Lichen planopilairis (LPP) is an autoimmune scarring hair loss condition that affected adults between 35 and 60. Patients develop hair loss but also symptoms of itching, burning and pain. The early stages of LPP are accompanied by increased shedding as well. Aggressive and early treatment of LPP is required to stop the hair loss.
What treatments are most effective?
Treatment that block inflammation are most effective. But not any anti-inflammatory can be used. For example, aspirin and ibuprofen don't help. Rather anti-inflammatories belonging to a group of medications known as immunosuppressive and immunomodulatory drugs work best. This includes:
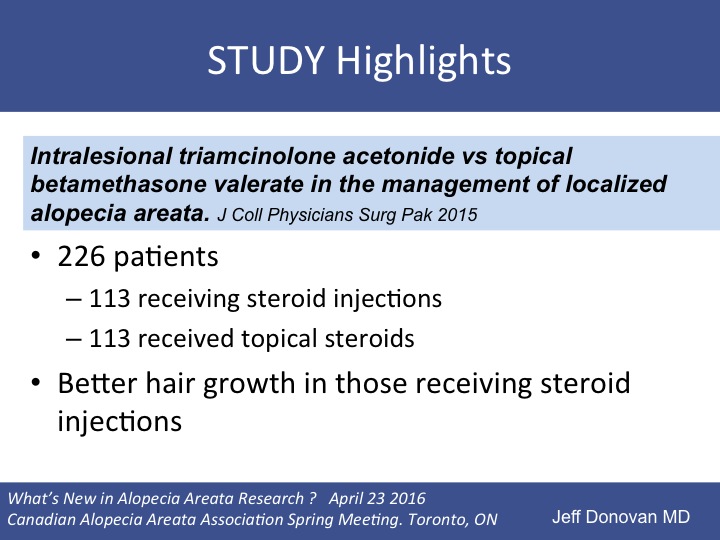
1. Topical steroids (mid to strong potency) and steroid injections
2. Topical tacrolimus (Protopic) and topical pimecrolimus (Elidel)
3. Oral hydroxychloroquine (Plaquenil and generics)
4. Oral tetracyclines (doxycycline, tetracyline, minocycline)
5. Oral cyclosporine (Neoral, prograft, Sandimmune)
6. Oral mycophenolate mofetil (Cellcept, Myfortic)
7. Oral predisone (mainly for flares and early bridging treatment, not long term)
These 7 treatments have the best published evidence for assistance with lichen planopilaris. Any other treatment has less evidence.
Conclusion
Whenever a patient tells me they have tried treatments for lichen planopilaris and it didn't work, I want to know two things. First, I want to know if they truly have lichen planopilaris as there are many many mimickers. Biopsies can be wrong ... yes! and yes! Conditions like pseudopelade of Brocq can mimic LPP and so can a few other scarring alopecias (discoid lupus and folliculitis decalvans). The second thing I want to know is what treatments the patient has tried. I've heard countless treatments - perhaps well over 60 to date. Being on treatment does not count unless it's a potentially beneficial one.
References
Lichen planopilaris: update on pathogenesis and treatment.
Baibergenova A, Donovan J. Skinmed. 2013 May-Jun;11(3):161-5. Review
Efficacy of oral retinoids in treatment-resistant lichen planopilaris.
Spano F, Donovan JC. J Am Acad Dermatol. 2014 Nov;71(5):1016-8. doi: 10.1016/j.jaad.2014.06.013. Epub 2014 Oct 15.
Lichen planopilaris following whole brain irradiation.
Perrin AJ, Donovan JC. Int J Dermatol. 2014 Oct;53(10):e468-70. doi: 10.1111/ijd.12576. Epub 2014 Jun 5.
Scalp trauma: a risk factor for lichen planopilaris?
Montpellier RA, Donovan JC. J Cutan Med Surg. 2014 May-Jun;18(3):214-6.
Lichen planopilaris after hair transplantation: report of 17 cases.
Donovan J. Dermatol Surg. 2012 Dec;38(12):1998-2004.