In defence of the scalp biopsy: Reliable or not?
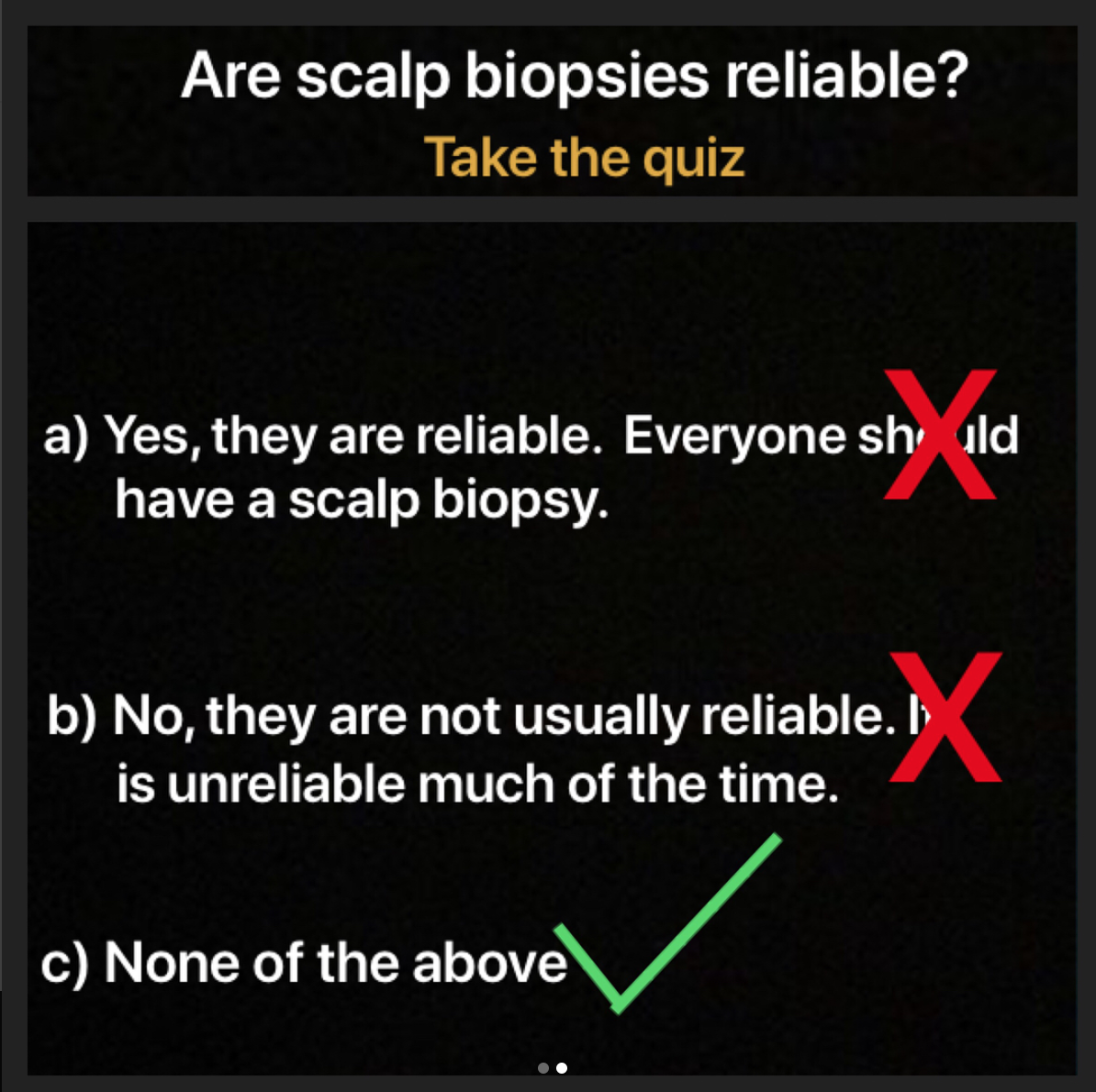
Are scalp biopsies accurate and reliable?
I’m increasingly asked if scalp biopsies are reliable. I don’t know why or how it has happened but somewhere and somehow out there in the great and vast entity known as the internet there has come to be a pervasive view that scalp biopsies are not so helpful and not so reliable. To some degree it almost seems that this view has now overtaken the polar and equally incorrect view that scalp biopsies are the “final answer” to all hair loss problems and everyone should have a scalp biopsy. Both of these extreme views are wrong and I’d like to give some clarity to the issue.
Reliable scalp biopsies are generally reliable
Scalp biopsies have the highest chance of being helpful if they are
1. Taken from the correct area of the scalp
2. Use of both vertical and horizontal sections is considered
3. The biopsy is interpreted by an expert dermatopathologist.
One often runs into problems in interpreting biopsies when:
1. The sample was taken from the wrong area on the scalp
2. The sample was not the correct size (i.e. not 4 mm punch)
3. The sample was sent for vertical sectioning only
4. The sample was sent “anywhere” for analysis
5. The sample was read by a pathologist with less familiarity in hair and scalp pathology.
Examples
Here are some examples. To protect privacy, these examples are all fictional but certainly match up pretty close to countless numbers of patients seen over the years. They illustrate important points.
Example 1.
An 50 year old woman with classic frontal fibrosing alopecia is seen in the office. She lost her eyebrows at age 46 followed by arms, leg and pubic hair. She has now has lost her frontal hairline. The dermatologist wishes to take a biopsy but is worried about scarring and leaving a permanent scar on the scalp. On account of this a biopsy is taken 1 cm back from the hairline. The biopsy is obtained with good technique and is proper size (4 mm). It is sent off to a world expert dermatopathologist. The pathological interpretation is “androgenetic alopecia with no evidence of frontal fibrosing alopecia.”
Take a look at the (hypothetical) report if her biopsy was taken from an area of redness and scale from the frontal hairline or side temple. The dermatologist took it from this site after explaining it was the best site but also explaining it could cause a permanent scar. The final pathological interpretation is “androgenetic alopecia with evidence of frontal fibrosing alopecia.”
Same patient. Same dermatologist. Same pathologist. Different site. Different diagnosis.
Surprised?
Don’t be. Biopsies are important but they need to be taken from the right spot. Are biospies accurate? Yes, fairly accurate if the right steps are taken from start to finish. Reliable biopsies are, in fact, fairly reliable. The above is a common scenario. Does this first biopsy mean the patient does not have FFA? Of course not. The biopsy means that the area where the biopsy was taken from does not contain FFA.
As physicians we wish to limit side effects where possible. In fact, one of the oaths of our profession itself is to “do no harm.” We often want to take a biopsy from an area that will be hidden and from an area where a long term scar will be less visible. This is important to consider but if the site of the biopsy jeopardizes receiving proper interpretation of the patient’s condition, another spot should be chosen (or one should not do the biopsy).
Example 2.
A 33 year old male with classic male balding and seborrheic dermatitis comes to the office. His history includes anxiety and severe depression. His scalp is burning and he has itching from time to time. It sometimes even feels sore. The patient has read alot and wonders about the possibility of having a scarring alopecia. “Doctor, I have researched everything and I am certain I have lichen planopilaris.” The patient really wants a biopsy. The dermatologist says that he does not think it is a scarring alopecia but agrees to do a biopsy. The biopsy is taken from two areas - one for horizontal sections and one for vertical sections. It is sent off to a local clinic that knows where to send the result for pathology. It is read by a pathologist who is well respected for general knowledge in pathology. The biopsy report appears as follows:
4 mm samples submitted by Dr Carver with a note to “rule out scarring alopecia in this patient with severe itching burning and pain.” The biopsies are excellent. There is some miniaturization of hairs noted. There is a lymphocytic infiltrate in the upper dermis with perifollicular fibrosis noted. The findings are consistent with possible lichen planopilaris with coexistent androgenetic alopecia.”
This example above is all too common. The man in the example leaves the clinic with a diagnosis of scarring alopecia when in fact he does not have scarring alopecia. The man in the example now must cope with the diagnosis which further adds to his anxiety. Does he have lichen planopilaris? Well not in this example.
Take a look at the (hypothetical) report if his biopsy was sent to an expert dermatopathologist. This pathologist reads and interprets alot of scalp biopsies.
4 mm samples submitted by Dr Carver with a note to “rule out scarring alopecia in this patient with severe itching burning and pain.” The biopsies are excellent. There is some miniaturization of hairs noted. The terminal to vellus ratio is 2.8 to 1. There are 12 % telogen hairs noted. There is a lymphocytic infiltrate in the upper dermis with perifollicular fibrosis noted. However, there is no lichenoid change of the follicular epithelium and no necrosis. The epidermis is normal. Sebaceous glands are preserved and appear enlarged. The findings are consistent with androgenetic alopecia with no evidence of lichen planopilaris or scarring alopecia.”
Surprised?
Same patient. Same biopsy. Different pathologist. Different result. Are biospies accurate? Yes, fairly accurate if performed properly. Again, reliable biopsies are fairly reliable.
Example 3.
A 65 year old female with chronic shedding due to chronic telogen effluvium (CTE) comes in for an evaluation. In this example, her dermatologist suspects CTE but is not sure if it’s androgenetic alopecia. He’s confident it’s not a scarring alopecia but does a biopsy and submits it to the pathology lab for vertical sectioning. The pathologist’s report returns as follows.
The biopsy is an excellent biopsy extending to the subcutis. There is a decreased number of hairs. Sebaceous glands and preserved but not overly prominent. There is no inflammation around the bulb to suggest alopecia areata and no evidence of scarring alopecia. The epidermis is normal. The findings are consistent with a non scarring alopecia and clinic correlation is needed to distinguish entities such as androgenetic alopecia and chronic telogen effluvium.
Here, the clinician and patient remain confused. The biopsy did not help.
Now consider the same 65 year old female but now when the dermatologist does a biopsy he does 2 samples of 4 mm size and submits it to the pathology lab for horizontal sectioning with the comment “please assess for CTE.” The pathologist’s report returns as follows.
"The biopsies are excellent biopsies and both extend to the subcutis. There are 37 hair follicles seen in the first biopsy with 17 % telogen hairs. 33 are terminal and 4 are vellus hairs. The terminal to vellus ratio is 8.25:1. Sebaceous glands and preserved but not overly prominent. There is no inflammation around the bulb to suggest alopecia areata and no evidence of scarring alopecia. The epidermis is normal. The second biopsy is similar with T:V ratios of 8.7:1. The findings are consistent with chronic telogen effluvium"
Surprised?
Same patient. Same pathologist. Different method of processing the sample. Different result. Are biospies accurate? Yes, fairly accurate if performed properly from A to Z. Reliable biopsies are fairly reliable.
Conclusion and Answers
The correct answer to the quiz is c. Option “a” is not correct. Scalp biopsies are not needed in everyone and really one needed if the diagnosis is in question or one os trying to decided between two diagnoses. Option “b” is also not correct. As we have seen in the post, reliable biopsies are actual fairly reliable. One can distinguish easily scarring from non scarring and determine of androgenetic alopecia is present much of the time if horizontal sections are used. One can often get a sense of telogen effluvium but the actual cause can’t be determined by biopsy (low iron, thyroid problem etc). That’s a clinical diagnosis- not a pathological one.
The scalp biopsy can be very helpful but only if all the proper steps are taken including proper site, proper technique. It should never be forgotten that the dermatopathologist can also make a difference especially in more challenging cases. Hair and scalp dermatology can be challenging- and hair and scalp pathology can also be challenging. If all the proper steps are taken, the chances increase greatly that challenging cases can be ... solved.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.