Can one see scaling arounds hairs in LPP/FFA without trichoscopy?
Perifollicular Scaling in Lichen Planopilaris & Frontal Fibrosing Alopecia may or may not be easy to see
Lichen planopilaris (LPP) and Frontal Fiborsing Alopecia (FFA) are both types of scarring alopecias. Clinically, patients with FFA and LPP typically give different stories about their hair loss. LPP typcially starts with increased shedding as well as symptoms likely ithcing and burning in the middle of the scalp. Of course, there’s about 50 variations on what patients with LPP report as the first signs and symptoms of the disease so this is not the only way it presents. Patients with FFA, on the other hand, often notice eyebrow or body hair loss month to years ahead of their scalp hair changes. Again, there are many variations on this too. The point is that LPP and FFA are recognized as being clinically distinct. To make matters even more confusing, many patients with FFA have LPP in the middle of the scalp too. The two conditions certainly have their overlap.
Trichoscopy of LPP and FFA are similar - and so is the histology
There’s no doubt that FFA and LPP have their similarities. In fact, when one looks up close with a dermatoscope (trichoscopy), it can be difficult to tell LPP and FFA apart. They can look the same up close. One needs to stand back and think about where the patient is losing hair to make a decision whether the patient has a) FFA or b) LPP or c) both FFA and LPP. The main point here is that dermatoscopic image of classic LPP and FFA can be similar and that includes perifollicular erythema, (redness around hairs) and perifollicular scale (scale around hairs) and many single hairs (rather than hairs in groups of 2 and 3.
The histology of LPP and FFA is also the same. If you give a dermatopathology a biopsy fo FFA and LPP to examine under the microscopy they look the same. One can’t tell them apart. Again, the actual diagnosis of LPP and FFA comes from examining the scalp and the trichoscopic findings and then stepping back and asking “so does this best fit with LPP of FFA?” If only the frontal hairline, eyebrows, body hair involved without any involvement in the mid scalp and crown, in probably fits best with FFA. If the findings are localized more to the mid scalp and crown, the diagnosis may be more likely to be LPP
Do we need a dermatoscope to diagnose LPP and FFA? Are these findings alway present?
Redness and scaling around hairs are imprortant signs of FFA and LPP. They can sometimes be seen simply by looking at the scalp - but not always. Typically, if one can see scale around many hairs without magnification or without a dermatoscope, it’s like the patient has very active disease.
A dermatoscope or trichoscope really enhances the ability to detect these findings of LPP and FFA. In my opinion, trichoscopy can greatly enhancee the ability to diagnose FFA and LPP. The classic scaling, redness and changes around hairs are not always seen from simple visual inspection.
EXAMPLES
Here are some example of perifollicular scale in LPP and FFA.
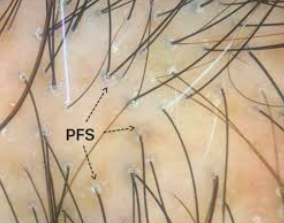
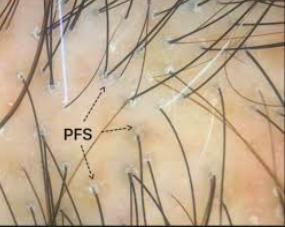
Perifolliclar scale in LPP. This case is subtle and would not be possible to identify without a dermatoscope.
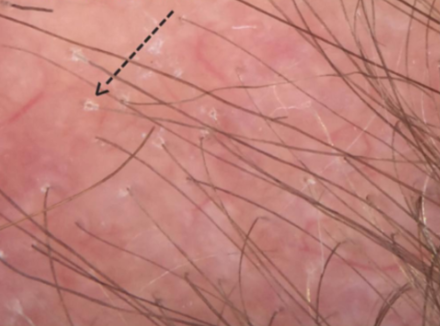
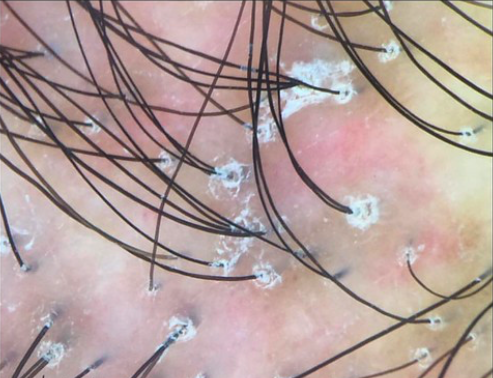
Perifollicular redness in FFA. This redness is seen even without a dermatoscope.
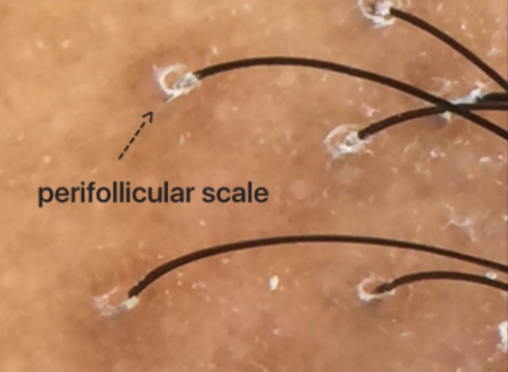
Perifollicular scale in FFA. The scale in this case is subtle and would only be seen with a dermatoscope. The diagnosis however might still be possible to make by an astute clinician without a dermatoscope. But there is not doubt a dermatoscope makes it easier and enhances the confidence in making the diagnosis. Such confidence can even help patients avoid the need for a biopsy in some cases.
Perfiollicular scale in LPP; This scale would be visible visually by simply looking at the scalp as well as with a dermatoscope.
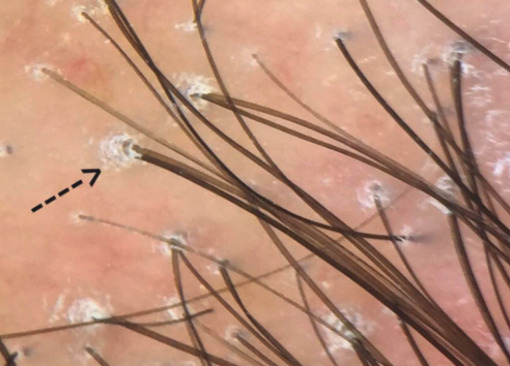
Perifollicular scale in FFA. The scale here is subtle and would only be seen with a trichoscopic examination.
Perifollicular scale in LPP. The scale here is thick and intensity of redness is quite high. This scale would even be seen without a dermatoscope/trichoscope.
Perifollicular scale in LPP. The scale here is quite thick and is visible simply by examining the scalp.
Perifollicular scale in LPP. The scale here is subtle and only a proper dermatoscopic examination would pick this up.
Perifollicular scale in LPP. The scale here is thick and visible even without a dermatoscope.
Conclusion
A dermatoscope greatly enhances the ability to diagnosis lichen planopilaris and frontal fibrosing alopecia. In extremely active forms, the redness and scale may be visible even without a dermatoscopic examination. By definition, these patients have active disease and are at risk for further loss.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.