Is Trichoscopy Really Essential in Diagnosing Hair and Scalp Disorders?
When is Trichoscopy Really Helpful and When is it Optional?
There is a lot of confusion as to when a practitioner should strongly consider using “trichoscopy” (scalp magnification) and when this technique might actually be considered optional. Many patients tell me that their practitioner did not examine their scalp with trichoscopy, and they are therefore concerned that an accurate diagnosis cannot be reached.
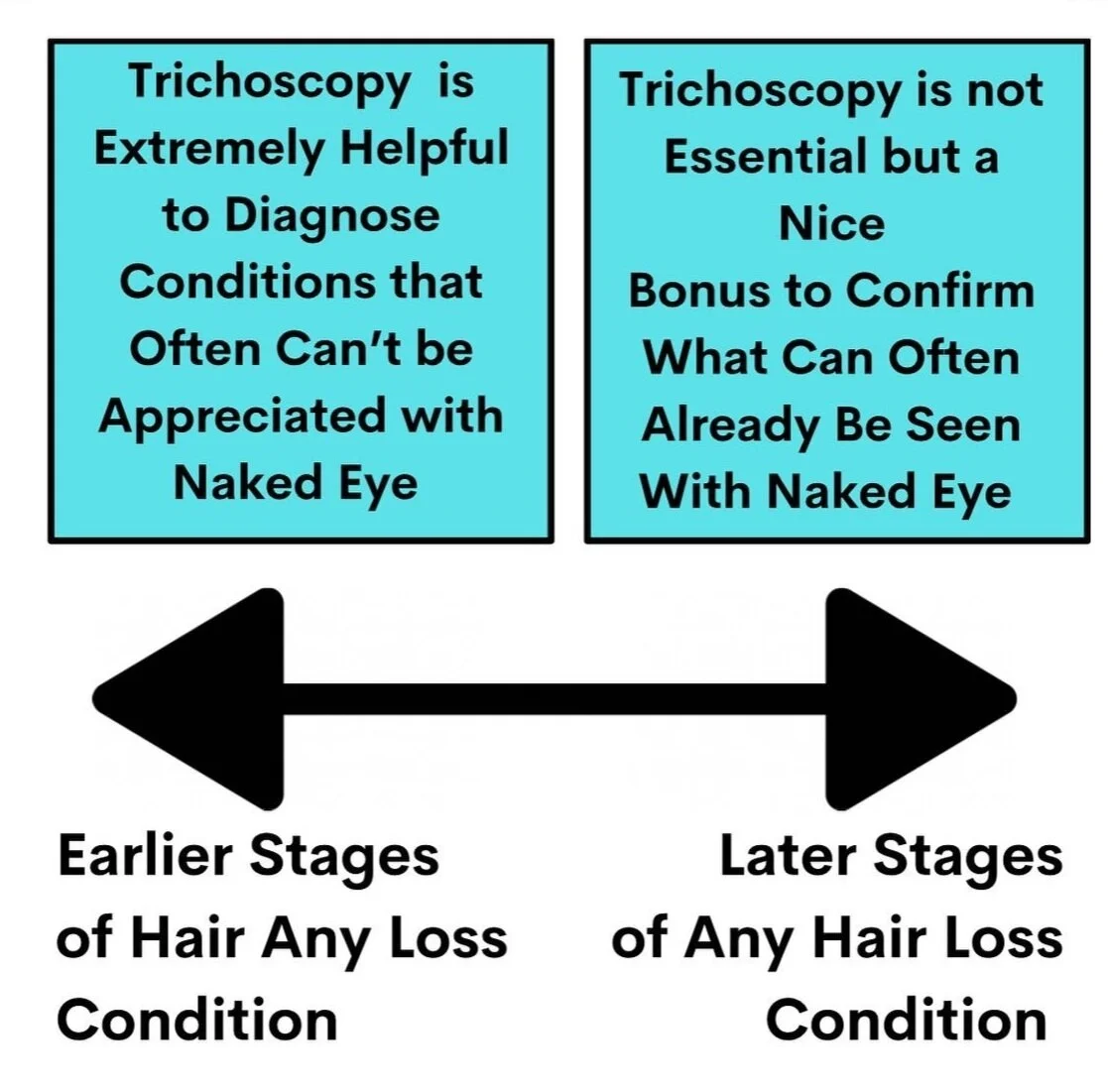
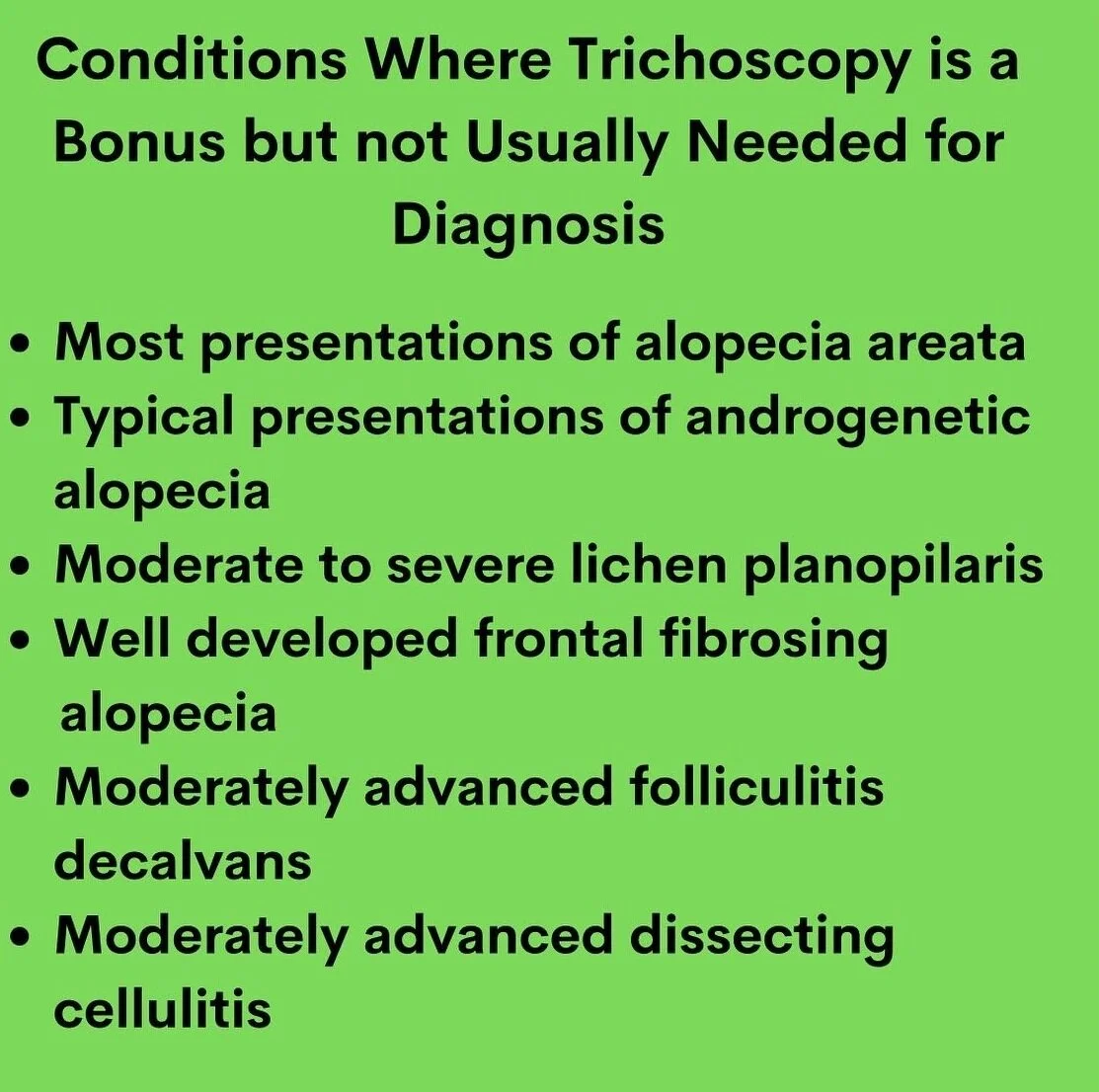
The reality is that many hair loss situations do not absolutely require trichoscopy to make the diagnosis. Trichoscopy may be still helpful to monitor a variety of hair loss conditions over time or to determine the degree of disease activity of the given condition, but trichoscopy may not be actually needed to make the initial formal diagnosis in every single patient with hair loss.
Trichoscopy, however, is very helpful to diagnose hair loss in the early stages and then becomes less and less essential as the stage of the hair progresses. Trichoscopy is often not needed when diagnosing hair loss in the moderate stages of progression or advanced stages of progression. It is of course a nice bonus and simply helps confirm what is already expected from a good standard examination.
In moderate to advanced cases of a given hair loss condition, a simple examination of the scalp by a skilled and knowledgeable practitioner can lead to the diagnosis with a very high degree of certainty, 95 to 99% of the time.
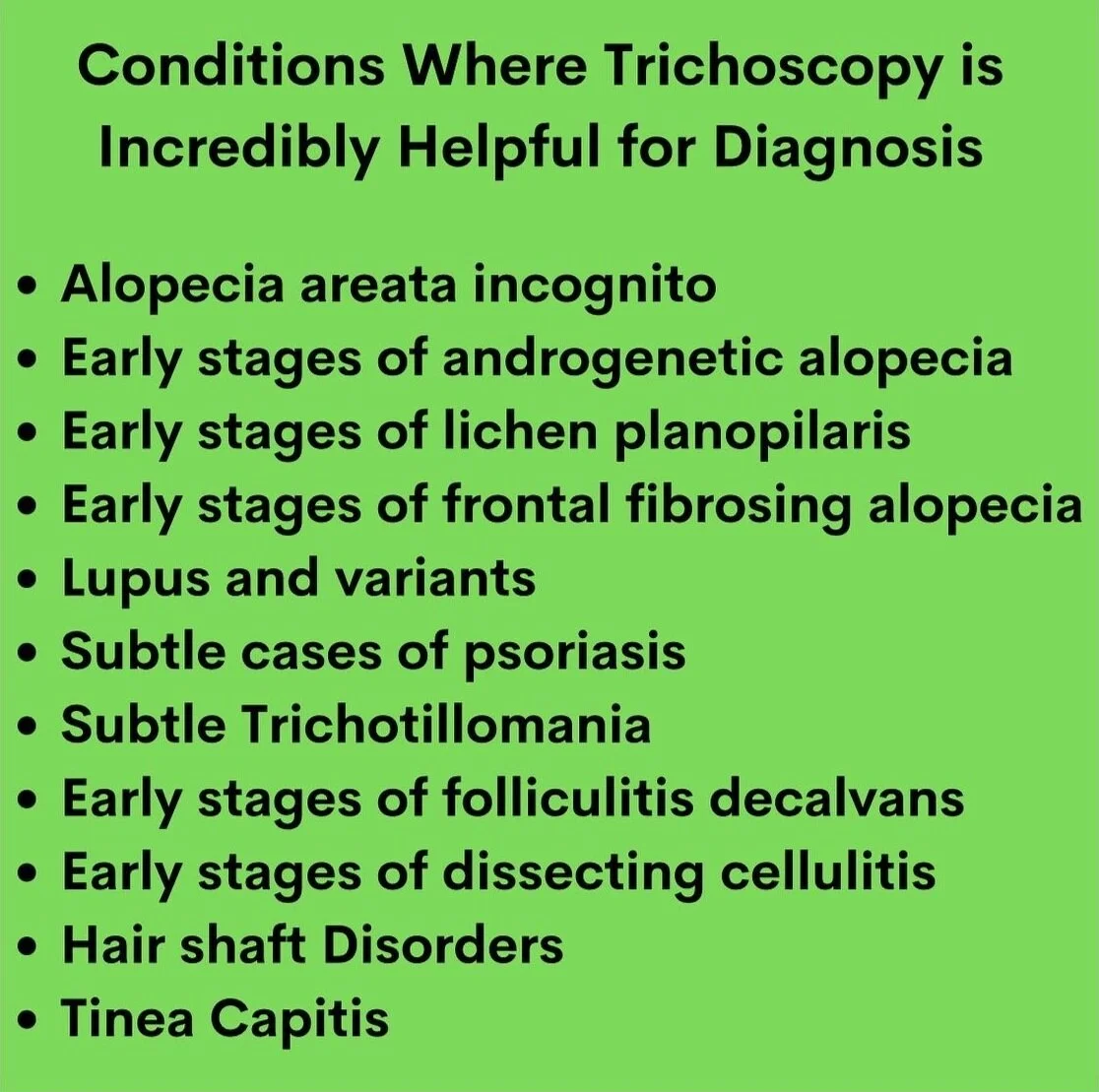
The key point therefore is really the ability of trichoscopy to help make diagnosis in the “very early” stages of the disease. The very early stages of most hair loss conditions helped tremendously through the use of trichoscopy. In fact, many diseases can only be diagnosed properly in the early stages with either a good trichoscopic exam, or a biopsy. Simple examination of the scalp with the naked eye will not lead to the diagnosis because the scalp appears otherwise quite normal when the hair loss condition has only begun.
For example, the early diagnosis of androgenetic hair loss, frontal fibrosing alopecia, lichen planopilaris, dissecting cellulitis and alopecia areata incognito is made possible through the use of trichoscopy. In such cases, the scalp may often appear quite normal at first glance, and a simple examination with a naked eye would lead the clinician to conclude that there’s really nothing particularly wrong with the hair or scalp, and that it looks otherwise normal to him or her. However the use of trichoscopy at that point would allow the well trained practitioner to make the correct diagnosis. In such cases, a biopsy would often not needed as the final diagnosis can often be reached through the use of trichoscopy.
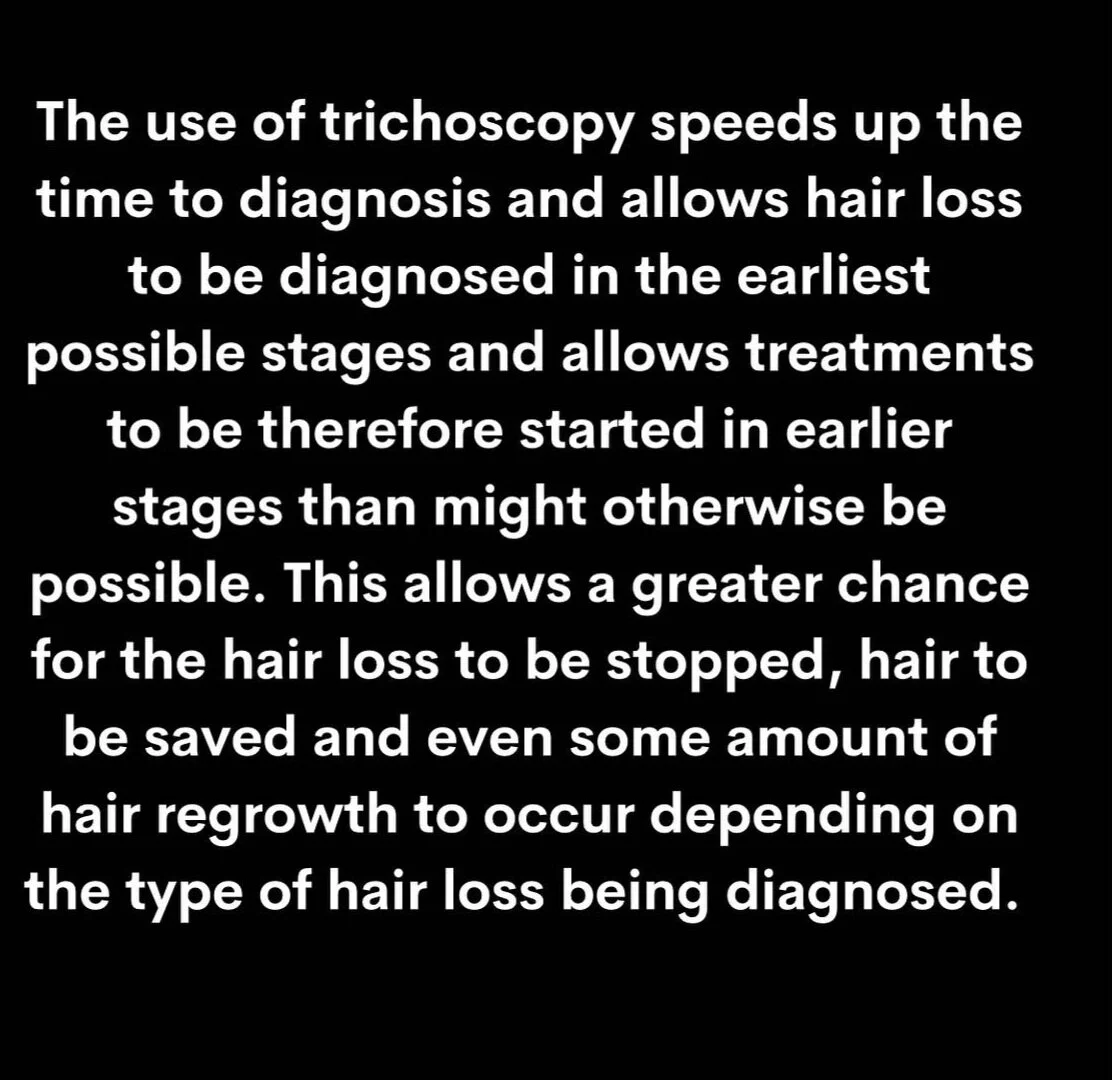
In many disease states, it may take 2, 3 or even four years from the day the disease starts to the time the hair loss condition finally becomes apparent with the naked eye. Many, many patients live with their hair loss for many years before they can convince a doctor, family member, or another practitioner that something is indeed wrong with their hair. The use of trichoscopy speeds up the time to diagnosis and allows hair loss to be diagnosed in the earliest possible stages and allows treatments to be therefore started in earlier stages than might otherwise be possible. This allows a greater chance for the hair loss to be stopped, hair to be saved and even some amount of hair regrowth to occur (depending on the type of hair loss being diagnosed).
There are many situations where trichoscopy is not needed. Patients with moderately advanced, and or genetic hair loss, or alopecia areata, or other modern advanced scarring alopecias do not need trichoscopy to make the initial diagnosis. The diagnosis can be rendered simply by looking at the scalp and sometimes even from across the room. However, one must not forget that the ability to diagnose other hair loss conditions that might be present in the early stages is often not possible with simple examination.
Consider the 32-year-old patient who comes in with a clear diagnosis of androgenetic alopecia hair loss. The patient also has some itching and some burning in the scalp. The clinician might state that it’s quite obvious that androgenetic hair loss is present. That clinician is indeed correct! However, without the use of trichoscopy that clinician will not recognize easily that the patient not only has a androgenetic hair loss, but also has like in planopilaris – a second diagnosis that was still somewhat hiding.
That clinician really should say “ I didn’t need trichoscopy to diagnose the androgenetic alopecia but I did need it to make the diagnosis of the other condition - lichen planopilaris. I completely missed the diagnosis of lichen planopilaris because I did not use trichoscopy.”
We must never forget that many patients have two diagnoses, and sometimes even three or four or five diagnoses. Arriving at one diagnosis should not bring the diagnostic thinking process to a halt. It may be quite easy to diagnose some conditions without trichoscopy. However, once you’re never fool themselves that they have ruled out all their loss conditions if they avoid the use of trichoscopy.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.