The "Vitamin D Paradox": What you need to know before giving more and more
Monitoring Vitamin D Levels in Black Patients: Knowing More About Vitamin D Might Cause Us All to Maybe Give a Bit Less.
While studies show a correlation of serum 25(OH)D levels (25 hydroxy-vitamin D) to bone mineral density and fracture risk in White and Mexican-Americans, serum 25(OH)D levels do not correlate with the same health outcomes in some other populations, particularly Black Americans. African Americans have a lower total serum 25-hydroxy-vitamin D but superior bone health. This has been referred to as the “vitamin D paradox”. Let’s explore what this means and why you need to understand this concept to avoid unintentionally causing more harm than good.
Blood Tests for 25 hydroxy-vitamin D: The Blood Lab Test For Which Many Decisions Get Made
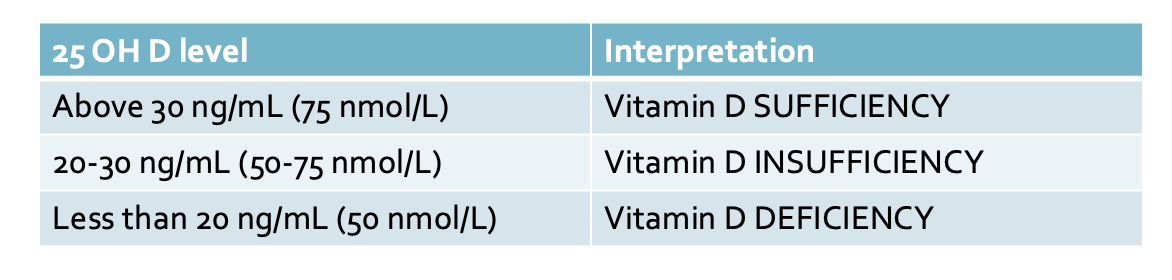
25 hydroxy-vitamin D has been used as the key blood test to determine vitamin D status of the patient. In most clinics and hospitals of the world, health care practitioners keep a pretty simple rule for vitamin D: If levels are less than 30 ng/mL but above 20, we tell the patient that they have vitamin D insufficiency and to take vitamin D. If patients have levels less than 20 ng/mL we tell the patient they are vitamin D deficient and to take more vitamin D.
The Institute of Medicine (IOM) has even different cut offs - a bit lower actually. They have stated that levels of serum 25(OH)D were sufficient when in the range of 20 ng/mL- 50 ng/mL; low when less than 20 ng/mL; and deficient when below 12 ng/mL
Research evidence has been accumulating over the past decade that basing decisions on vitamin D supplementation in black patients simply based on blood test measurement of 25 hydroxy-vitamin D levels might not be such a great idea after all.
The exact details of how best to measure vitamin D is still being worked out by researchers - including how much vitamin D we all should really be getting each day.
Why do black patients have lower 25 hydroxy-vitamin D levels?
There are likely many reasons for lower 25 hydroxy-vitamin D levels in black patients than white patients. It has long been known that there is reduced absorption of UV light in the melanin-rich skin of black individuals and therefore a reduced ability to generate vitamin D.
Genetic factors are also thought to play a role so it is far more complex than the ability of the skin to make vitamin D.
Do lower vitamin D levels translate into worse health consequences for black patients?
Vitamin D is known to play a key role in bone health. Much to the surprise of researchers, many black patients have better bone health than white patients despite lower levels of 25 hydroxy-vitamin D. In 2007, Kalkwarf et al showed that the bone mass of black patients was higher than white patients in early childhood and then increased further during the teenage years. This all seems to translate into better bone health and reduced rates of fractures. In 2005, Barrett et al showed that the fracture rate in elderly African American women is only half that of white American women.
The VDBP
The vitamin D binding protein (VDBP) is the somewhat new protein of interest - at least to some researchers. It’s not that the protein is all that new - simply that its role in understanding how we should be measuring and thinking about vitamin D status appears to be changing.
To understand the role of vitamin D binding protein, we need to review the vitamin D pathway. Vitamin D (also known as cholecalciferol) gets made in the skin after UVB radiation hits the skin. The cholecalciferol then gets converted to 25 hydroxy-vitamin D (25OHD) by the liver. 25 OHD is an inactive form of vitamin D. The 25 hydroxyvitamin D then makes its way to the kidney and the kidney converts the 25 hydroxy vitamin D to 1,25 dihydroxyvitamin D. Other cells and tissues can also convert 25OHD to active 1,25 dihydroxy vitamin D. Active 1,25(OH)2 vitamin D exerts its effects inside cells following binding to the vitamin D receptor.
The thing that tends to be forgotten in this classic story is that serum 25(OH)D is transported in blood attached to a protein - and that protein is the vitamin D binding protein (VDBP). Most serum 25OHD is believed to be transported by VDBP (88%) or albumin (12%). So there are really two forms of 25 hydroxy-vitamin D - 1) the so called “free” 25 hydroxy-vitamin D which is not bound to VDBP and 2) the “bound” 25 hydroxy-vitamin D which is bound to VDBP. It appears that VDBP controls how much “free” 25 hydroxy vitamin D the body gets to see.
It’s free 25 hydroxyvitamin D that seems to be at least somewhat relevant to how we measure vitaminD.
The Famous Powe et al 2013 New England Journal of Medicine Study
If you don’t know about the 2013 study by Powe et al you probably should - especially if you’ve read this far in the article!
Powe indirectly estimated free 25(OH)D and total the 25(OH)D. Their estimates suggested that although serum total 25(OH)D was lower in black Americans, their bioavailable 25(OH)D was the same as white Americans.
Specifically, the data showed that the mean levels of both total 25-hydroxyvitamin D and vitamin D–binding protein were lower in blacks than in whites (total 25-hydroxyvitamin D, 15.6 ng per milliliter vs. 25.8 ng per milliliter, P<0.001; vitamin D–binding protein, 168 μg per milliliter vs. 337 μg per milliliter, P<0.001). Genetic polymorphisms independently appeared to explain 79.4% and 9.9% of the variation in levels of vitamin D–binding protein and total 25-hydroxyvitamin D, respectively. The authors showed that bone mineral density was higher in blacks than in whites. Levels of parathyroid hormone increased with decreasing levels of both total and bioavailable 25-hydroxyvitamin D (P<0.001 for both relationships). Among homozygous participants, blacks and whites had similar levels of bioavailable 25-hydroxyvitamin D overall (2.9±0.1 ng per milliliter and 3.1±0.1 ng per milliliter, respectively; P=0.71) and within quintiles of parathyroid hormone concentration.
All in all, Powe et al estimated that although serum total 25(OH)D was lower in black Americans, the “bioavailable 25(OH)D” was the same as white Americans. The authors also showed that genetic polymorphisms may result in lower VDBP in African Americans. Dr Powe’s group has subsequently conducted alot of studies looking at the ability of different VDBP polymorphisms to sop up vitamin D and these may affect the actions of vitamin D.
The Post Powe Era: Studies 2013-2022
Studies in the years after the Powe study supported the notion that current 25 hydroxy-vitamin D blood tests may incorrectly lead many African Americans to be considered vitamin D deficient when in fact they might not be.
In 2015, Aloia et al also reported that although the total serum 25(OH)D is lower in black than white Americans, free 25(OH)D is almost identical.
Several researchers have since suggested that there is no one factor alone that could fully explain the vitamin D paradox in Black Americans. Relevant issues include adiposity, skin pigmentation, vitamin D binding protein polymorphisms, and genetics. These factors all seem to contribute to differences in 25(OH)D levels in Black vs. White Americans.
The Dec 2017 Meeting “The Vitamin D Paradox in Black Americans: A Systems-based Approach to Investigating Clinical Practice, Research, and Public Health.”
In Dec 2017, several organizations co-sponsored an expert panel meeting to further address these vitamin D issues. Six panelists, each of whom were considered experts in the vitamin D paradox, were invited to the meeting. A summary of the panelists’ views is available free online through a post meeting summary paper.
Dr Hoofnagle from the University of Washington pointed out that 25(OH)D levels appeared to decrease as skin color darkened when comparing White, Chinese, Hispanic, and Black Americans.
Dr Hoofnagle also pointed out data from a trial known as the multiethnic study of atherosclerosis (MESA). The MESA trial supported the accepted finding that the fracture rate for Black Americans was lower than that for White Americans. However, much to the surprise of many, the data showed that higher serum levels of 25(OH)D were associated with lower cardiovascular (CVD) risk in White and Chinese Americans, while higher serum levels of 25(OH)D were associated with a slightly higher risk of CVD in Black and Hispanic Americans.
Furthermore, Dr Hoofnagle reminded the panel that a study known as the National Health and Nutrition Examination Survey (NHANES) study showed that higher levels of 25(OH)D were associated with lower all-cause mortality in White Americans but less strongly associated with all-cause mortality in Black Americans.
Dr. Aloia from the Stony Brook School of Medicine reminded the panel that higher levels of vitamin D presents hazards for Black Americans, resulting in more falls and fractures. Furthermore, lower vitamin D levels under 12 ng/mL (30 nmol/L) increase the risk of rickets and osteomalacia.
Dr Shapses from Rutgers University reminded the panel that obesity is also an important factor and may have an important role in understanding 25 OH D levels. Dr Shapses pointed out that Adipose tissue acts as a depot for vitamin D. Weight loss leads to higher 25 OHD levels and also better responses to vitamin D supplementation. More studies are needed to determine if certain dosing is more appropriate for different body mass indices. Many authors do feel that obesity plays a role in the vitamin D paradox given that rates of obesity in the US are higher in black individuals than white.
The paper is worth reading for those looking to better understand the vitamin D paradox. The panelists propose that 25 OH D is not the best test for measuring vitamin D status but rather is a good biomarker of exposure (through sunlight and diet). The panelists seemed to agree that the 25(OH)D test is far from perfect but is currently the best tool available for assessing vitamin D status.
What I found interesting in the paper is that the panelists pointed out that safe upper limits of vitamin D intake are very high for white patients but not necessarily for black patients. For example, it was noted by panelists that the Endocrine Society recommends 10,000 IU/day as an upper safe limit in the general population, while the IOM recommends 4000 IU/day as an upper safe limit in the general population. However, in black patients, doses as low as 2000 IU/day can increase the risk of falls and fractures in Black Americans.
What levels of 25 hydroxy-vitamin D should we be aiming for? And is there a better marker for vitamin D status?
It seems that there is still some uncertainty and unknowns when it comes to how best to assess vitamin D status in differences races.
It’s not clear if we should be using some other measure of vitamin D status like free 25(OH)D. Some have suggested using the ratio of 25(OH)D levels to 24,25(OH)2D levels. Although 25(OH)D levels and 24,25(OH)2D levels are higher in White Americans compared to Black Americans, the ratio of 25(OH)D to 24,25(OH)2D was the same in both groups. These issues merit further study.
Some researchers have suggested for now we need to be careful about saying that 25(OH)D levels less than 30 nm/mL are of significant concern. Again this needs more study. Some have suggested that levels should probably be well above 12.5 ng/mL. It does seem that at very low levels of 25(OH)D (<12.5 ng/mL), African Americans may be more susceptible to develop rickets and osteomalacia.
It seems that 25 OH D levels are only partly explained by skin color and how much vitamin D gets made in the skin. There are clearly other factors and most researchers feel that there are important genetic differences that affect 25 OH D levels.
The vitamin D paradox in Black Americans is an important and relevant public health issue that needs more study. It does not appear that there are the same skeletal benefits from high doses of vitamin D supplementation in Black Americans compared to white Americans. Specifically, a randomized, double-blind, placebo controlled, parallel-group study by Aloia et al in 2005 was done to evaluate the efficacy of vitamin D3 in the prevention of bone loss in 208 black postmenopausal women. The study results showed no change in bone mineral density (BMD) with vitamin D supplementation (i.e., 800 International Unit or IU for the first 2 years and 2000 IU for the last year of the trial)
Finally, not only isn’t there the same benefit from vitamin D supplementation in black patients but there may in fact be important skeletal risks of maintaining high serum levels of 25(OH)D in this population. This all needs further study
REFERENCE
Aloia J et al. Free 25(OH)D and the Vitamin D Paradox in African Americans. J Clin Endocrinol Metab. 2015 Sep; 100(9): 3356–3363.
Aloia JF, et al. A randomized controlled trial of vitamin D3 supplementation in African American women. Arch Intern Med. 2005;165(14):1618–23
Barrett-Connor E, Siris ES, Wehren LE, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20(2):185–194
Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin, D. and Calcium. In: Ross AC, et al., editors. The national academies collection: reports funded by National Institutes of Health, in Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): National Academies Press (US) National Academy of Sciences; 2011.
Kalkwarf HJ, Zemel BS, Gilsanz V, et al. The bone mineral density in childhood study: bone mineral content and density according to age, sex, and race. J Clin Endocrinol Metab. 2007;92(6):2087–2099
Powe CE, Evans MK, Wenger J, et al. Vitamin D-binding protein and vitamin D status of black Americans and white Americans. N Engl J Med. 2013;369(21):1991–2000.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.