Scalp Biopsies Lead to Scalp Biopsy Results NOT Final Diagnoses!
The Final Diagnosis of a Person’s Hair Loss is Never Reached without The Full Story and a Proper Examination!
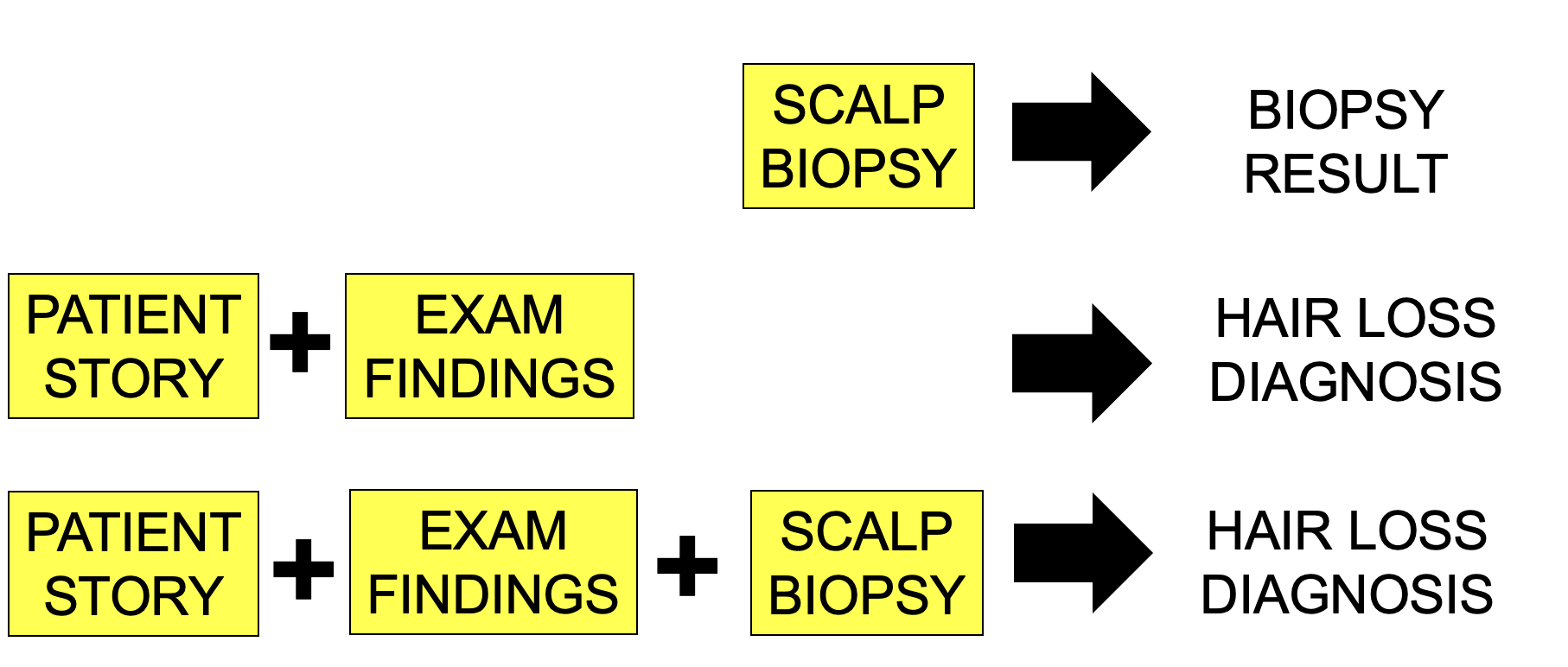
The diagnosis of hair loss always requires a careful review of a patient’s story and review of scalp findings. Sometimes a biopsy is needed to confirm suspicions that arose from listening to the patient’s story or following examination of the scalp. In the vast majority of patients with hair loss, however, a scalp biopsy is not needed and the patient’s medical history and scalp examination findings alone are sufficient to confidently render a diagnosis.
A scalp biopsy does not give a final diagnosis. Rather, a scalp biopsy gives a scalp biopsy report. It is never in and of itself a “final” clinical diagnosis.
The diagnosis always requires one to consider the story and the examination findings in context with the report.
When one gets back a biopsy result, one should not say “Oh, what is the diagnosis!?”
That is of course commonly done - but it is incorrect.
When one gets back a biopsy result one should say “Oh, I have the biopsy result back. Let me review the patient’s story again and review the examination findings and see if it fits with the information from the biopsy report”
If the biopsy result does not fit with the story or does not fit with what was seen on examination- another biopsy should be considered or a second opinion on the biopsy should be sought.
A biopsy does not generate any kind of “final diagnosis”. A biopsy generates a biopsy report. It is the history and examination and biopsy (if biopsy is even needed) that allow one to confirm the proper final diagnosis.
I receive many emails a week with biopsy results attached. The emailer asks “What do you think of my diagnosis?”
A biopsy report is not a diagnosis.
I reply by saying to the emailer “What is the story of the hair loss and what does the scalp examination show?”
A biopsy result showing lichen planopilaris is not a final diagnosis of lichen planopilaris unless it fits with the clinical history and scalp examination findings. If an experienced clinician feels this couldn’t possibly be LPP, then a repeat biopsy is needed or another opinion on the biopsy is needed.
A biopsy result showing alopecia areata is not a final diagnosis of alopecia areata unless it fits with the clinical history and scalp examination findings. If an experienced clinician feels this couldn’t possibly be alopecia areata then a repeat biopsy is needed or another opinion on the biopsy is needed.
A biopsy result showing central centrifugal cicatricial alopecia is not a final diagnosis of CCCA unless it fits with the clinical history and scalp examination findings. If an experienced clinician feels this couldn’t possibly be CCCA then a repeat biopsy is needed or another opinion on the biopsy is needed.
A biopsy result showing chronic telogen effluvium is not a final diagnosis of CTE unless it fits with the clinical history and scalp examination findings. If an experienced clinician feels this couldn’t possibly be CTE then a repeat biopsy is needed or another opinion on the biopsy is needed.
Biopsies give biopsy reports.
Biopsies, together with clinical histories and examinations, generate final diagnoses.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.