody (ANA) blood test, but they don't really meet criteria for a defined condition like lupus or myositis or scleroderma. in those cases, the diagnosis may not be obvious. Such patients are often diagnosed as having undifferentiated connective tissues disease or “UCTD.” Patients with UCTD typically have Reynaud’s phenomenon as well as joint symptoms (arthritis/arthralgias, nonspecific rashes, and sicca symptoms (dry mouth and dry eyes).
A small proportion of patients with UCTD proceed over time to develop a well defined connective tissue disease. In 2003, Bodolay and colleagues published a study on 665 Hungarian patients with UCTD who were followed for five years. In that group, one-third of patients (34 %) with a diagnosis of UCTD eventually went on to develop a well-defined CTD: The most common type was rheumatoid arthritis (RA) in 13.1%, Sjogren’s syndrome in 6.8%, SLE in 4.2%, scleroderma, in 2.8%, MCTD in 4.0%, systemic vasculitis in 3.3% and myositis in 0.5%. 12.3% of the patient’s achieved complete remission. A very important point of the Bodolay study was that it’s the first tow years after diagnosis of UCTD that really matter. The first two years after diagnosis carry the highest probability of a patient developed a defined.
What is an Overlap Syndrome? … and What is MCTD ?
Some patients who come into the office seem to meet criteria for not only 1 autoimmune disease but 2 autoimmune diseases or even 3. Some develop the various conditions at the same time. Others developed one type first and then developed a second over time. For example, a patient may develop what appears to be lupus and then develop a rheumatoid arthritis type picture a few years later. Patents often show positive blood tests for both the conditions. These are what we refer to as ‘overlap syndromes”
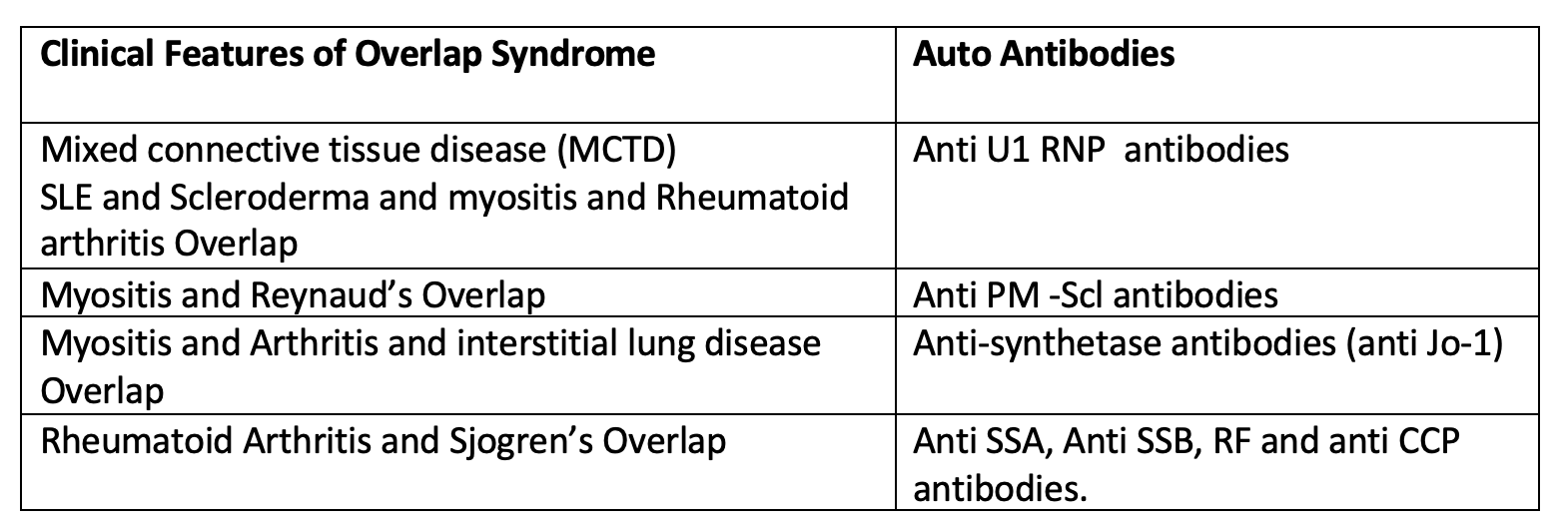
Examples of overlap syndromes include 1) mixed connective tissues disease , “MCTD” as well as 2) the myositis/Reynaud’s overlap syndrome 3) a myositis, arthritis and interstitial lung disease overlap syndrome and 4) a rheumatoid arthritis and Sjogren’s overlap syndrome. The antibodies from blood tests that define these conditions are shown below. Therefore mixed connective tissue disease is a type of overlap syndrome and is characterized by high titres of a specific antibody on blood tests known as “RNP” (ribonucleoprotein).
MCTD: A Type of “Overlap” Syndrome
Mixed connective tissue disease (or MCTD) is a condition that rheumatologists are quite familiar with. It was first recognized in 1972 by Sharp and colleagues. The term MCTD is a term used to describe an immune system disorder that has mixed or overlapping features with several conditions including systemic lupus erythematosus, systemic sclerosis, and polymyositis and rheumatoid arthritis. Many patients with MCTD have Sjogren’s syndrome as well. When patients with MCTD have features of all these conditions they typically occur sequentially over time rather than develop simultaneously. Early in the course of disease, patients may have somewhat nonspecific symptoms such as fatigue, myalgias, arthralgias, and especially Raynaud’s phenomenon.
Patients with certain systemic features along with a positive ANA, high titres of antiRNP antibodies and negative results to other antibody tests are mosts likely to have MCTD. The key to MCTD compared to other rheumatological conditions is the high titre of anti-RNP antibodies.
It is the very high titer ANA and anti U1-RNP antibodies that often give a first clue to MCTD. It’s also important to note that patients with MCTD show a lack of other specific autoantibodies.. Antibodies to double-stranded DNA (dsDNA), Sm, and SSA/SSB are not typically a feature or are low titre or only transient.
A variety symptoms and signs are present in patients with MCTD which we will review together shortly. Raynaud syndrome is present in most patients. Other features include joint pains, various skin abnormalities, muscle weakness, and a variety of internal issues affecting the lungs, joints, esophagus and heart and kidneys.
The average age of onset of MCTD is the mid 30s although the age range can range for childhood to elderly. Females are mjuch more often affected with MCTD than males.
Diagnostic Criteria for MCTD
There are several different researchers that have put forth criteria for diagnosis of MCTD. The most commonly used one is the 1987 Criteria put forth by Alarcon-Segovia.
In order to make a diagnosis of MCTD patients must have
a) blood tests showing antiRNP antibodies great than 1:1600
PLUS
b) have 3 of the following 5 clinical criteria (one of which MUST be synovitis or myositis).
1) Edema of the hands
2) Synovitis
3) Myositis
4) Reynaud’s phenomenon
5) Acrosclerosis/sclerodactyly
Several studies have provided an understanding of the spectrum of conditions that can occur with MCTD.
Skin Manifestations
Skin manifestations included swollen hands or sclerodactyly (50 percent), lupus-like or dermatomyositis like rashes on the face of hands (48 percent), periungual telangiectasia (46 percent), dyspigmentation (28 percent), photosensitivity (28 percent) and vasculitis (22 percent). Hair loss occurs in 21-46 % of MCTD patients depending on the study. It is often a diffuse type hair loss (telogen effluvium) although other patchy and inflammatory presentations may be possible as well.
Systemic issues
The systemic issues of MCTD don’t appear all at once. They can appear in a staggered manner, over many many years which complicates the diagnosis. One of the most frequent systemic issue is Raynaud’s phenomenon and is present in most patients (93 percent). Reynaud’s typically happens early in the course of the condition and affected patients note a change in finger color in the cold. Hands may go white and then blue and then red. Pins and needle like sensations are often present which are very uncomfortable. Patients may also note puffy fingers (scleroderma like changes in the hands).
Other features include arthritis or arthralgia (91 percent), arthritis (50-60 %) adenopathy (43 percent). Lung disease is found in 75 % of patients and affected patents have cough, shortness of breath and pain when they take a deep breath. Other symptoms include vascular headaches (35 percent), serositis (35 percent), hoarseness (28 percent), myositis (26-70 percent), muscle weakness and tenderness (myalgia), sicca syndrome (24 percent), renal disease (17 percent) and central nervous system disease (9 percent). A polyneuropathy may occur. Difficulty swallowing is common. Dry eyes (23%) and dry mouth (33%) are sometimes also a feature of MCTD. Some patients with MCTD present with fever.
Blood test Results and Lab Results in MCTD
Associated laboratory findings included antinuclear antibodies (100 percent), hypergammaglobulinemia (78 percent), rheumatoid factor (16-57 percent), hypocomplementemia (28 percent). Anti Sm antibodies are seen in 11 % of patients. anti dsDNA is often negative. SSA is present in 18 % of patients and SSB in 7 % of patients. Elevated muscle enzymes (CK) are seen in 25-40 %. Anemia (low hemoglobin) is seen in 25 % and low white cells (leukopenia in 37 %) can also occur. Low platelets (thombocytopenia) is less common by seen in 9 % of patients with MCTD.
Urinalysis shows proteinuria in 8 % of patients and hematuria in 15 %.
Other results that come from more sophisticated testing include esophageal dysmotility (61 percent), abnormal pulmonary function (59 percent) and pulmonary hypertension (30 %).
Treatment for MCTD
Treatment for mixed connective tissue disease is similar to the way there various other autoimmune diseases are treated. For skin issues that have an inflammatory cause, topical steroids, calcineurin inhibitors and steroid injections can be helpful. Steroid injections are particularly helpful for inflammatory scalp issues.
For systemic issues, immunosuppressive and immunomodculatory treatments are used. Hydroxychloroquine, methotrexate, mycophenolate, azathioprine are all part of the management strategies. Short (and sometimes long) courses of prednisone may be important and sometimes lifesaving.
Conclusion
Hair specialists can sometimes be the very first in line when patients develop autoimmune issues. The ability of recognize basic features of the main autoimmune diseases is important - as well as to understand the concepts behind undifferentiated connective tissues diseases and overlap syndromes.
This article highlights th importance of the anti-RNP antibody in evaluated mixed connective tissues disease and the Alarcón-Segovia Criteria.
REFERENCE
Alarcon-Segovia D and Villarreal M. Classification and diagnostic criteria for mixed connective tissue disease. In: Kasukawawa R, Sharp GC, editors. Mixed connective tissue disease and anti-nuclear antibodies. Amsterdam: Exerpta Medica; 1987. pp. 33–40.
Bodolay E et al. Five-year follow-up of 665 Hungarian patients with undifferentiated connective tissue disease (UCTD). Clin Exp Rheumatol. 2003 May-Jun; 21(3):313-20.
Prystowsky SD. Mixed connective tissue disease. West J Med. 1980 Apr;132(4):288-93.
Sharp GC et al. Mixed connective tissue disease--an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am J Med. 1972 Feb; 52(2):148-59.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.