Scalp Sarcoidosis: Another One of the Great Mimickers
Scalp Sarcoidosis: What does one need to know?
Scalp sarcoidosis is rare. The condition is also easily missed. So many scalp conditions can look just like it. Here, we’ll take a look at a few important principles of scalp sarcoidosis, skin sarcoidosis as well as systemic sarcoidosis.
What is sarcoidosis?
Sarcoidosis is an inflammatory disease that affects multiple organs of the body. The cause is unknown. Almost every subspecialty of medicine will treat patients with sarcoidosis because of how it can affect so many different organ systems. The lungs and the lymph nodes are most commonly affected and so are the eyes. In fact, 90 % of patients with sarcoidosis have lung involvement. About one-third of patients with systemic sarcoidosis will have skin involvement which makes the skin also a common organ of involvement. Dermatologists, therefore, understand sarcoidosis fairly well. The liver, nervous system, heart and kidneys can all be involved by sarcoidosis.
The key to the diagnosis of sarcoidosis is the finding of a specific pattern of inflammation known by pathologists as “non caseating granulomas” in various organs of the body.
Who is affected?
Anyone can be affected by sarcoidosis worldwide although some studies have suggested that individuals of Irish, Scandinavian, and those of the African diaspora are more likely to have sarcoidosis. Females are more commonly affected than males.
How does the disease itself present?
A very small proportion of patients with sarcoidosis are asymptomatic. About 50% have lung symptoms of some kind (like shortness of breath, cough). Some patients have fever and weight loss. A variety of other symptoms are possible depending on the organ affected. Sometimes the skin is the first site of involvement but usually it occurs at the same time as systemic involvement. Therefore, dermatologists need to understand the different ways this disease presents itself so that they can help make the diagnosis in early stages.
How does “scalp sarcoidosis” present ?
Scalp sarcoidosis is quite uncommon. In fact, there has been less than 50 cases published in the medical literature so far. Many of these cases have been African American women who have systemic involvement. In the medical literature, 87% of patients with scalp sarcoidosis were African American with only 2 cases reported in Caucasians. Scalp sarcoidosis may be non-scarring or scarring. It is more likely to be a scarring alopecia and less likely to be non-scarring alopecia.
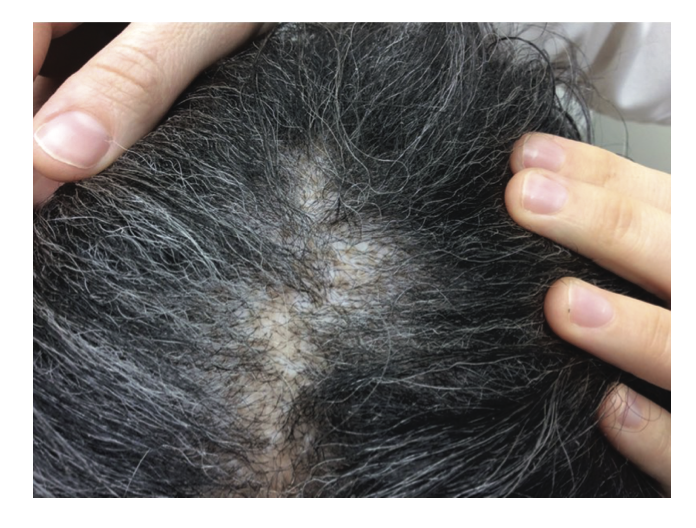
Scalp Sarcoidosis. Scalp sarcoidosis is a great imitator. Note the orange or “apple jelly” color in a female with scalp involvement. Image from Long T et al. Severe scalp sarcoidosis in an unlikely patient. JAAD Case Rep . 2020 Apr 24;6(11):1165-1166. Image used here with creative commons license.
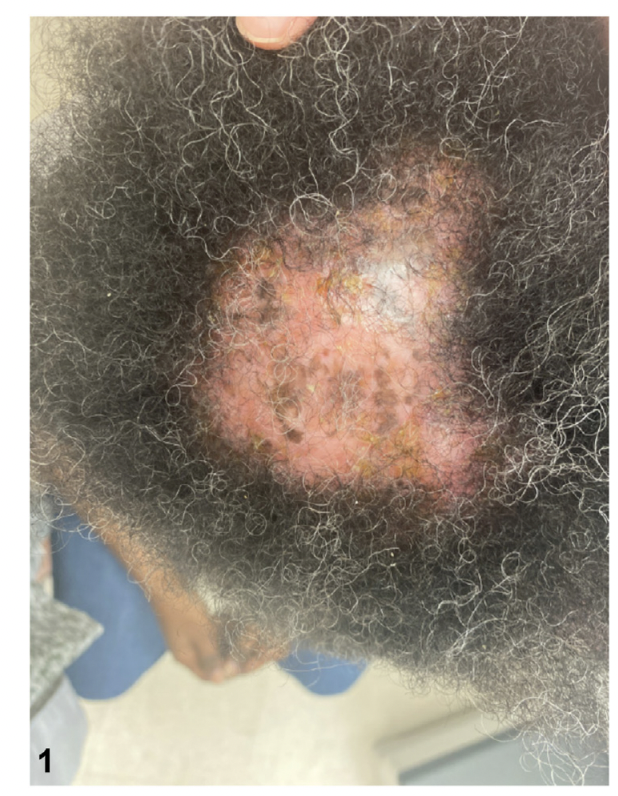
Scalp sarcoidosis resembling central centrifugal cicatricial alopecia. The patient had a history of lung sarcoidosis and had skin lesions consistent with cutaneous sarcoidosis. Image from Prohaska J et al. Scalp Sarcoidosis Presenting as Cicatricial Alopecia. J Am Osteopath Assoc . 2018 Dec 1;118(12):824-826. Image used with creative commons license.
Scalp sarcoidosis in a 43 year old woman. She did not have systemic involvement other than mildly elevated calcium levels. Image from Ghosh A et al. Single lesion of sarcoidosis presenting as cicatricial alopecia: a rare report from India. Int J Trichology . 2014 Apr;6(2):63-6. Image used with creative commons license.
Scalp sarcoidosis in a 43 year old woman. The patient’s other image is shown above. She did not have systemic involvement other than mildly elevated calcium levels. Image from Ghosh A et al. Single lesion of sarcoidosis presenting as cicatricial alopecia: a rare report from India. Int J Trichology . 2014 Apr;6(2):63-6. Image used with creative commons license.
Scalp sarcoidosis in a patient first mistaken for folliculitis decalvans. Image from House NS et al. Sarcoidosis-induced alopecia.Dermatol Online J 2012 Aug 15;18(8):4. Used with creative commons license.
A patients with scalp sarcoidosis mimicking acne keloidalis. Image from Roche FC et al. Sarcoidosis: An atypical mimicker of acne keloidalis nuchae. JAAD Case Rep. 2020 May; 6(5): 397–399. Used with creative commons license.
Image of scalp in patient with sarcoidosis. Image from Barker C et al. Scarring alopecia and scalp pruritus. JAAD Case Rep. 2022 Nov 2;30:134-136. doi: 10.1016/j.jdcr.2022.10.021. eCollection 2022 Dec. Image used with creative commons license.
Clinically, the lesions often have an orange color. They do not always especially in darker skin types. It’s important to realize that scalp sarcoidosis truly is one of the great imitators and can take on many many different appearances! and may look very similar to lichen planopilaris, discoid lupus, pseudopelade, central centrifugal cicatricial alopecia, acne keloidalis, folliculitis decalvans, necrobiosis lipoidica, scleroderma or even alopecia areata at first glance. Some present like diffuse scaling and some present with ulcerations. Just like the skin lesions (which we’ll review below), scalp sarcoidosis can take on many forms!
One of the fastest ways to get clues about a possible diagnosis of scalp sarcoidosis might be present in a patient with hair loss is to look for the skin sarcoidosis that is present elsewhere or ask about a history of systemic sarcoidosis. Most patients with scalp sarcoidosis have other clues!
Trichoscopy is a very important first step when evaluating lesions and this is generally followed up by scalp biopsy. It’s the scalp biopsy however that helps confirm the diagnosis. Confirmation of a diagnosis of scalp sarcoidosis is very important - especially if the patient is unaware that they have systemic disease. Most patients with scalp sarcoidosis will have systemic involvement.
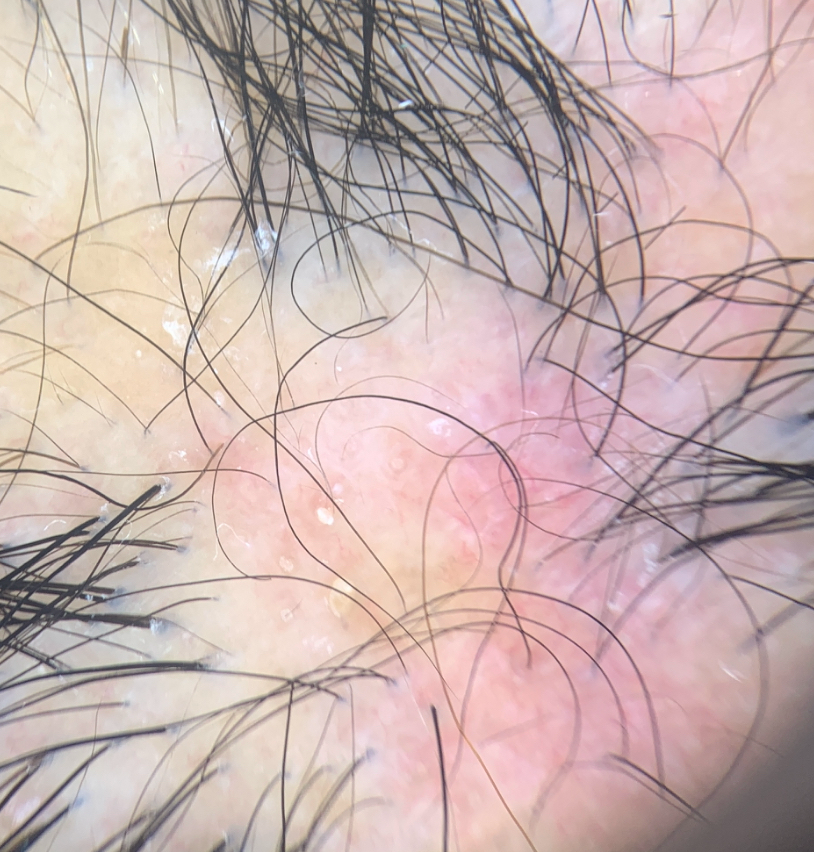
Trichosocpy of Scalp Sarcoidosis
Trichoscopy is helpful. A variety of trichoscopic findings have been described by others including Starace et al and Torres et al.
a) lack of follicular ostia
b) red-orange color (granulomas in the dermis)
c) capillaries (vasodilatation in the papillary dermis)
d) brown dilated ostia (bigger than those of alopecia areata)
e) dystrophic hairs
f) cicatricial skin spots
The orange color with the telangiectasis is thought to be quite a specific skin sign of sarcoidosis.
Trichoscopy of sarcoidosis closely mimicking discoid lupus. Red brown color and telangiectasis can be seen.
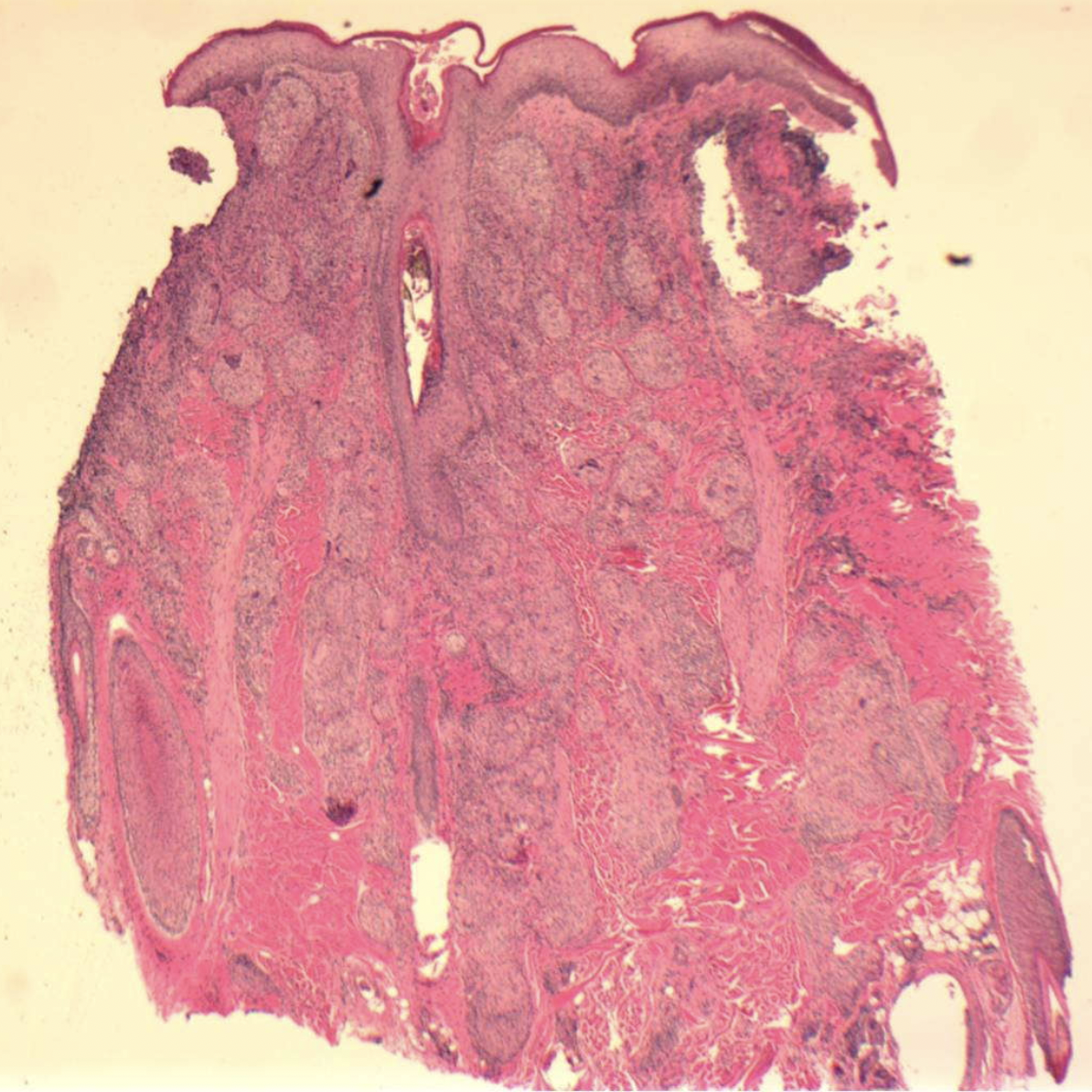
Histopathology of Scalp Sarcoidosis
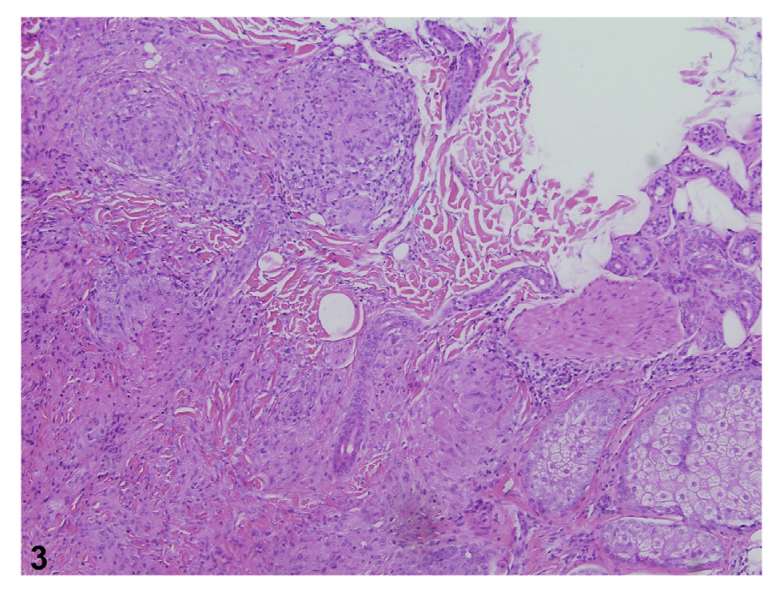
Biopsies of scalp sarcoid will show the classic pattern of inflammation that characterizes this disease: sarcoidal granulomas in the dermis. The key to the diagnosis is the characteristic noncaseating epitheloid granulomas. The central area has lymphocytes, macrophages, multinucleate giant cells and the is all surrounded by CD8 and CD4 positive T cells (and fibrosis).
Skin Biopsy (4 mm punch) showing Sarcoidosis. Biopsy from the vertex scalp showed a dense dermal granulomatous infiltrate of lymphocytes, histiocytes, multinucleated histiocytes, and scattered neutrophils with few terminal hairs. There was significant dermal atrophy. Image from Long T et al. Severe scalp sarcoidosis in an unlikely patient. JAAD Case Rep . 2020 Apr 24;6(11):1165-1166. Image used here with creative commons license.
Histopathology from a 43 year old patient with scalp sarcoidosis. The image shows typical ‘naked’ epithelioid granulomas with Langans type giant cells. There are no adnexal structures here suggesting this is a scarring alopecia. Image from Ghosh A et al. Single lesion of sarcoidosis presenting as cicatricial alopecia: a rare report from India. Int J Trichology . 2014 Apr;6(2):63-6. Image used with creative commons license.
Punch biopsy showing scalp sarcoidosis. Magnified views are shown below. Image from House NS et al. Sarcoidosis-induced alopecia.Dermatol Online J 2012 Aug 15;18(8):4. Image used and shown with creative commons license.
Punch biopsy showing scalp sarcoidosis. Naked granulomas with epithelioid histiocytes and Langhans type giant cells are seen. Image from House NS et al. Sarcoidosis-induced alopecia.Dermatol Online J 2012 Aug 15;18(8):4. Image used and shown with creative commons license.
Histology of scalp in patient with sarcoidosis showing non-caseating granulomas. Image from Barker C et al. Scarring alopecia and scalp pruritus. JAAD Case Rep. 2022 Nov 2;30:134-136. doi: 10.1016/j.jdcr.2022.10.021. eCollection 2022 Dec. Image used with creative commons license.
How does general “skin sarcoidosis” present?
Patients with suspected scalp sarcoidosis should always have their skin examined because often typical skin sarcoidosis can be found.
Skin involvement in sarcoidosis can occur at any time during the development of systemic sarcoidosis. Often it’s present at the same time the patient is diagnosed with systemic disease but it can occur before or after. Generally speaking about 20-25 % of patients with systemic sarcoidosis have skin involvement.
There are many different types of skin lesions that patents with sarcoidosis can have. These are typically classified into “specific” and “non-specific.” Specific lesions will show the famous “non-caseating” granulomas when biopsied. The commonest specific skin lesions observed clinically are reddish yellow maculopapules, plaques and subcutaneous nodules. Lupus pernio is the most specific lesion. Non specific lesions will not show the granulomatous process. There are no non caseating granulomas to be found. Examples of the non specific lesions include erythema nodosum type lesions, calcinosis cutis, prurigo, erythema multiforme, and nail changes Scalp lesions discussed above are usually specific.
Sarcoidosis is a great mimicker of so many conditions in dermatology.
In summary, sarcoidosis can appear as plaques, papules, lupus pernio (the most specific lesion), erythema nodosum, scar sarcoid, ulcerative lesions, hypopigmented patches, subcutaneous nodules as well as others too.
Skin sarcoidosis. The patient had a history of lung sarcoidosis and had skin lesions consistent with cutaneous sarcoidosis. Image from Prohaska J et al. Scalp Sarcoidosis Presenting as Cicatricial Alopecia. J Am Osteopath Assoc. 2018 Dec 1;118(12):824-826. Image used with creative commons license.
How is sarcoidosis diagnosed?
There is no one single test that proves a patient has sarcoidosis. Rather the entire clinical picture and radiographic picture needs to be taken into account.
Diagnosis of sarcoidosis generally requires fulfillment of three criteria:
(1) a compatible clinical and radiologic presentation that suggests sarcoidosis
(2) pathologic evidence of noncaseating granulomas somewhere in the body
(3) exclusion of other diseases with similar findings, such as infections or malignancy.
From the perspective of the dermatologist, the histological evidence of “non -caseating granulomas” is an important step. My job is to biopsy suspected lesions to see if we can identify these granulomas. If we can find them, we fulfil criteria 2. My radiology, internal medicine and other colleagues assist in evaluating x rays and other tests to prove that sarcoidosis fits well with the suspected diagnosis.
What tests are needed in suspected sarcoidosis?
A variety of tests can be considered after the clinician obtains a good history and preforms a complete examination. These include
a) CBC
b) AST, ALT
c) creatnine
d) serum calcium (elevated in 10-13 %) and urine calcium
The macrophages of granulomas express the enzyme 1-alpha-hydroxylase. This triggers “extrarenal” synthesis of active form of vitamin D in the sarcoidal granulomas and ultimately leads to increased intestinal absorption of calcium and raised serum calcium levels.
e) ACE levels (elevated in 50 % of patients)
f) ALP levels.
g) Chest - x-ray and pulmonary function test.
The chest x ray is very important and may show normal findings (stage 0) or bilateral hilar lymphadenopathy (stage 1), or lymphadenopathy with infiltrates (stage II) infiltrates alone (stage III) or fibrosis (stage IV).
h) ECG
i) Eye examination
j) PPD or Quantiferon (for TB)
What is the treatment for scalp sarcoidosis?
The treatment for scalp sarcoidosis involves a variety of potential treatments and can often be quite refractory to treatment. These include topical steroids, steroid injections, oral prednisone, hydroxychloroquine and similar immunosuppressive agents that can be used for treating systemic sarcoidosis (methotrexate, cyclosporine). Other treatments are also possible including TNF inhibitors like infliximab. Very often systemic steroids are needed.
Sarcoidosis can be life threatening for some individuals and the mortality is as high as 5-10 %. Patients with severe lung disease (stage 4 chest radiographs), fibrosis on CT, and pulmonary hypertension are more likely to die.
REFERENCE
Akhdari N, et al. Erythematous lesions on the scalp. Sarcoidosis. Arch Dermatol. 2004;140:1003–8.
Ghosh A, et al. Single lesion of sarcoidosis presenting as cicatricial alopecia: A rare report from India. Int J Trichology. 2014;6:63–6.
Katta R, et al. Sarcoidosis of the scalp: A case series and review of the literature. J Am Acad Dermatol. 2000;42:690–2.
Pellicano R et al. Dermoscopy of cutaneous sarcoidosis. Dermatology. 2010;221(1):51-4.
Starace et al. SCALP SARCOIDOSIS WITH SYSTEMIC INVOLVEMENT: A CASE REPORT AND LITERATURE REVIEW. European Medical Journal Spet 2019.
Torres F et al. Trichoscopy as a clue to the diagnosis of scalp sarcoidosis. Int J Dermatol. 2011;50(3):358-61
IMAGE REFERENCES
Long T et al. Severe scalp sarcoidosis in an unlikely patient. JAAD Case Rep . 2020 Apr 24;6(11):1165-1166.
Prohaska J et al. Scalp Sarcoidosis Presenting as Cicatricial Alopecia. J Am Osteopath Assoc . 2018 Dec 1;118(12):824-826.
Ghosh A et al. Single lesion of sarcoidosis presenting as cicatricial alopecia: a rare report from India. Int J Trichology . 2014 Apr;6(2):63-6.
House NS et al. Sarcoidosis-induced alopecia.Dermatol Online J 2012 Aug 15;18(8):4.
Roche FC et al. Sarcoidosis: An atypical mimicker of acne keloidalis nuchae. JAAD Case Rep. 2020 May; 6(5): 397–399.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.