A recent question, submitted by a visitor to www.donovanmedical.com
I have a teenage daughter who was diagnosed with folliculitus decalvans by one dermatologist and dissecting cellulitus by another. The first time she went bald her hair grew back. This episode is much more severe with a large region that is progressively getting bald. She is very aware of the loss and obviously upset. She is on erythromycin and topical steroid. Is it worth seeing an immunologist? Previous biopsies show negative results for staph. I don’t know what else to do.
ANSWER FROM DR. DONOVAN
Thanks for the very interesting question. Because I don’t know much about your daughter’s specific history, and haven’t examined her scalp, I can only make a few general comments. But I hope they are helpful to you!
1. Folliculitis decalvans and dissecting cellulitis are not very common in children and teenagers.
2. Dissecting cellulitis is more common in males, especially Black or Hispanic men. It can occur in females. It typically causes boggy tender areas on the scalp that sometimes leak pus. Hair loss occurs in these areas and can lead to permanent hair loss. Hair growth occurs if treated early, otherwise leads to permanent hair loss. Patients rarely have bad acne, and cysts under the armpits and in the groin.
KEY QUESTIONS TO CONSIDER FOR DISSECTING CELLULITIS DIAGNOSIS:
Is your daughter experiencing discharge of pus (often with odor) in the areas of hair loss?
Are the areas tender?
Are the areas boggy?
(Individuals with Dissecting Cellulitis often answer yes)
3. Folliculitis decalvans also causes permanent hair loss and begins with itchy bumps often in the crown. Swabs from the scalp may grow bacteria (like the Staphylococcus you mentioned) but not always.
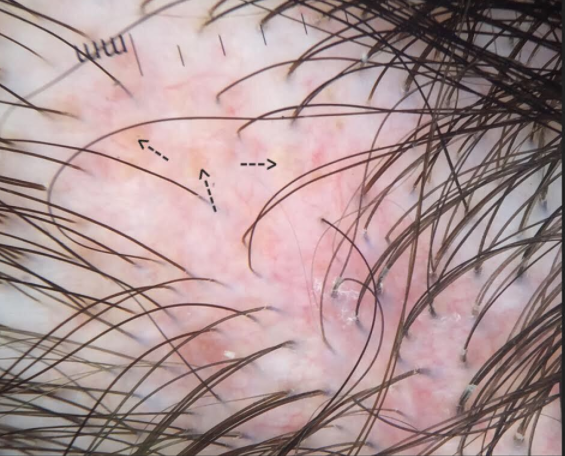
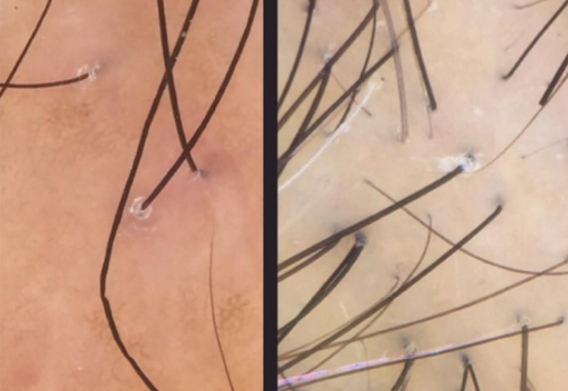
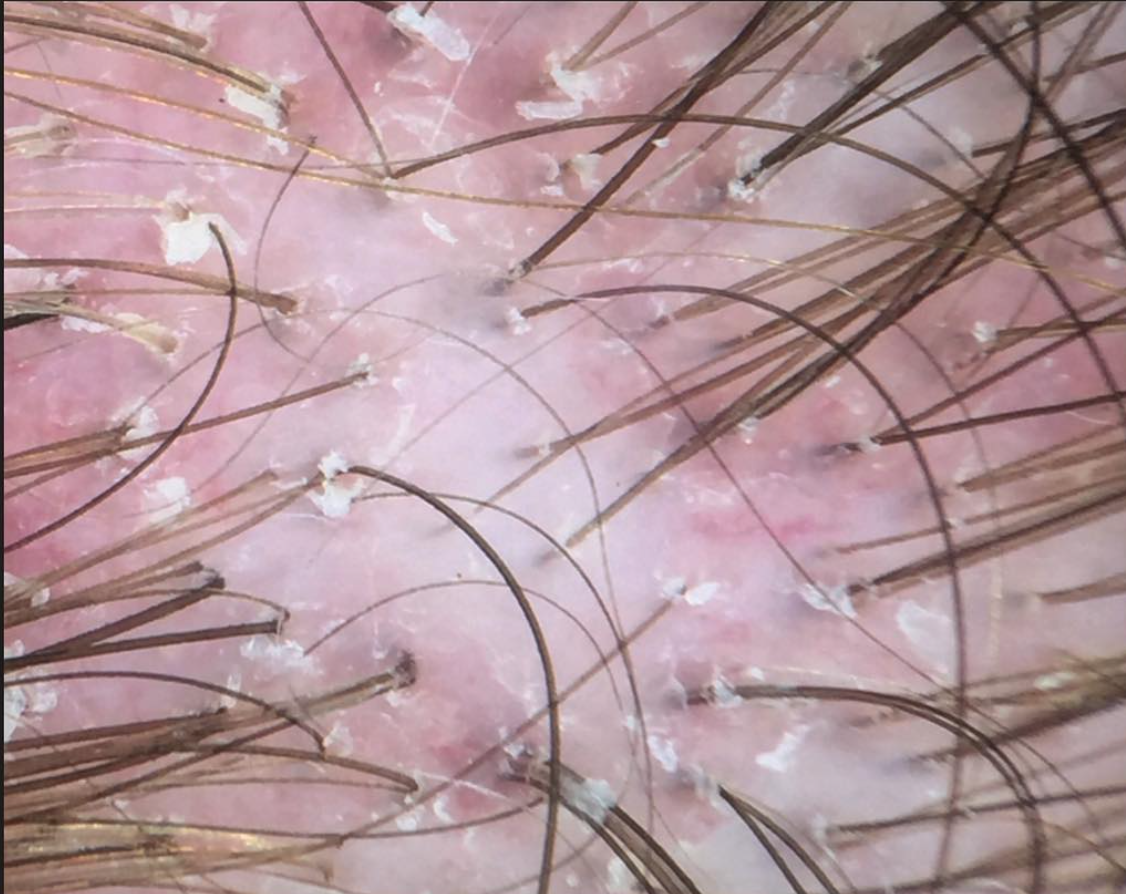
Folliculitis decalvans
KEY QUESTIONS TO CONSIDER FOR FOLLICULITIS DIAGNOSIS :
Does your daughter have itching red bumps in the scalp?
Does she ever wake up with blood on the pillow?
(Individuals with folliculitis decalvans often answer yes)
Why is the diagnosis important?
The diagnosis is important because treatments are different for folliculitis decalvans compared to dissecting cellulitis. For folliculitis decalvans treatment includes medications such as antibiotics, dapsone and retinoids. For dissecting cellulitis, treatments include retinoid medications, possibly antibiotics and sometimes even injectable medications known as TNF inhibitors.
Other considerations
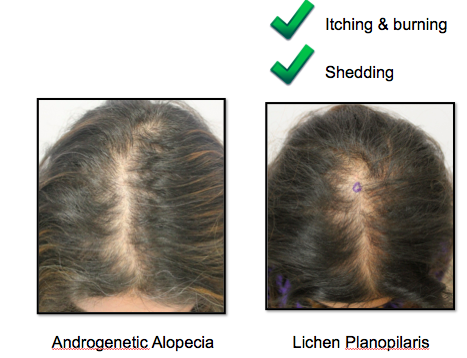
Episodes of hair loss in teenagers where baldness occurs and then grows back is quite typical of alopecia areata – or specifically a form known as alopecia totalis. Of course without seeing your daughter, I can't determine the cause of her hair loss- but alopecia areata is one of the few scalp conditions that leads to complete baldness followed by regrowth. Did your daugther experience "complete" scalp baldness for a period of time? Alopecia areata is an autoimmune disease – it’s common in the population and affects about 2 % of the world. Seeing an immunologist for alopecia areata is not necessary, nor folliculitis decalvans or dissecting cellutlis.
Dermatologists are among the best trained physicians to address complex hair loss issues. If you're not sure of what diagnosis your daughter has or question the diagnosis that has been given, be sure to address these issues with the dermatologist. All in all, if the diagnosis remains uncertain, a scalp biopsy might be considered and sent to a specially trained dermatopathologist with expertise in evaluating scalp biopsies.
I hope this information offer help.
- Dr Jeff Donovan