Top 25 Things to Remember About Diagnosing and Treatment Tinea Capitis in Children.
Key Points About Tinea Capitis in Children.
Here are 25 of the most important things the practitioners should know about diagnosing and treating tinea capitis in children.
Download PDF - Tinea Capitis in Children: Key Points for Practitioners
1. Tinea capitis is a contagious fungal infection of the hair that affects 0.5% to 18 % of children.
The actual percentage of children affected by tinea capitis differs in different parts of the world. The actual number to therefore quote will depend on the country that one is referring and even the precise area of any given city where one lives.
2. The most common ages for children to be affected are ages 3-10.
Tinea capitis is uncommon before age 2 and uncommon after puberty. It can, of course, occur. Most children we see are between 4 and 8.
3. Tinea capitis is uncommon after puberty and in adults.
Tinea capitis can certainly occur in healthy adults. But it’s rare. When tinea capitis does occur in adults, we need to carefully consider whether the adults has an immunocompromised states. Not every adult with tinea capitis is immunocompromised but it is important to consider - and rule out.
4. Trichophyton and Microsporum fungal genera are the two most common causes of tinea capitis.
Of the three fungal dermatophyte genera - Trichophyton, Microsporum and Epidermophyton - most tinea capitis is due to Trichophyton and Microsporum genera infections.
5. The most common species that causes tinea capitis will vary from country to country. T. tonsurans is the most common species in North America and UK. M. canis is the most common in central Europe and Australia.
The exact species that is most common will differ from country to country. It is important for practitioners to know the tinea capitis species that are most likely in their country as this will affect the medications used for treatment.
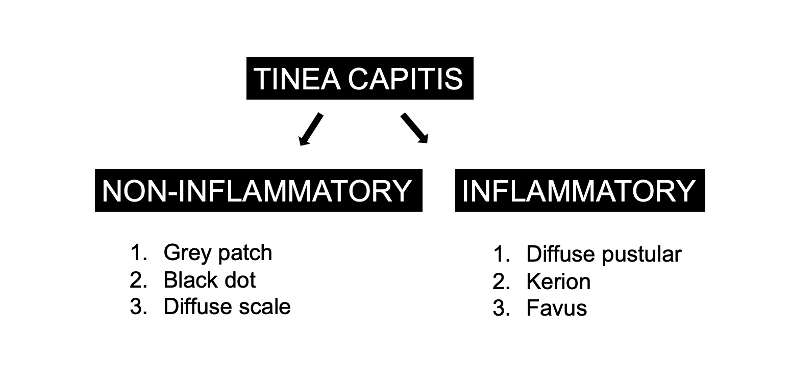
6. Tinea capitis has many different clinical presentations including non-inflammatory forms (grey patch, black dot and diffuse scaling) and inflammatory forms (kerion, pustular, favus).
There are many ways that tinea capitis shows up on the scalp and not all children’s scalps look the same when they have a diagnosis of tinea capitis. I say to doctors that if you are thinking of a certain picture of tinea capitis to burn in the back of your brain storage system so you can remember forever, you are going to be fooled because tinea capitis has many forms! The “non-inflammatory” forms of tinea capitis can look very unconcerning in the early stages. Some forms even resemble seborrheic dermatitis, dandruff, psoriasis or alopecia areata and therefore are often not recognized and properly diagnosed in the early stages. The inflammatory forms may cause a red and swollen scalp and may even cause permanent scarring hair loss. It’s not uncommon for children with more inflammatory forms of tinea capitis to have enlarged lymph nodes or ‘lymphadenopathy.’
7. The diagnosis of tinea capitis is best achieved by using all the known clinical tools to reach the diagnosis including history and clinical examination skills, trichoscopy findings, KOH examination under the microscope, Wood’s lamp and culture. All patients with suspected tinea capitis should have a fungal culture done.
There are many techniques to assess for possible tinea capitis. All have their unique benefits and limitations. If possible, a sample scraping should always be taken and send to the lab. History and clinical examination skills, trichoscopy findings, and KOH examination are wonderful methods to suggest the diagnosis but they do not give the precise species that is causing the condition.
8. Trichoscopy is extremely helpful for diagnosing tinea capitis. Findings such as comma hairs, corkscrew hairs, zigzag hairs, bent hairs, i-hairs, and block hairs are very specific for the tinea capitis.
Trichoscopy has emerged as an excellent and rapid tool to diagnosis tinea capitis. Many of the trichoscopic findings are highly specific. As mentioned above, trichoscopy should be always paired with a culture if possible so that the precise organism causing tinea capitis can be identified. Trichoscopy is wonderful sometimes but at the end of the visit - we have no idea as to whether the patient’s tinea capitis is from a Trichophyton species or a Microsporum species
Please see “Making the Diagnosis of Tinea Capitis with Trichoscopy”
9. Systemic antifungals (oral medications) are always required for treatment of tinea capitis. Topical antifungal creams and lotions are not the appropriate treatment. Topical shampoos can be used as an adjuvant (add on) to prevent the spread of fungal spores but should not be used alone (as “monotherapy”) for the patient affected by tinea capitis.
One of the biggest mistake that a practitioner can make in treating tinea capitis is prescribing antifungal shampoos and antifungal creams rather than an oral (systemic) antifungal medications to treat tinea capitis. Tinea capitis requires oral medications! Shampoos and topical cream and lotions are far less effective. If we don’t treat tinea capitis properly, we run the risk of permanent hair loss occurring.
10. Most patients have a good outcomes with appropriate treatment although permanent hair loss and permanent scarring can occur.
Most children with tinea capitis get their hair back once the condition is properly treated. Those children with the more inflammatory forms (kerion, pustules, favus) are at greater risk of permanent loss and scarring. For example 10-25% of children with tinea capitis and kerion may have permanent scarring. The condition must be caught early and treated aggressively!
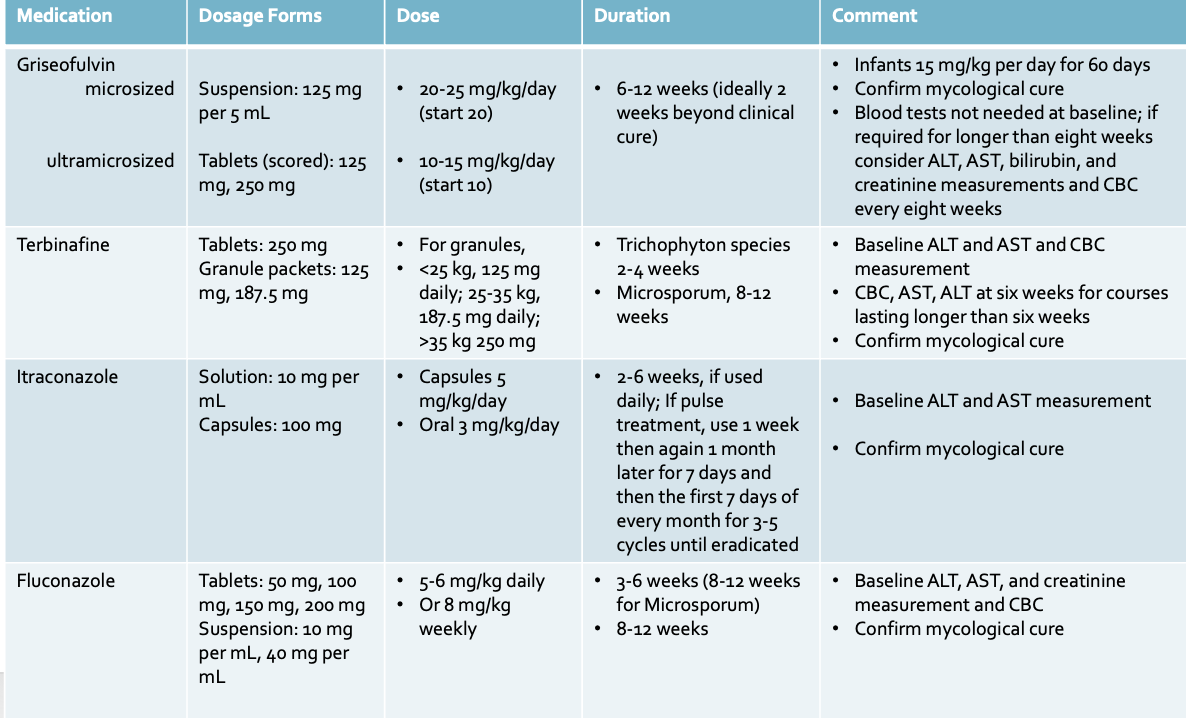
11. Griseofulvin, Terbinafine, Itraconazole and Fluconazole are the main oral medications to treat tinea capitis.
Griseofulvin has long been a first line agent since 1958. It is FDA approved for patients ages 2 and above. Terbinafine is increasingly viewed as another acceptable “first line” especially for tinea capitis due to the Trichophyton species. Terbinafine is formally FDA approved for age 4 and above. Griseofulvin is not available in all countries and its becoming more difficult to obtain in some countries. (It’s not available in Canada for example). Itraconazole and Fluconazole are viewed as “second line” agents in North America. In Europe, Itraconazole is very popular and often used first line for many cases.
12. Griseofulvin is better than terbinafine for treating tinea capitis due to Microsporum canis.
Griseofulvin is a great option for tinea capitis caused by M canis. Terbinafine can also be used to treat M. canis but it’s less than ideal. M canis seems much more refractory to terbinafine. In many countries outside the US, itraconazole is favoured to treat M canis where griseofulvin is not available.
13. Terbinafine is better than griseofulvin for treating tinea capitis due to Trichophyton species (or at minimum it’s at least as good) and requires a shorter time.
It appears that for tinea capitis due to T tonsurans, treatment with terbinafine is more effective than griseofulvin. 4 weeks of terbinafine in some studies is equivalently effective as 8 weeks of griseofulvin.
14. There are no formally FDA approved treatments for treating tinea capitis in infants.
Tinea capitis is not common in infants. However, it can occur in infants. Everything we use to treat infants with tinea capitis is therefore said to be off label. We do use griseofulvin, terbinafine, itraconazole and fluconazole in infants. One must explain to parents that these are off label.
15. Shampoos should never be used alone - but should still be used in the treatment plan.
Antifungal shampoos used to treat dandruff are helpful to reduce fungal spores and should be used by patients 2-7 times per week. The shampoos should be left on the scalp for 5-10 minutes when they are used. Recommended shampoos include selenium sulfide, ciclopirox or ketoconazole. Two times per week is the minimum that a patient should use these shampoos but daily use is also excellent for 3-6 weeks.
16. Family members of patients with tinea capitis should be screened and should use these shampoos too as a preventive measure.
Parents, sisters, brothers, grandparents in the home should be examined properly to see if they too have infection. In the event they do have infection, treatment is needed. However, in the event they do not have infection, use of antifungal shampoos is highly recommended. Recommended shampoos include selenium sulfide, ciclopirox or ketoconazole.
17. Close follow up is needed for patients with tinea capitis - ideally on a monthly basis.
One does not just give some pills to the patient and wish the patient well with treatment course. Close follow up is needed to ensure the infection resolves and to determine when to stop. Some children need standard courses and some need much longer courses. Some children don’t improve with the given medication and other treatments may be needed. One needs to see the patient back and make absolutely certain that the tinea capitis is resolving.
18. Ideally, “mycological cure” should be confirmed at the end of a treatment course - and not just a clinical cure.
At the end of a course of treatment, ideally one should scrape the scalp and see if anything can be cultured. If there is no clinical cure, treatment should be continued another 2-4 weeks and fungal cultures repeated again. Consideration should be given to possibly switch the treatment agent if the disease is not resolving.
If M canis fails griseofulvin treatment, then itraconazole is a good option for the next step. If T tonsurans fails itraconazole treatment, then terbinafine is a good option for the next step. If T tonsurans fails terbinafine treatment then intraconazole,is a good option. Cultures should be done monthly until mycological cure is achieved.
19. For griseofulvin, laboratory evaluation prior to starting the medication is not routinely necessary.
Of course, if there are any known medical concerns or prior lab abnormalities, performing baseline tests might still be a good option. If therapy is continued beyond eight weeks or repeated courses of griseofulvin are needed, liver function tests (AST and ALT) and a complete blood count (and creatinine too) should be obtained to evaluate for hepatic or hematologic toxicity.
20. In contrast to griseofulvin, laboratory evaluation prior to starting terbinafine is necessary.
Baseline labs helpful for CBC, AST and ALT are important to obtain. Repeat labs at month 1 and 3 are helpful if treatment is going to continue beyond 4-6 weeks. The product labeling suggests that prescribers obtain baseline labs.
21. Baseline labs are recommended for fluconazole and itraconazole.
If treatment extends beyond 6 weeks, consider getting repeat labs as well.
22. Griseofulvin is absorbed more effectively when given with fatty food (eg, peanut butter, ice cream). Terbinafine can be taken empty stomach or with food but should not be given with acidic foods.
Terbinafine absorption is reduced when crushed or sprinkled into apple sauce or fruits is given with fatty foods.
23. Children can go to school once they start treatment.
Children do not need to stay away from school once they have taken their first dose. They do not need to wear a hat. They do not need to shave their head.
24. Careful hygiene should also be practiced.
Patients should not share such items as hats, combs, brushes or pillows. Fomites should be disinfected – either boiling or cleaning with disinfectant.
25. In the event a family pet is the source of infection (ie zoophilic tinea species), appropriate evaluation and treatment of the cat or dog by a veterinarian is strongly recommended.
The family pets and sometimes farm animals can be a source of infection. Proper veterinarian consultation is needed in such cases.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.