Testosterone Replacement in Androgen Deficient Women: What are the effects on the hair?
Testosterone Replacement for Women with Androgen Deficiency: Good or Bad for Hair?
Androgens can both help hair growth and block hair from growing. In males, androgens help hair on the beard grow thicker. In genetically susceptible males, it’s clear that androgens cause balding in males that have the right set of genes.
In women, androgens can also contribute to hair loss. Women with hormonal issues that give high androgens such as polycystic ovarian syndrome (PCOS) and congenital adrenal hyperplasia (CAH), higher than normall androgen drive the balding process. Furthermore, reducing the levels of androgens with drugs such as spironolactone can help slow or stop hair loss.
Does taking androgens cause hair loss in women who are very low in androgens?
Supplementing with androgens (i.e. anabolic steroids and testosterone) can cause hair loss in some men and women. For example, men who take androgens for body building can develop hair loss if they have the right balding genes to begin with.
Androgen deficiency can occur in women and often leads to changes in mental health, loss of libido, reduced bone mass - among other symptoms. A proper evaluation is needed to determine the precise reason for the androgen deficiency as pathological processes affecting the ovary, hypothalamus and pituitary gland can all affect circulating androgen levels.
An important question is whether taking androgens can cause hair loss if women have androgen deficiency to begin with. If women with androgen deficiency are given androgen replacement…. will their hair become even worse? A 2012 study by Glasner and colleagues set out to answer that very question
TESTOSTERONE REPLACEMENT: EFFECTS ON 285 ANDROGEN DEFICIENT WOMEN
The authors studied a total of 285 women with androgen deficiency who were treated with androgen replacement therapy for at least one year. The women in this study had used subcutaneous testosterone implants.
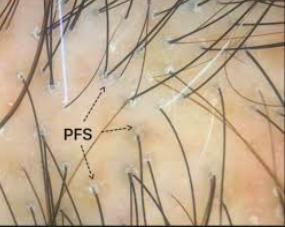
About one quarter of women (27%) had hair thinning prior to starting treatment. Women with thinning hair had the lowest levels of testosterone to begin with compared to women who did not mention problems with their hair.
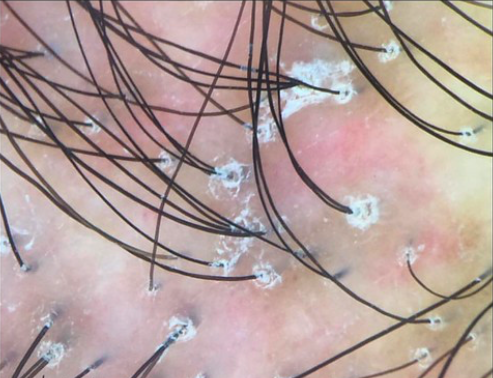
Interestingly, a majority of these women (63%) actually went on to have some amount of hair regrowth on testosterone treatment. Some women did not have any improvement of their hair on therapy - and these women tended to be of higher body weight (higher BMI).
An important finding of the study was that none of the 285 women reported hair loss on the testosterone replacement. The treatment was otherwise well tolerated although 92 % did develop increased facial hair.
Conclusion
This is an important study and one that I refer to often in my practice. It is appropriate for women who are androgen deficiency and have symptoms and signs that seem to be related to the androgen deficiency to begin an open discussion about androgen replacement with their doctors. This may not be appropriate for everyone and when to offer androgen replacement (and when not to) …. is still a bit controversial. Women with low libido and low blood androgen levels may be the best candidates for replacement based on current evidence. These are important discussions for patients to have with their endocrinologists, gynecologists or primary care physicians. There is no good evidence that androgen replacement for women who are truly deficient compromises the hair and cause hair loss. In fact, it may help many of these women with their hair.
Reference
Glaser RL et al Improvement in scalp hair growth in androgen-deficient women treated with testosterone: a questionnaire study. British Journal of Dermatology 2012. READ ARTICLE
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.