The Diagnosis and Treatment of Scalp Seborrheic Dermatitis: A Brief Overview
The Treatment of Scalp Seborrheic Dermatitis (SD)
Seborrheic dermatitis of the scalp is common. About 5 % of the world has seborrheic dermatitis. Some patients with SD are completely asymptomatic but some have scalp itching, burning, redness, greasiness and irritation. Some patients are concerned not only about the seborrheic dermatitis they have on their scalp but the seborrheic dermatitis on the nose, eyebrows, chest, and other parts of the body too.
Seborrheic dermatitis impacts patient’s quality of life, so addressing it properly and treating it effectively is a really important goal. I see seborrheic dermatitis of the scalp every single working day. Patients with some scalp conditions, like scarring alopecia, may be at increased risk of seborrheic dermatitis compared to the general population.
What is the cause of seborrheic dermatitis?
The cause of seborrheic dermatitis is complex and still not perfectly worked out. That said, we know quite a bit about the condition thanks for several decades of productive research. It appears that a fundamental issue in seborrheic dermatitis is impaired skin barrier function that allows Malassezia yeast to happily proliferate in the skin. It’s still open to some debate as to whether Malassezia contribute to the disrupted barrier function or whether the disrupted barrier function facilitates Malassezia to proliferate. Nevertheless, seborrheic dermatitis has several features that scientists are carefully researching a) the impaired skin barrier function b) the proliferation of Malassezia c) the change in other components of the scalp microbiome including reduction in bacteria such as Cutibacterium acnes and increased in Staphylococci and Streptococci and d) a plethora of inflammatory changes happening in and on the scalp and e) the abnormal immune response that happens against Malassezia.
The last comment - the abnormal immune response - is important to consider. There is so much more to seborrheic dermatitis than just Malassezia proliferating too much. Certain Malassezia species are very prevalent on the human scalp but yet not everyone gets SD.
We still have a bit more to learn about this common condition.
A Closer Look at the Role of Malassezia in SD
To be human, means to live in harmony with Malassezia. It is the most prevalent fungus in healthy human skin. Anywhere between 30 % to 100 % of newborn babies already have Malassezia living on the skin from day 1.
Malassezia are clearly involved in the pathogenesis of SD. Certain Malassezia species increase dramatically in seborrheic dermatitis. Treatment to eradicate the Malassezia correlates well with a reduction in the seborrheic dermatitis. M sympodialis, M restricta and M globosa are all contributors to SD.
Malassezia have a major problem that makes their life challenging. They lack an enzyme known as fatty acid synthase so they can’t make their own lipids! They can’t make their own fatty acids. This means they need to live close to areas of the body rich in oil glands. The Malassezia secrete enzymes (lipases and phospholipases) that help break down fats from the human skin and give them all the fatty acids they need to survive. That’s the main reason why seborrheic dermatitis happens in areas rich in oil glands.
Who gets seborrheic dermatitis? …. A Closer Look at the “Risk Factors.
5-10 % of the world will experience seborrheic dermatitis. An astounding 50 % of the world will also experience a very closely related condition called “dandruff”. I often tell my own patients that dandruff and seborrheic dermatitis are like cousins. They have a whole lot in common, including the role of Malassezia yeast. When the scalp is red and more inflamed, we tend to use the term “seborrheic dermatitis.” When the scalp is not inflamed but has scale and flaking, we tend to use the term dandruff. Dandruff tends to be limited to just the scalp whereas seborrheic dermatitis may affect many areas of the body .
The Risk Factors for Seborrheic Dermatitis
Over the years, researchers have identified several risk factors for seborrheic dermatitis, including:
Neurological diseases like Parkinson’s disease, Tardive dyskinesia
Age
Males (slightly more commonly than females)
Depression and Anxiety
Darker Skin Types
Altitude
Lower temperature Climate (Fall/winter more than summer)
High humidity weather
Medications (lithium, griseofulvin, buspiridone, cimetidine, and others)
Stress
Sleep deprivation
Immunocompromised states
Diet (Western diets promote SD)
HIV
Lymphomas
Excessive Alcohol Use
What does scalp seborrheic dermatitis look like?
Patients with scalp seborrheic dermatitis present with a red scalp with yellow or greasy yellow - white scale. There can, of course, be features of dandruff present on the scalp as the two conditions are really viewed as a spectrum. Patients often have itching and sometimes burning. The scalp is oily and some patients feel obligated to shampoo every day in order to combat the excessive oiliness.
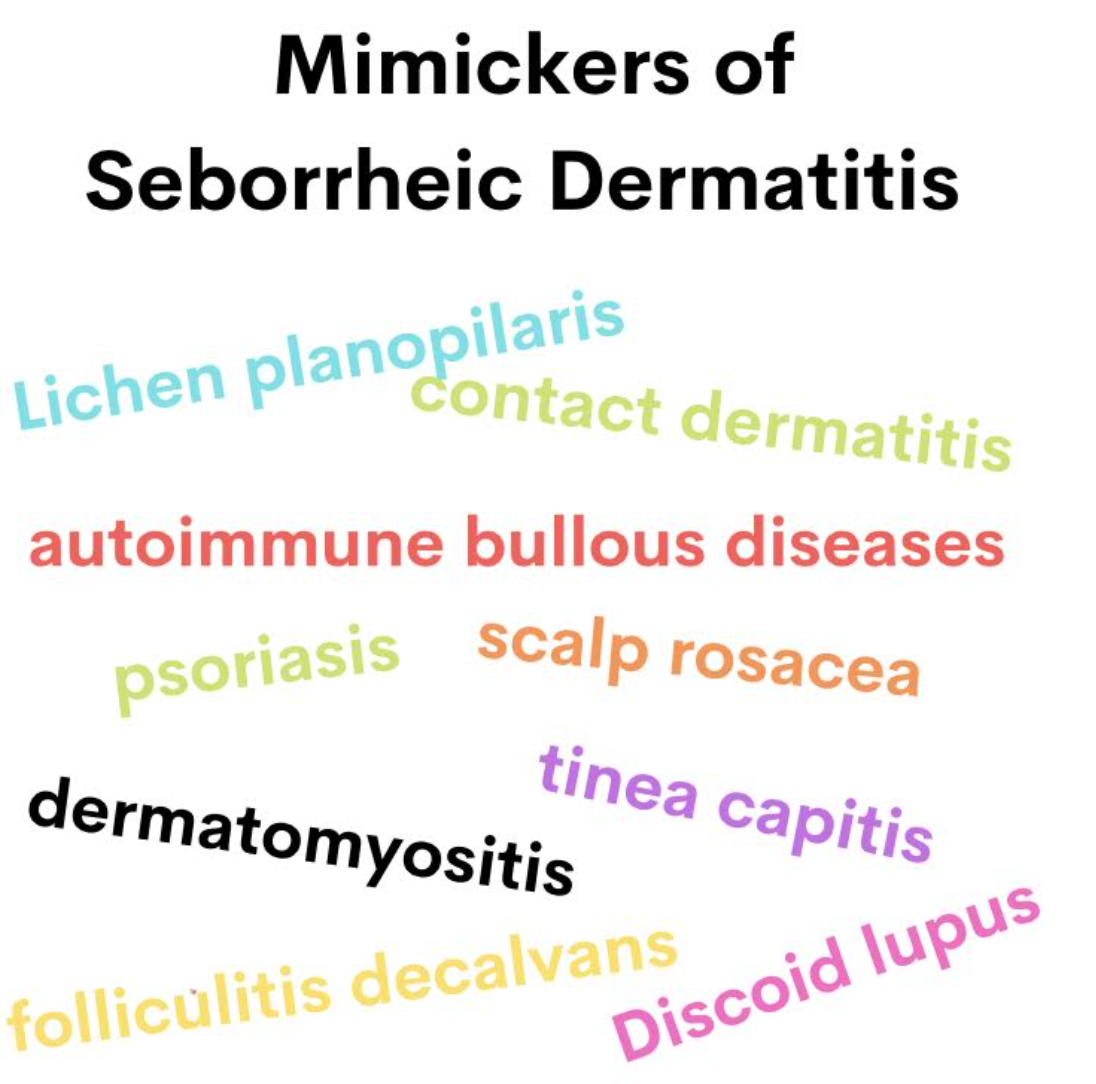
What conditions can “mimic” seborrheic dermatitis?
Anyone who treats seborrheic dermatitis needs to have a health respect for the multitude of scalp conditions that can sometimes mimic seborrheic dermatitis. It is often possible to diagnosis seborrheic dermatitis following a good history and careful examination of the scalp (including trichoscopy). Sometimes, however, it is challenging and many conditions can take on the same red scaly appearance that seborrheic dermatitis gives.
Conditions that can closely resemble seborrheic dermatitis include lichen planopilaris (LPP), discoid lupus, folliculitis decalvans, contact dermatitis, psoriasis, scalp rosacea, tinea capitis, dermatomyositis and autoimmune bullous diseases.
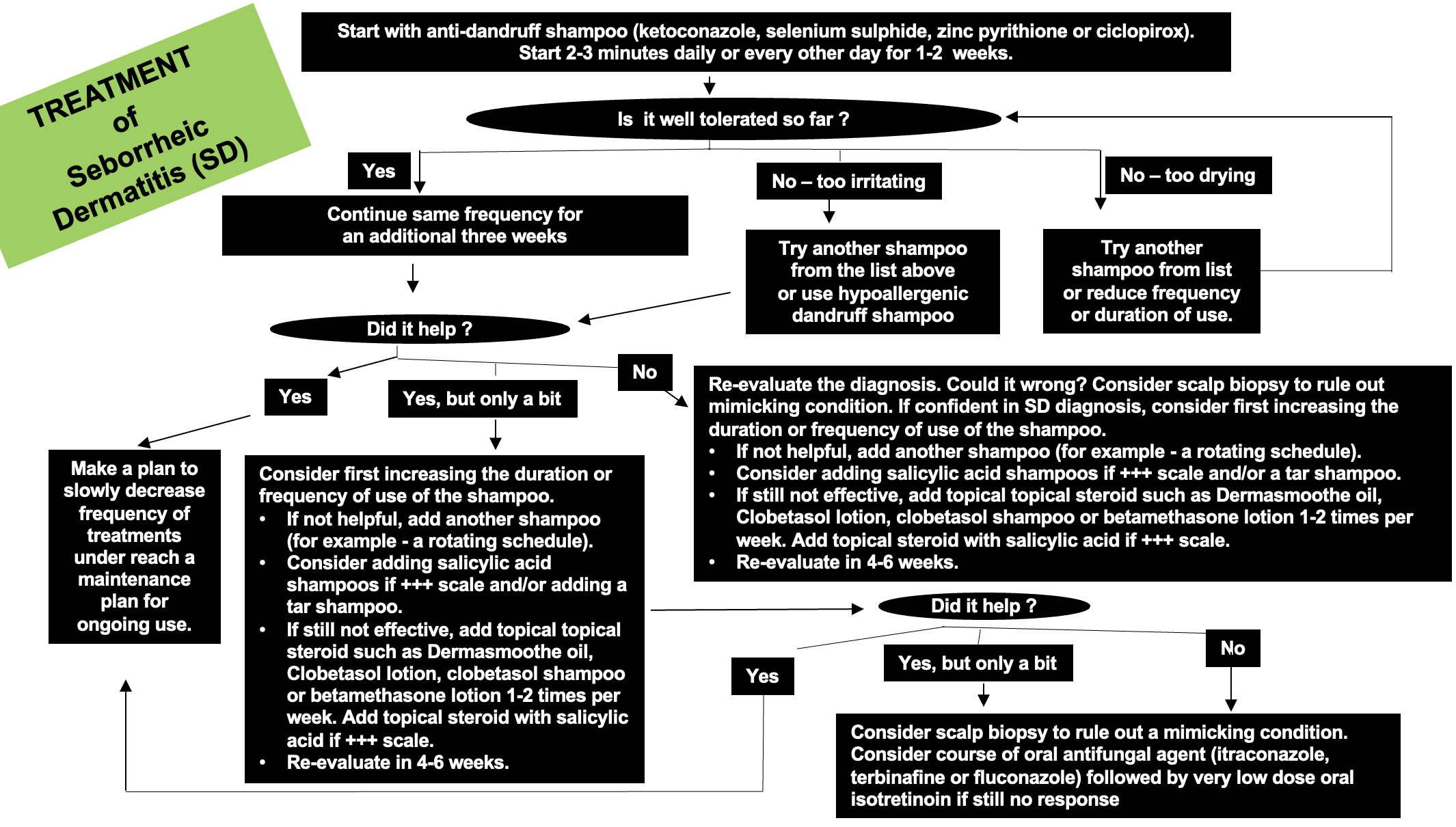
Treatment of Seborrheic Dermatitis
Treatment of seborrheic dermatitis begins with addressing any of the modifiable risk factors (if possible).
Thereafter, treatment begins with use of various antidandruff shampoos with application to the scalp for 2-3 minutes. These can be used initially daily or every other day. If the shampoo is well tolerated after 1 or 2 weeks, the shampoos can be left on the scalp for longer periods ( up to 3 to 5 minutes daily). If a patient finds a given shampoo too irritating or too drying, it would be important to consider switching the shampoo.
Patients with afro-texture hair find daily shampooing too drying. In my patients with afro-texture hair I often use zinc pyrithione based shampoos once or twice weekly and rely on periodic use of fluocinolone acetonide scalp oil (DermaSmoothe oil) to help reduce inflammation.
If the shampoo is helping considerably, one may decrease the frequency of use after the first month. Because seborrheic dermatitis is a chronic condition, the shampoos are not usually stopped completely but rather reduced in their frequency and duration of use. For example, patients who are really stable might reduce to using the shampoo once every 5-10 days.
If the shampoo is not helping as much as hoped for, the frequency and duration can be increased. In addition, I am a big fan or rotating shampoos if needed - so sometimes two or even three anti-dandruff shampoos can be brought on board. Some of my patients use ketoconazole on Monday, selenium sulphide on Wednesday and zinc pyrithione on Fridays. If itching, burning, redness and scale and not subsiding, salicylic shampoos can be used as well as topical corticosteroids.
If the treatment does not seem to really be helping at all, one needs to consider whether or not the diagnosis is correct!!! I’ve reviewed some of the famous potential mimickers of seborrheic dermatitis above. These always need to be considered. Not all seborrheic dermatitis is easy to treat but if a patient doesn’t really seem to be making any improvement one need to have a low threshold for performing one or two scalp biopsies.
For cases of refractory seborrheic dermatitis, use of oral antifungal agents (oral itraconazole, oral terbinafine) or very low doses of oral isotretinoin can be considered.
Algorithmic Approach to Treating Seborrheic Dermatitis.
Below I’ve included a helpful approach to treating seborrheic dermatitis.
Download Figure - “Approach to SD Treatment “
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.