False Positive and False Negative Scalp Biopsies: Three Important Principles to Know.
Scalp Biopsies: Do they tell me everything?
Scalp biopsies are short procedures that can help the physician determine what diagnosis best fits the patents hair loss pattern. Scalp biopsies are not always needed. In fact, the vast majority of patients with hair loss don’t need to have a scalp biopsy provided a proper history is taken from the patient and a proper scalp examination is done. Some clinics do a biopsy on every single person that walks in the door - but that’s another topic altogether. Scalp biopsies are not always needed. Scalp biopsies can be helpful when the diagnosis is just not clear or the diagnosis seems clear but the patient is not responding to treatment that way that was hoped.
See Indications for a Scalp Biopsy
What kind of results can come back after the biopsy is done?
Scalp Biopsy results are usually accurate. However, the results that come back can be of three types
1. MOST COMMON - The result is accurate and shows the report generated by three pathologist is actually the diagnosis the the patient has.
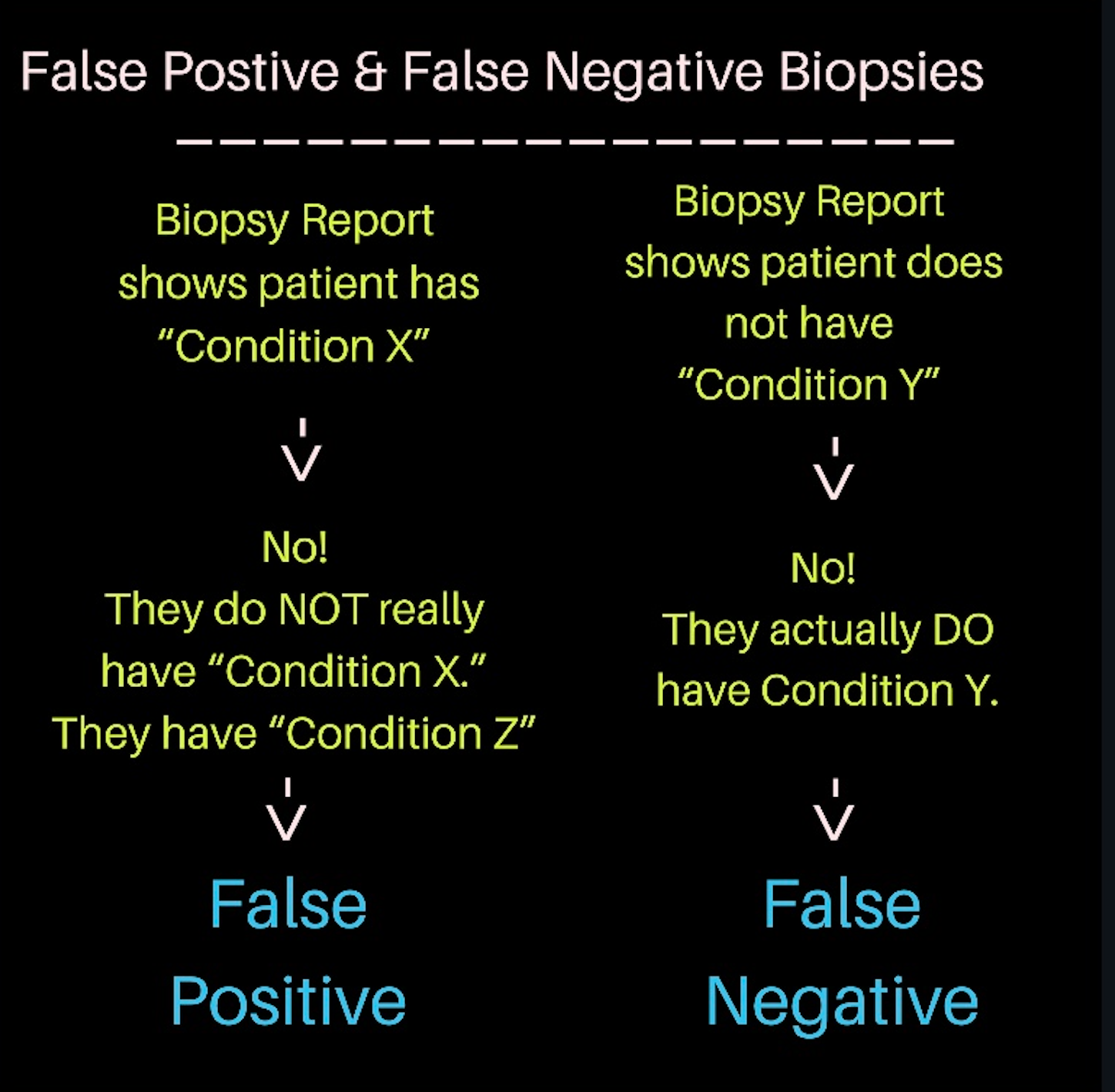
2. LESS COMMON - The result is inaccurate and shows the report generated by the pathologist is not the diagnosis the the patient has. We call this a FALSE POSITIVE.
3. LESS COMMON - The result is inaccurate and shows the report generated by the pathologist is missing thee diagnosis the the patient has. We call this a FALSE NEGATIVE.
PRINCIPLE 1: A scalp biopsy represents 0.1 % of the scalp surface. A biopsy can often tell what is happening within the tiny core of skin and from this the pathologist tries to extrapolate what is happening in the other areas of the scalp. But a biopsy has its limitations and “false positives” do exist.
Performing a scalp biopsy has three basic requirements: 1) One needs a scalp. 2) One needs a biopsy tool. 3) One needs a human being to determine where exactly to take the biopsy from. All of these three are important. The first two are rather obvious. The latter is easily forgotten.
When a biopsy result comes back the doctor must always ask himself or herself: Does this report I have in front to me represent what is happening over a larger area of the scalp? After all a scalp biopsy is just 4 mm in size with an area of 0.5 square centimetre. The total scalp is 500 to 700 square centimetres. We need to make sure that the 0.5 square centimetre sample is representative of the entire scalp!
Most of the time, they do. If the biopsy suggests androgenetic alopecia happening inside that tiny 4 mm biopsy sample, there is probably androgenetic alopecia happening over a larger area of the scalp. If the biopsy shows a higher proportion of the hairs in telogen phase, then there is likely to be some hair cycling disorder affecting the scalp (ie a diagnosis of telogen effluvium).
But biopsies are not without error. A biopsy can be interpretted as scarring alopecia when it might not actually be scarring alopecia. This occurs for example when the pathologist feels that the presence of perifollicular fibrosis alone is a sign of scarring alopecia.
Perifollicular Fibrosis in AGA: Not Necessarily a Sign of LPP
When Interpretations go Wrong: A Look at AGA vs LPP
A biopsy can be interpretted as alopecia areata when it might not actually be alopecia areata. This occurs sometimes when a pathologist feels that a high proportion of telogen and catagen hairs int he biopsy represents a diagnosis of alopecia areata.
When the pathologist gives a result that does not truly represent the diagnosis that a patient really has, we call this a ‘false positive.’
Let’s summarize “false positives” another way:
If you find a certain diagnosis in your scalp biopsy report, it probably means the patient has that diagnosis. But once you get the biopsy report back in your hands you need to review the entire history again, review the scalp examination findings again and review the blood tests again and ask yourself -does this make sense? In some cases you then need to assume it’s a right diagnosis and start treatment. After a period of a certain number of weeks of months on treatment, you then need to review the entire history again, review the past and current scalp examination findings again and review the blood tests again and ask yourself - does this all make sense? Is the patient responding to treatment like I would expect for this diagnosis? If not, there is a small chance you had a false positive biopsy and a good chance that a repeat biopsy could be helpful
PRINCIPLE 2: A scalp biopsy does not always tell a patient what diagnoses they do not have. If a certain diagnosis does not turn up in the biopsy - it means that diagnosis was not seen inside the tiny 4 mm core. That’s the main conclusion. Fortunately it “probably” means the also diagnosis won’t be found in the other 99.9 % of the scalp but that is a big assumption sometimes. There are “false negatives.”
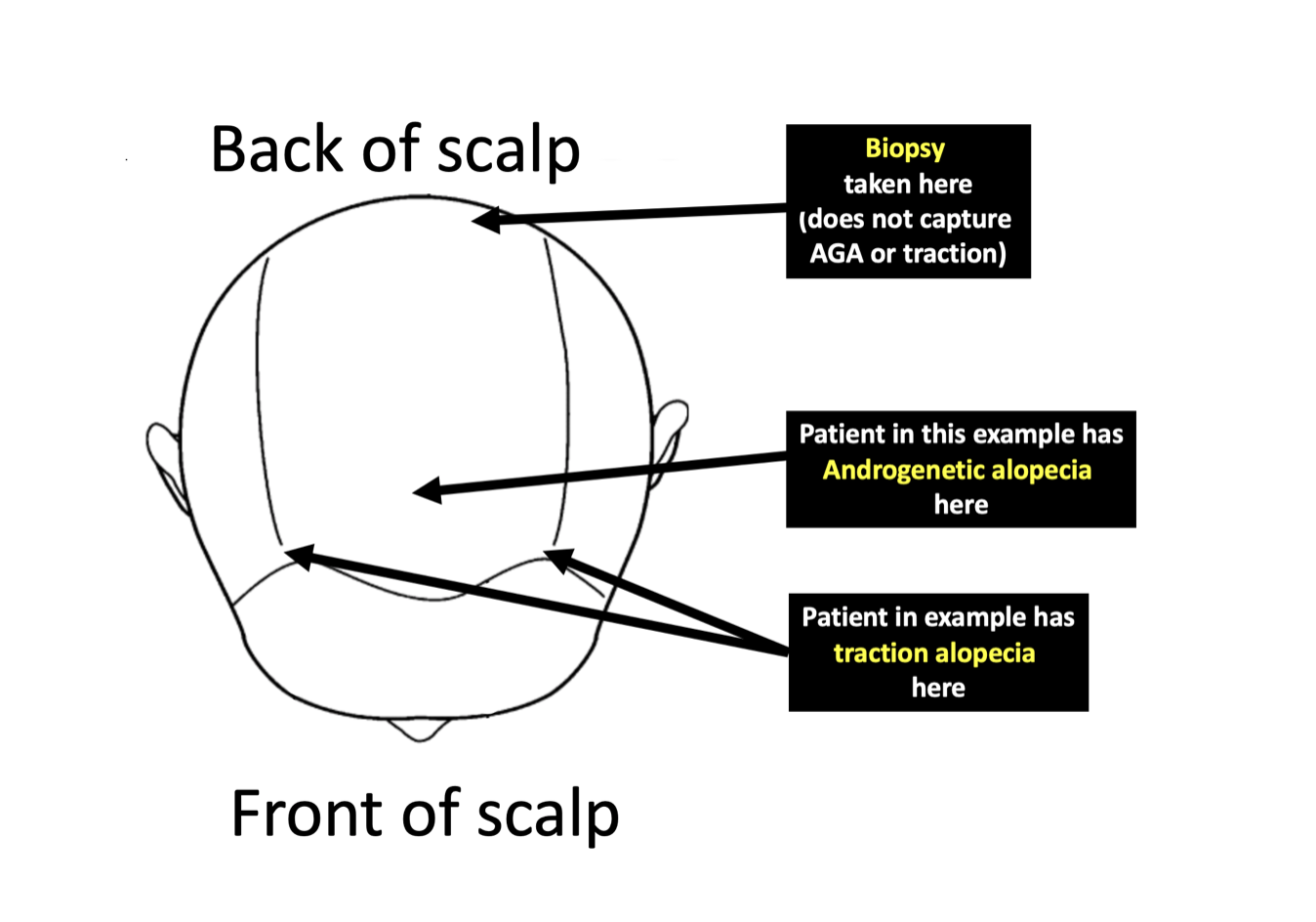
Principle 2 is important. If a biopsy returns showing that patient does not have androgenetic alopecia - it might mean the patient does not have androgenetic alopecia. But it all depends, of course, if the biopsy was taken from the right area of the scalp. If the biopsy was taken from an area of the scalp where androgenetic alopecia rarely occurs, it’s not very useful.
We discussed this in a recent article
Does a scalp biopsy capture all diagnoses a patient has?
For example, if a biopsy is taken from the back of the scalp in a patient who actually has androgenetic alopecia in the front of the scalp, one can’t conclude that the patient does not have androgenetic alopecia. The only thing that can be concluded is that there was no evidence of androgenetic alopecia in the site where the biopsy was taken from.
Let’s summarize “false negatives” another way:
If you can’t find the words “telogen effluvium” in your scalp biopsy report, it probably means the patient does not have telogen effluvium but biopsies are not so great for diagnosing TE. The clinical story and examination is better. That will require the clinician to examine the patient !
If you can’t find the words “androgenetic alopecia” in your scalp biopsy report, it probably means the patient does not have androgenetic alopecia in the area where the biopsy was taken. We have no idea if the patient has androgenetic alopecia at an area far away from that area. That will require the clinician to examine the patient !
If you can’t find the words “lichen planopilaris,” ‘frontal fibrosing alopecia”, “discoid lupus,” “folliculitis decalvans,” “central centrifugal cicatricial alopecia” or “scarring alopecia” in your scalp biopsy report, it probably means the patient does not have a scarring alopecia in the area where the biopsy was taken. We have no idea if the patient has a scarring alopecia at an area far away from that area but likely they don’t. That will require the clinician to examine the patient!
PRINCIPLE 3: A scalp biopsy is a glimpse of what’s happening on the scalp on the day the biopsy is taken. It does not tell a patient what diagnoses they may develop in the weeks, months or years ahead.
It’s usually a reason for celebration when a biopsy report comes back from the pathologist and it does not show some of the more serious or worrisome diagnoses I was wondering about. Most of the time - there’s good reason celebrate.
However, one must always remember that a biopsy is a snapshot of what’s happening on a tiny area repreresenting 0.1 % of the scalp area on the day the biopsy was taken. It’s up to the doctor who took the biopsy to figure out if the biopsy really represents the other 99.9% of the scalp surface area. It’s also up to the doctor to figure out if the result is likely to hold true for the next few weeks, months or years.
Sometimes it does not.
Let’s take a look at some examples
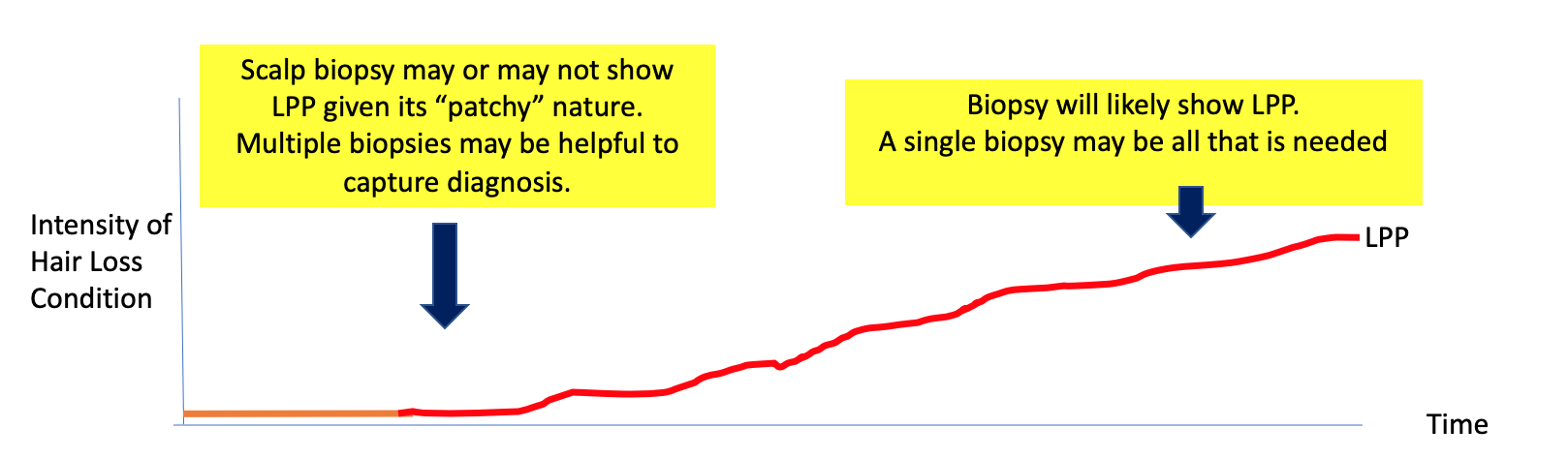
A scalp biopsy may miss a slowly evolving case of scarring alopecia.
Consider a patient who just developed new redness in the scalp, new shedding and new symptoms of itching and burning. You are really wondering about lichen planopilaris. You see some features by dermoscopy but not enough to convince you. The patient is known to have oral lichen planus which you know is very closely related to scalp LPP. You biopsy the scalp in February and do not find good evidence for LPP. You decide to rebiopsy again in August and it shows a convincing case of LPP.
Although not common, this is a case where the patchy nature of early disease can lead to a false negative biopsy. I truly believe the patient had LPP in April, but the biopsy suggested the patient did not.
The key lesson here is: if one is really convinced about a diagnosis and the biopsy returns showing otherwise - a repeat biopsy in the future could make a lot of sense.
2. A scalp biopsy may miss a slowly evolving case of androgenetic alopecia after shedding.
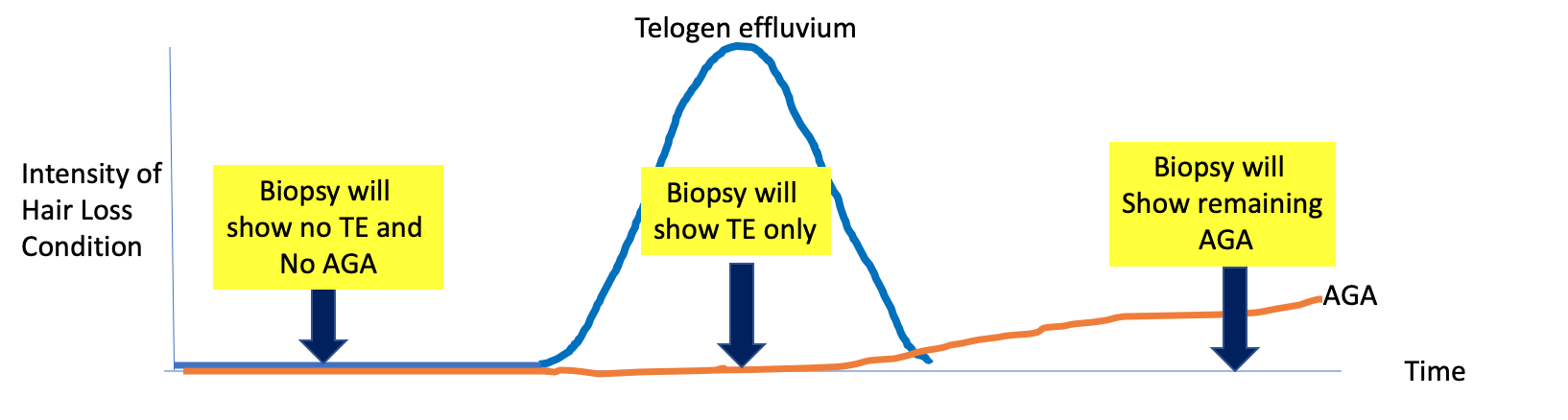
There is a situation that can sometimes develop in patients who experience shedding. It is a phenomenon whereby patients who experience shedding can sometimes find that their hair density does not return back to normal once the shedding episode is done. This is because the patient finds they are dealing with a new hair loss condition - androgenetic alopecia - once the shedding condition is gone. Hair doctors refer to this by many names including the fact that the shedding “precipitated” androgenetic alopecia or the shedding “unmasked” androgenetic alopecia. You can read more about this here.
The Sequelae of Hair Shedding: Modelling Telogen Effluvium
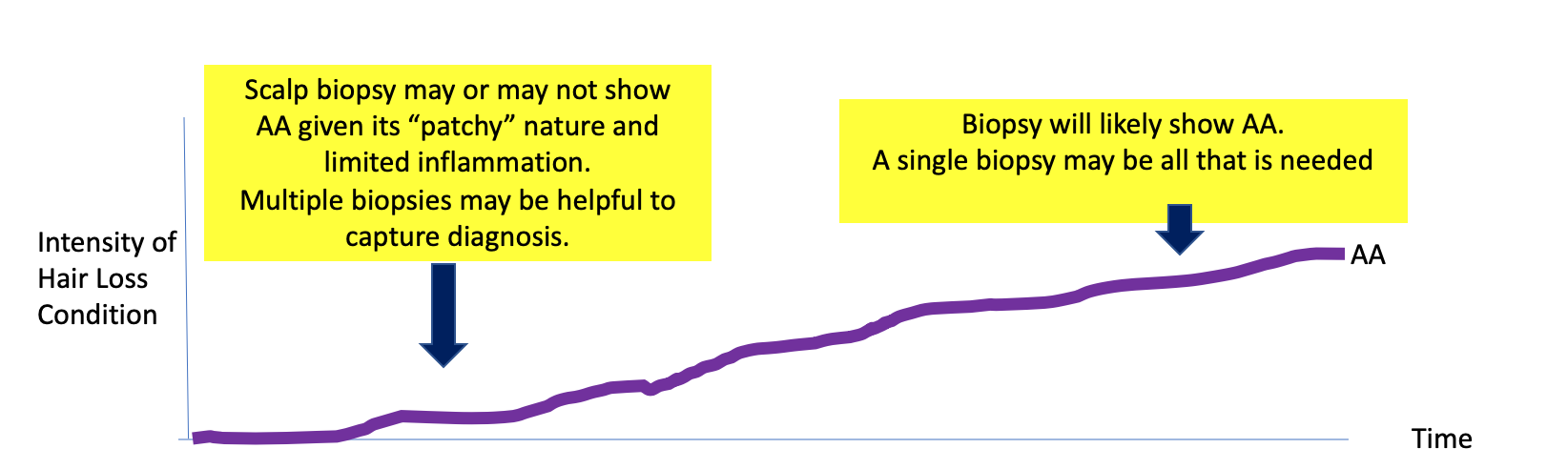
In these situations, a scalp biopsy may or may not show the androgenetic alopecia (AGA). If the biopsy is done early in the course of thee patient’s shedding experience, the biopsy may only show telogen effluvium (middle yellow rectangle in diagram below). However, over time, the biopsy will show more and more convincing evidence of androgenetic alopecia.
The key lesson here is: one must at least consider the possibility of androgenetic alopecia in a patient who does not regain their hair density after a shedding episode.
3. A scalp biopsy may miss a slowly evolving case of alopecia areata
Consider a patient who just developed new shedding. You are really wondering about diffuse alopecia areata. You see some features by dermoscopy but not enough to convince you. The patient has thyroid disease and nail pitting. Her mother has alopecia areata. You biopsy the scalp in June and do not find any good evidence for alopecia areata. You decide to rebiopsy again in August and it shows a convincing case of LPP.
This is a case where the patchy nature of early disease can lead to a “false negative” biopsy. Diffuse alopecia areata can be challenging to diagnose sometimes - and a biopsy must not dissuade you from treating for AA if you truly think this is what the patient has.
The key lesson here is: if one is really convinced about a diagnosis and the biopsy returns showing otherwise - a repeat biopsy in the future could make a lot of sense.
Summary
In summary, scalp biopsies are a not only a snapshot of one area of the scalp but also a snapshot of what is happening in that area on the day the biopsy was taken.. It’s up to the doctor who did the biopsy to figure out if the results that come back truly make sense and if they truly represent what could be happening in other areas of the scalp. If a certain result does not show up in the biopsy report, it likely means the diagnosis is not present but there are plenty of exceptions. Finally, one must always keep in mind that some hair loss conditions are evolving and if they are not present on scalp to any significant degree on the day the biopsy was taken, they could potentially be present on the scalp in the weeks, months or years ahead.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.