Spinal Disease in Dissecting Cellulitis (DSC)
Dissecting cellulitis (DSC) is an inflammatory scalp disease. It may lead to scarring alopecia.
DCS may occur as an isolated entity. However a proportion of patients - perhaps 25-33 % of patients - have other coexisting inflammatory issues. These include hidradenitis suppurativa (HS) acne conglobata (AC) nand pilonidal cysts. This full tetrad is referred to as the “follicular occlusion tetrad,” and suggests a common underlying pathogenic mechanism. Although the exact mechanism is not clear, it is proposed that abnormalities in keratinization, follicular occlusion, and accumulation of cellular debris, follicular rupture, and recurrent secondary bacterial infection are associated with the condition.
Spinal Disease in DSC
There have been prior reports of patients with DSC having inflammatory spinal disease. The association of seronegative peripheral and/or axial spondyloarthritis in patients with HS and/or AC is well established. How commonly this occurs in DSC is not know but it’s likely underreported.
Spondyloarthropathy is rare autoimmune disease with a prevalence of 0.1–1.4%. The occurrence of spondyloarthropathy in patients with either isolated or combined DCS is likely underrecognized by clinician.
What are Spondyloarthropathies?
The spondyloarthropathies (SpA) are a group of inflammatory arthritis conditions that often affect the axial skeleton and have a vareity of systemic features including involvement of the peripheral joints (arthritis), enthesitis, uveitis, bowel disease. SpA consists of many entities including ankylosing spondylitis (AS), reactive arthritis, arthritis/spondylitis associated with psoriasis (PsA) and arthritis/spondylitis associated with inflammatory bowel diseases (IBD). The association with human leukocyte antigen (HLA)-B27, peripheral joint involvement predominantly of the lower extremities, sacroiliitis, spondylitis, enthesitis, dactylitis, uveitis, enteric mucosal lesions and skin lesions are the shared manifestations of the disease
Ward et al 2022
Authors of a new report present a 33 year old male with dissecting cellulitis who also developed pain in his fingers, elbows, knees, ankles, heels and feet. X rays of his hands showed erosive changes in the left fifth PIP joints and MRI showed sarcoiliitis.
He was started on methotrexate but ultimately stopped due to worry about side effects. He was recommended to start TNF inhibitor but again declined.
12 Cases in the Literature of DSC associated Spondyoarthrophy
What makes this report interesting is the fact the authors dove into the medical literature to try to identify all cases of DSC associated with spondyloarthropathy. They found 12 patients including 1 female and 11 male patients. All patients were of African American or Afro-Carribean ancestry. 9 of the 12 patients had the follicular occlusion triad (HS, DSC and AC). 2 had isolated DSC only. 1 had DSC with ankylosing spondylitis. 11 patients had peripheral inflammatory arthritis and 1 had axial only disease. In all cases, the scalp lesions preceded the onset of spinal disease by 1.5 to over 10 years.
8 of the patients in the series had symptomatic disease with pain, stiffness and limited range of motion of the cervical or lumbar spine. One had achilles tendinitis and one had arthritis of the acromioclavicular joint and sternoclavicular joint. None of the 12 patients in the literature had psoriasis, uveitis, inflammatory bowel disease or psoriasis.
Conclusion and Comment
This is an interesting report that reminds us to ask about spondyloarthropathy in our DSC patients. Spondyloarthropathy can develop even in patients who do not have HS or AC. We need to ask about spinal disease in our DSC patients at the time of diagnosis but also in follow up.
If SpA is suspected, referral to a rheumatologist is advised. In many cases, magnetic resonance imaging (MRI) will be ordered to visualize active inflammation at sacroiliac joints and spine.
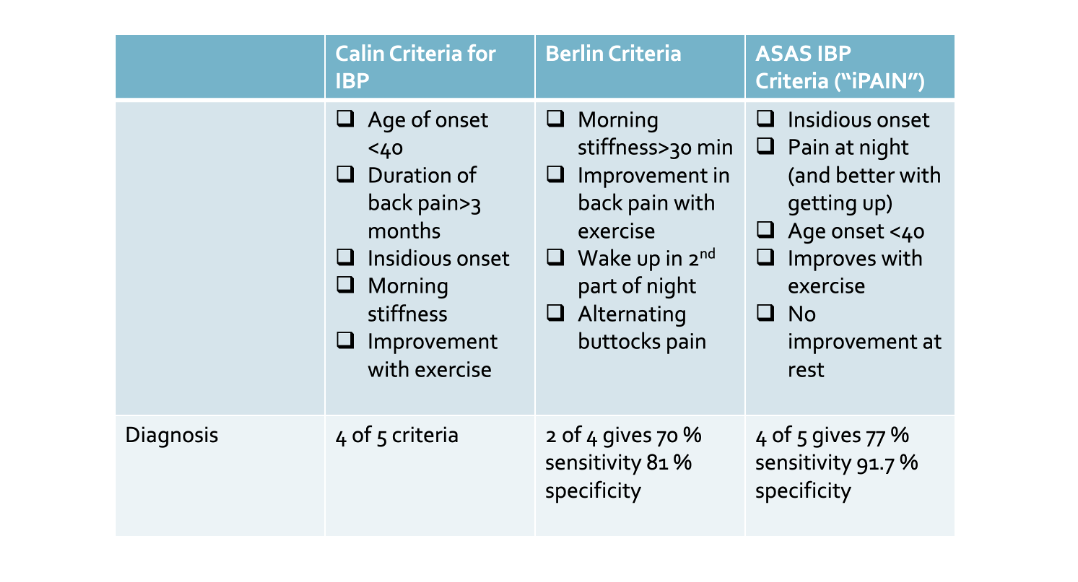
A variety of simple questions can help the hair specialist get a sense of whether or not there truly might be a concern. First, it’s helpful to understand some of the basic features of inflammatory back pain which is so common in patients with axial spondyloarthropathy. Patients (typically under 40 years of age) have back pain for more than 3 months and it gets better with exercise and does not improve with rest. There is associated morning stiffness. These are really helpful criteria. Pain that gets getter with exercise and is worse at night and prompts patients to get up is very concerning for inflammatory back pain.
Various criteria for inflammatory back pain. From : Ozgur Akgul and Salih Ozgocmen Classification criteria for spondyloarthropathies. World J Orthop. 2011 Dec 18; 2(12): 107–115.
Asking Patients About SpA Features
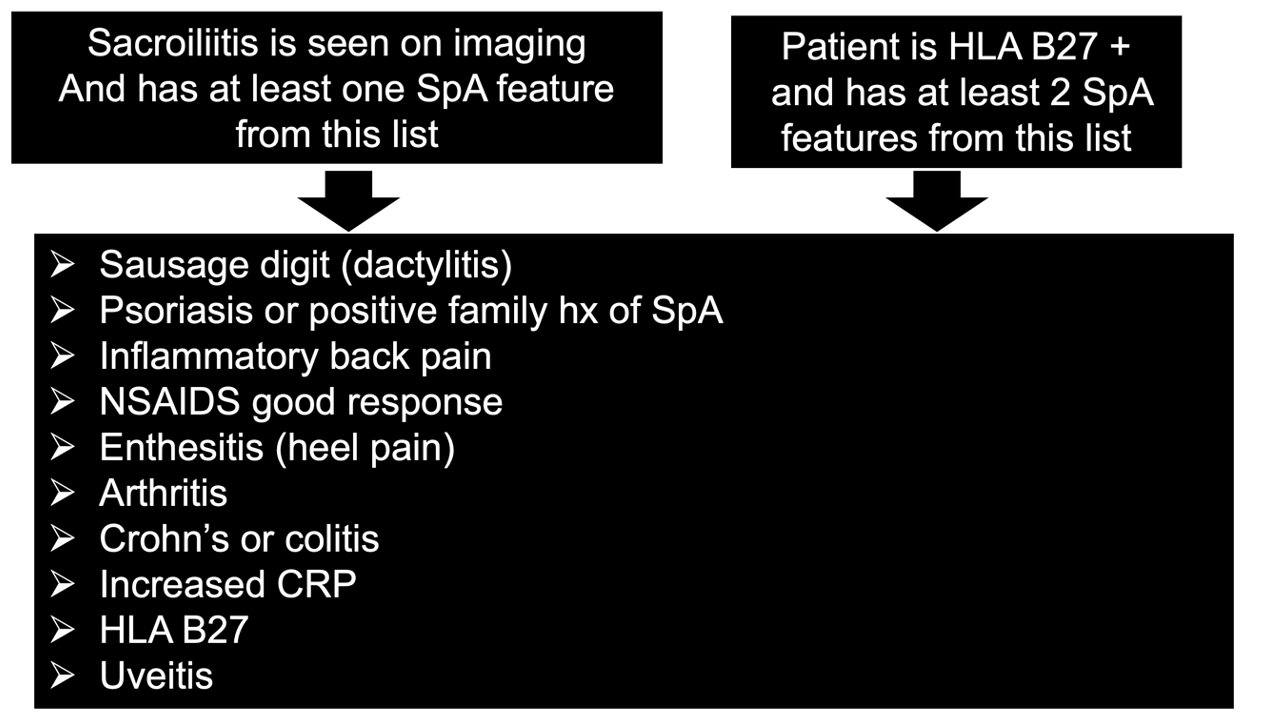
In addition to being able to identifhy inflammatory back pain, it’s helpful to know what kind of questions to ask a patient that might increase the likelihood that they have SpA and perhaps need rheumatology referral. The “Assessment in SpondyloArthritis international Society classification criteria (ASAS Criteria)” are helpful criteria which highlight when SpA might in fact be present. Typcially in my patients with inflammatory back pain, I will order HLA B27, ESR, CRP and send a referral off to the rheumatologist. About 10% of the unaffected population has HLA B27 positive results. However, that number risks to 70% in SpA patients and 70-95 % in patients with ankylosing spondylitis. I don’t typically order an MRI as I wait for the rheumatologist to order and have read by an MSK radiologist they trust. Having an MRI done and improperly interpreted sometimes does more harm than good.
Assessment in SpondyloArthritis international Society classification criteria (ASAS Criteria)
ASAS Criteria From : Ozgur Akgul and Salih Ozgocmen Classification criteria for spondyloarthropathies. World J Orthop. 2011 Dec 18; 2(12): 107–115.
Amor criteria
The Amor criteria is a helpful set or criteria for identifying spondyloarthropathy and directing questions. A score of 6 or more suggests spondyloarthropathy. These questions are helping as they too guide questioning.
Do you have lower or upper back pain at night or do you have lower or upper back stiffness in the morning
(1 point) ?
Is there buttocks pain (1 point) ?
Is there alternate buttocks pain (2 points) ?
Is there a sausage digit or toe (2 points) ?
Is there heel pain or some type of esthesopathy (2 points) ?
Is there an iritis (1 point) ?
Was there a non gonococcal urethritis or cervicitis within 1 month of onset of arthritis(1 point) ?
Is there diarrhea within 1 month of onset of arthritis (1 point) ?
Is there a history of psoriasis or IBD (2 point) ?
Is there a positive HLA B27 or is there a family history of AS, RA, uveitis, psoriasis or IBD (2 points) ?
Is there an improvement with NSAIDs (2 point) ?
Is there an asymmetrical oligoarthritis on examination? (2 points) ?
Does imaging show grade 2 bilateral of grade 3 unilateral sacroilitis (3 points) ?
REFERENCE
Ward N et al. Dissecting cellulitis of the scalp associated with peripheral and axial spondyloarthritis: report of a case and review of the literature. Clin Rheumatol 2022 Apr 23.
Devis Benfaremo et al. Multicenter Validation of the DETAIL Questionnaire for the Screening of Spondyloarthritis in Patients With Inflammatory Bowel Diseases. Study Group. The Journal of Rheumatology February 2021, 48 (2) 179-187; DOI: https://doi.org/10.3899/jrheum.200364
Ozgur Akgul and Salih Ozgocmen Classification criteria for spondyloarthropathies. World J Orthop. 2011 Dec 18; 2(12): 107–115.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.