Is there an Increased Risk of Diabetes in Patients with Central Centrifugal Cicatricial Alopecia?
Central Centrifugal Cicatricial Alopecia: Risk of Diabetes
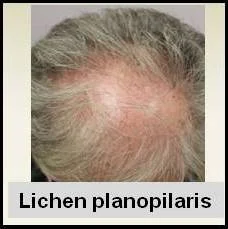
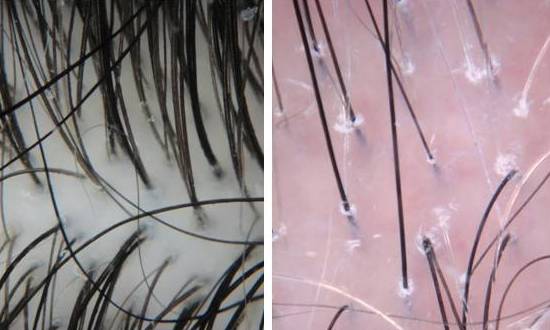
Hair Loss in Patient with CCCA Central centrifugal cicatricial alopecia or "CCCA" is the most common cause of scarring alopecia. Scarring alopecia refers to hair loss conditions where scarring develops around the hair follicles and leads to permanent hair loss. "CCCA" predominantly affects black women where up to 30 percent of women are affected.
Last year, an interesting paper was published in the journal Archives of Dermatology by researchers at the Cleveland Clinic. The authors handed out a survey to African American women at 2 churches as well to African American women attending a health fair. The survey allowed the collection of information about basic medical history as well as information about hair styling practices. In total, 326 women participated in the study.
8% of Women with CCCA Had Diabetes
About 8 percent of women in the study had type 2 diabetes. However, the researchers found an increased prevalance of diabetes in women with centrifugal cicatricial alopecia. Women with CCCA were more likely to used braids and weaves than women without CCCA. The vast majority of women who participated in the study used releaxers. However it did not appear that the use of relaxers was associated with the development of CCCA in this particular study.
Although there are many limitations to this study, I particularly like the study. First, it reminds us the CCCA is a common reason for hair loss in black women. Second, this study provides new information that CCCA may be asociated with an increased risk of diabetes. Although more research is needed to confirm this, these findings open many new avenues for research.
Reference
Kyei et al. Medical and Environmental Risk Factors For the Development of Central Centrifugal Cicatricial Alopecia. Arch Dermatol 2011; 147: 909-14
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.