Morgellons Disease: The Basics
Morgellons Disease
Morgellons disease (MD) is skin and scalp condition that is becoming better and better recognized. However, its cause and classification still remains open to debate. It's important for hair specialists to recognize this condition and to understand options for patients. Patients with Morgellons disease frequently lack insight, and are reluctant to be referred to psychiatrists regardless of the underlying psychopathology present. It's important for dermatologists and hair specialists to understand the options for managing Morgellon's disease.
What are the features of Morgellons Disease?
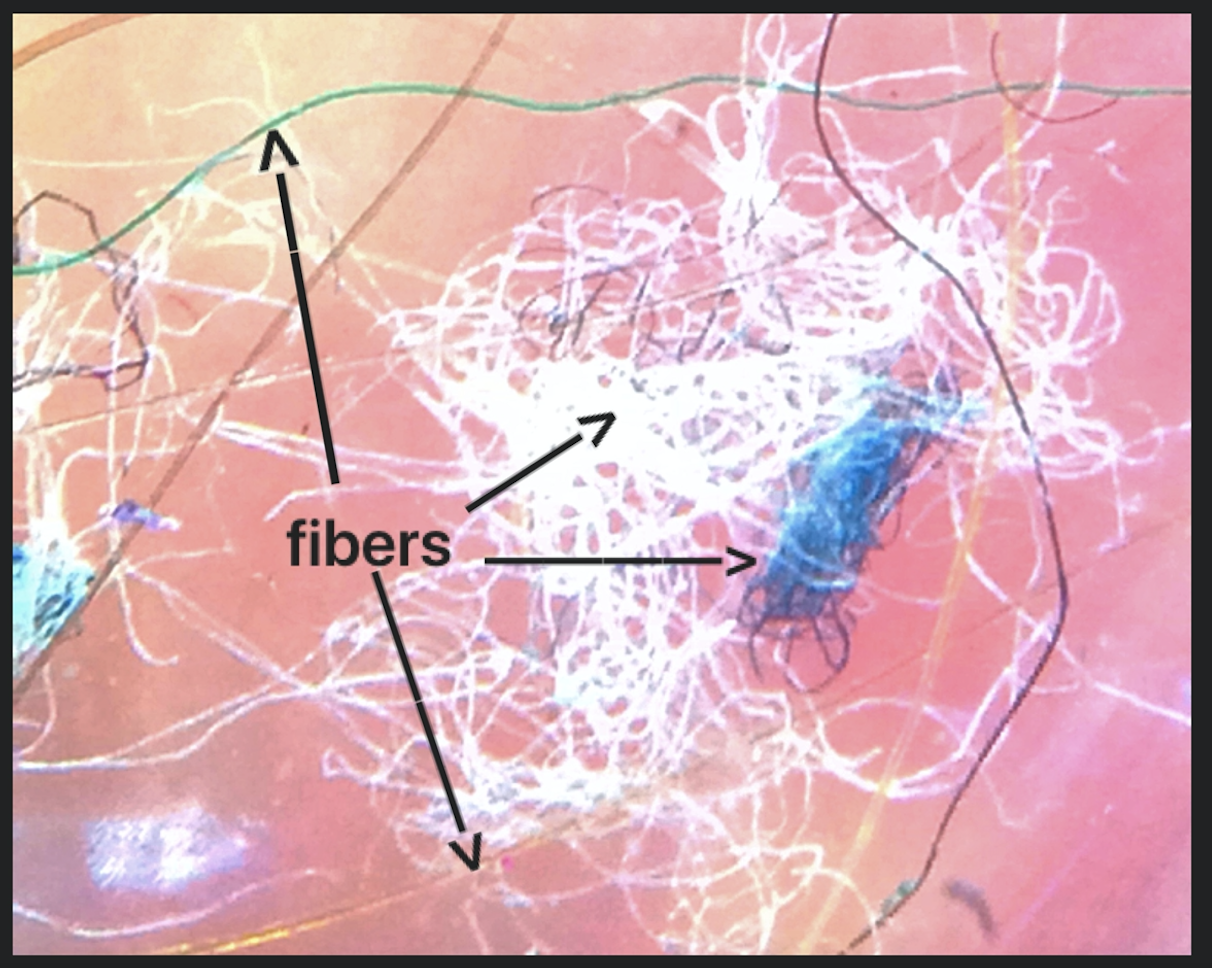
The key features of MD is the presence of skin lesions with filaments that lie under, are embedded in, or project from skin. These filaments can be many colors including white, black, or brightly coloured. The typical patient with MD has concerns that fibers of glass/other material are coming out of the skin. They may resemble cotton. Many patients (up to 25 %) self-diagnose themselves through reading on the internet. A vast majority of patients believe there are specific precipitating factors that explain the fibers. Patients may have burning, itching, stinging of the skin and sensations of something crawling. They may have fatigue, difficulty concentrating and difficulties with sleep.
How common is Morgellons Disease?
It's not clear how common the condition really is. Pearson and colleagues suggested rates as high as 3-4 people out of every 100,000 population.
What is the cause of MD?
The exact cause of MD remains a mystery. Some sources, continue to describe this as a purely psychiatric disease having overlap with Delusions of Parasitosis.
Recent research has suggested that MD patients display a variety of clinical manifestations that closely resemble symptoms of Lyme disease (LD). These symptoms include joint pain, nerve damage and fatigue. In one study, 98% of patients with MD subjects had positive Lyme disease serology and/or a diagnosis of tick borne disease. IN comparison, only 6% of LD patients in an Australian study were found to have MD.
The spirochetes identified as Borrelia spp. are thought to be alive and viable in tissue from patients from Morgellon's Disease. These spirochetes are difficulty to culture in a laboratory so PCR amplification is often used to identify Borrelia.
The exact relationship between Lyme disease and Morgellon's Disease is still open to debate. Not all experts agree with the link. A much quoted CDC study by Pearson and colleagues. did not find an infectious cause or any good proof of an environmental link in a study of 115 patients
Psychiatric Disease in Patients with MD
The central debate in the Morgellons medical literature (i.e. the medical journals) is whether MD is a psychiatric disease or a infectious disease (perhaps due to Borellia) with psychiatric manifestations. It's clear from many studies that mental illness can develop in patients affected by tick-borne disease. These include depression, mania, delusions, bipolar disorder, paranoia, schizophrenia, sensory hallucinations, major depression, and mania. Infection by spirochetes can affect how neutrons function.
The vast majority of patients with Morgellons disease have psychiatric disease as well. In one study by Harvey and colleagues, 23 of 25 Morgellons patients had psychiatric diagnoses including attention deficit, bipolar disorder, obsessive-compulsive disorder, and schizophrenia. The fact that MD patients may show neuropsychiatric symptoms is what makes this field so challenging. It makes the diagnosis challenging. It also makes it difficult to distinguish from a delusional disorder.
Animal Models of MD
Animal models of MD have arisen which provide some understanding of how human MD may come about. There is similarity between MD and an animal disease known as bovine digital dermatitis (BDD). Similar to MD, this particular animal disease is associated with ulcerative lesions exhibiting keratin projections and is an acknowledged spirochetal infection (just like human Lyme disease. In this animal model, it was confirmed that there is a bona fide causal relationship between spirochetal infection and filament formation infection with pure cultured tremens lead to the clinical disease.
What are the fibers in Moregellon's Disease?
The fibers seen in patients with MD are often mistaken by patients and physicians to be textile fibers. However, this is not correct in most cases- the fibers are composed of keratin and collagen. They are produced by epithelial cells. They come from the patient themselves because the base of these filaments are nucleated. A proportion of these fibers may actually be types of hairs.
Classification of Moregellons Disease
Middelveen and colleagues recently proposed a clinical classification system that reflects the duration and location of MD lesions:
Early localized Morgellons Disease. This is a form of MD with lesions/fibers present for less than three months and localized to ONLY ONE area of the body (head, trunk, extremities).
Early disseminated Morgellons Disease. This is a form of MD with lesions/fibers present for less than three months and involving MORE THAN ONE area of the body (head, trunk, extremities).
Late localized Morgellons Disease. This is a form of MD with lesions/fibers present for more than six months and localized to ONLY ONE area of the body (head, trunk, extremities).
Late disseminated Morgellons Disease. This is a form of MD with lesions/fibers present for more than six months and involving MORE THAN ONE area of the body (head, trunk, extremities).
Treatment of MD
Since the cause of MD can't be uniformly agreed upon and since the clinical classification of MD has not been universally accepted, it is not difficult to understand why optimal treatment strategies are still open to some amount of debate. Some view this as entirely a psychiatric disease and so much of the medical literature focuses on use of psychiatric medications.
A few principles do seem relevant:
1. Treat it early. Morgellons Disease should be treated as early as possible to improve the ultimate outcome that a patient will achieve.
2. Consider treatments that address Spirochetes. Although still controversial, treatment should be aimed at the Borrelia if there is evidence by serology or other studies. In such cases, treatment may involve prolonged antibiotic and/or anti-parasitic therapy.
3. Consider psychiatric medications. Psychiatric medications, particularly the antipsychotics are helpful in Morgellon's Disease patients with psychiatric symptoms. However, use of these medications as stand along treatments without addressing the tick infection often leads to incomplete clinical responses. Psychiatric medications that have best been studies in MD include pimozide, rispidadone, olanzapine and trifluoperazine.
4. Offer support. Patients affected by Morgellons disease often feel isolated and stigmatized. There are few resources in the medical community for patients affected by Morgellons disease.
Conclusion and Final Thoughts
Morgellons is a fascinating condition that is still poorly understood. Some experts take a position that Morgellons Disease is a real somatic condition and yet some take the stance that it's a delusion disorder. It's not all that easy to diagnose properly and the whole entity itself is surrounded with controversy. The literature on Morgellons is filled with a great deal of controversy. Many patients with Morgellon's have psychiatric disease and separating whether psychiatric disease is due to Lyme disease and Morgellons Disease and what component is due to pre-existing psychiatric disease is challenging. Furthermore, countless numbers of patients I see have been given diagnoses of Lyme disease by various clinics - even using methods that are not generally agreed upon. There is still controversy as to what 'really' constitutes Lyme disease.
Despite these controversies, I strongly believe that we need to be thinking about Lyme disease, syphilis and similar spirochetes in all patients who present to clinic with sensations of creepy crawlers, concerns about parasites, chronic itch and report of fibers emerging from their skin. If we don't think about spirochete type infections and infestations, we'll repeatedly miss this condition and the entire field of MD will remain shrouded with controversy and mystery. It's likely that many patients with true Delusions of Parasitosis will present with a Morgellons-like presentation but the reverse needs to be considered as well. The fact that a patient has psychiatric disease (including delusions), is not proof they don't have a Morgellon-like presentation. Moreover, the fact that a given patient responds to anti-psychotics is also not proof they have a Morgellon-like presentation.
We certainly need to open the dialogue in this are of medicine rather than close it. For every study that suggests there is no link between infections and Morgellon's there is a study that suggests there could be. For every study that suggests the fibers that patients find are man made external fibers, there are studies that suggest these are keratin and collagen fibers from the skin itself. The true story of Morgellons will unfold as years go by. For now, patients affected by Morgellons disease need support.
Reference
Harvey WT, Bransfield RC, Mercer DE, Wright AJ, Ricchi RM, Leitao MM. Morgellons disease, illuminating an undefined illness: a case series. J Med Case Rep. 2009;3:8243. [PMC free article][PubMed]
Kellett CE. Sir Thomas Browne and the disease called Morgellons. Ann Med Hist, n.s., VII. 1935;7:467–479.
Mayne PJ. Clinical determinants of Lyme borreliosis, babesiosis, bartonellosis, anaplasmosis, and ehrlichiosis in an Australian cohort. Int J Gen Med. 2015;8:15–26. [PMC free article] [PubMed]
Middelveen MJ, et al. History of Morgellons disease: from delusion to definition. Clin Cosmet Investig Dermatol. 2018.
Middelveen MJ, Bandoski C, Burke J, et al. Exploring the association between Morgellons disease and Lyme disease: identification of Borrelia burgdorferi in Morgellons disease patients. BMC Dermatol. 2015;15:1. [PMC free article] [PubMed]
Middelveen MJ, Stricker RB. Filament formation associated with spirochetal infection: a comparative approach to Morgellons disease. Clin Cosmet Investig Dermatol. 2011;4:167–177. [PMC free article][PubMed]
Mohandas P, et al. Morgellons disease: experiences of an integrated multidisciplinary dermatology team to achieve positive outcomes. J Dermatolog Treat. 2018.
Pearson ML, Selby JV, Katz KA, Cantrell V, Braden CR, Parise ME, et al. Clinical, epidemiologic, histopathologic and molecular features of an unexplained dermopathy. PLoS One. 2012;7:e29908.[PMC free article] [PubMed]
Savely VR, Stricker RB. Morgellons disease: analysis of a population with clinically confirmed microscopic subcutaneous fibers of unknown etiology. Clin Cosmet Investig Dermatol. 2010;3:67–78.[PMC free article] [PubMed]
Savely G, Leitao MM. Skin lesions and crawling sensation: disease or delusion? Adv Nurse Pract. 2005;13(5):16–17. [PubMed]
Savely VR, Leitao MM, Stricker RB. The mystery of Morgellons disease: infection or delusion? Am J Clin Dermatol. 2006;7(1):1–5. [PubMed]
Savely VR, Stricker RB. Morgellons disease: the mystery unfolds. Expert Rev Dermatol. 2007;2(5):585–591.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.